Case Report

Ileocolic Intususception due to Non –Hodgkin's Lymphoma –A Rare Presentation in Adults- A Case Report
1Narayanarao Teppela, 2Suvarchala Akkidas, 3Parvathi Teppela, 4Srinivas Abburi
- 1.Dr.T.Narayana Rao, M.S., FICS,FACS.Professor of Surgery,Andhra Medical College Chief surgeon, King George HospitalVisakhaptnam.
- Saturday, July 27, 2013
- Monday, September 02, 2013
- Thursday, November 14, 2013
This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/3.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Introduction
The first report of intussusception was made in 1674 by Barbette of Amsterdam. In1871 Sir Jonathan Hutchinson was the first to successfully operate on a child with intussusception. Overall the male-to-female ratio is approximately 3:1.The pathogenesis of idiopathic intussusception is not well established. It is believed to be secondary to an imbalance in the longitudinal forces along the intestinal wall. In enteroenteral intussusception this imbalance can be caused by a mass acting as a lead point or by a disorganized pattern of peristalsis (eg, an ileus in the postoperative period). In approximately 2-12% of children with intussusception a surgical lead point is found. Occurrence of surgical lead points increases with age and indicates that the probability of non operative reduction is highly unlikely. Adult intussusception represents 5% of all intussusceptions and 1% to 5% of all cases of intestinal obstruction in adults. In the adult population approximately 40% of them are caused by primary or secondary malignant neoplasms.
Case Presentation
A 30 years female patient brought to the hospital with pain abdomen since one week. Ultrasound abdomen suggestive of ileo-caecal intussusception. CECT abdomen done which shows ileo-caecal intussusception Laparoscopic assisted reduction of intussueption and resection of ileum-end to end anastomosis done along with appendicectomy . Tumor shows features of Non-hodgkins lymphoma-follicular variant.
Conclusions
Adult intussusception remains a rare cause of persistent or intermittent chronic abdominal pain. In contrast to its paediatric counterpart the treatment almost always is surgical.
Key Words
Intussusception, Lymphoma, Laparoscopy.
Introduction
The first report of intussusception was made in 1674 by Barbette of Amsterdam. In1871 Sir Jonathan Hutchinson was the first to successfully operate on a child with intussusception. A wide geographic variation in the incidence of intussusception among countries makes difficult to determining the true prevalence of the disease. Overall the male-to-female ratio is approximately 3:1. In patients older than 4 years the male-to-female ratio is 8:1. Intussusception is a process in which a segment of intestine invaginates into the adjoining intestinal lumen causing bowel obstruction. A common cause of abdominal pain in children is intussusception with classic triad of signs and symptoms: vomiting, abdominal pain, and passage of blood per rectum. Intussusception presents in 2 variants: idiopathic intussusception which usually starts at the ileocolic junction and affects infants and toddlers and enteroenteral intussusception (jejunojejunal, jejunoileal, ileoileal) which occurs in older children. The latter is associated with special medical situations ,cystic fibrosis, hematologic dyscrasias or may be secondary to a lead point and occasionally occur in the postoperative period.
The pathogenesis of idiopathic intussusception is not well established. It is believed to be secondary to an imbalance in the longitudinal forces along the intestinal wall. In enteroenteral intussusception this imbalance can be caused by a mass acting as a lead point or by a disorganized pattern of peristalsis (eg, an ileus in the postoperative period).
As a result of imbalance in the forces of the intestinal wall an area of the intestine invaginates into the lumen of adjacent bowel. The invaginating portion of the intestine (ie, the intussusceptum) completely “telescopes” into the receiving portion of the intestine (ie, the intussuscipiens). This process continues and more proximal areas follow allowing the intussusceptum to proceed along the lumen of the intussuscipiens.
If the mesentery of the intussusceptum is lax and the progression is rapid the intussusceptum can proceed to the distal colon or sigmoid and even prolapse out the anus. The mesentery of the intussusceptum is invaginated with the intestine leading to the classic pathophysiologic process of any bowel obstruction. Early in this process lymphatic return is impeded then with increased pressure within the wall of the intussusceptum venous drainage is impaired. If the obstructive process continues the pressure reaches a point at which arterial inflow is inhibited and infarction ensues. The intestinal mucosa is extremely sensitive to ischemia because it is farthest away from the arterial supply. Ischemic mucosa sloughs off leading to the heme-positive stools and subsequently to the classic "currant jelly stool" (a mixture of sloughed mucosa, blood, and mucus). If un treated transmural gangrene and perforation of the leading edge of the intussusceptum occur. In approximately 2-12% of children with intussusception a surgical lead point is found. Occurrence of surgical lead points increases with age and indicates that the probability of non operative reduction is highly unlikely. Examples of lead points are as follows:Meckel diverticulum ,Enlarged mesenteric lymph node, Benign or malignant tumors of the mesentery or of the intestine, including lymphoma, polyps, ganglioneuroma, and hamartomas associated with Peutz-Jeghers syndrome, Mesenteric or duplication cysts, Submucosal hematomas, which can occur in patients with HSP and coagulation dyscrasias, Ectopic pancreatic and gastric rests, Inverted appendiceal stumps,Sutures and staples along an anastomosis, Intestinal hematomas secondary to abdominal trauma, Foreign body. Although intussusception is a common condition in children it is a rare entity in the adult population [1]. Adult intussusception represents 5% of all intussusceptions and 1% to 5% of all cases of intestinal obstruction in adults. Intussusception in adults is distinct from pediatric intussusception in many aspects [2]. In contrast to intussusceptions in children a demonstrable etiology is found in 70%to 95% of cases in the adult population and approximately 40% of them are caused by primary or secondary malignant neoplasms. In general the majoritiy of lead points in the small intestine consist of benign lesions. Malignant lesions account for up to 30% of cases of intussusception in the small intestine. Intussusception occuring in the large bowel is more likely to have a malignant etiology and represents 63% to 68% of cases.The gastrointestinal tract is the most common extranodal site affected by lymphoma accounting for 5% to 20% of all cases. Primary gastrointestinal lymphoma however is very rare constituting only about 1% to 4% of all gastrointestinal malignancies. Gastrointestinal lymphoma is usually secondary to widespread nodal diseases. The most frequently affected sites are the stomach followed by the small bowel (20%-30%) and colon. Histopathologically almost 90% of primary gastrointestinal lymphomas are B-cell nonHodgkin‟s lymphoma (NHL) followed by T-cellNHL and Hodgkin‟s lymphoma (HL). Adult intussusception can be classified according to etiologic factors: primary or idiopathic and secondary. Primary or idiopathic adult intussusception accounts for about 8% to 20% of cases and is more likely to occur in the small intestine. Secondary intussusception which is more commonly present in the adult population is associated with a pathological condition involving alead point [3,4]. Adult intussusceptions have been classified into three major categories according to their gastrointestinal locations: enteroenteric, ileocolic ileocecal, and colocolic. Lymphoma, lymphosarcoma, and leiomyosarcoma have also been reported as tumoral masses inducing intestinal invagination. Benign lesions provoking large bowel intussusception include lipoma, leiomyoma, adenomatous polyp, and endometriosis, and up to 13% of colonic intussusceptions cases remain unexplained. Malignant causes of small bowel intussusception are predominantly metastases. Only rarely does a primary small bowel malignancy include adenocarcinoma, carcinoid, GIST, or lymphoma tumors. Nonmalignant lesions include benign tumors, Meckel‟s diverticulum, inflammatory fibroid polyps, lymphoid hyperplasia, adhesions, intestinal tubes, jejunostomy feedingtubes, and trauma. It was also concluded from the literature research that of the 396 cases,intussusception developed secondary to benign and malignant causes in 252 (63.6%) and 144(36.4%) cases, respectively. 50 (24.5%) of enteroenteric cases, 34 (41%) of ileocolic cases, and 60 (54.5%) of colocolic cases. The risk of intussusception secondary to malignancy rises gradually from proximal to distal. An important finding is that lymphomas which are rated third in terms of primary gastrointestinal malignancies are rated second in terms of those leading to intussusceptions.
Case Presentation
A 30 years female patient brought to the hospital with pain abdomen since one week. Ultrasound abdomen suggestive of ileo-caecal intussusception. CECT abdomen done which shows ileo-caecal intussusception as there is a short segment ileo-colic intussusceptions with the intussusceptum just extending through the ileocecal valve in to the ascending colon. Then colonoscopy done showing ileo-caecal intussusceptions.
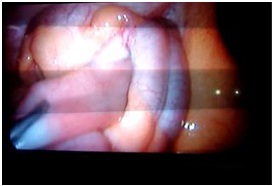
Figure 1- Intraoperative view showing intussusuception.
Laparoscopic assisted reduction of intussuception and resection of ileum-end to end anastomosis done along with appendicectomy. Resected bowel send for histopathological examination. Post operative period uneventfull patient discharged without any complications. Histopathological sections shows submucosal ileal mass extending into caecum. Tumor shows nodular arrangement of monomorphic lymphoid cells with scanty stoma. Lymphoid cells are small centrocytic with indented nuclei and large nucleoli .Centroblasts are seen and are 3-4/10HPF –these features are suggestive of ileocolic intussueption with submucosal massas the leading point. Tumor shows features of Non-hodgkins lymphoma-follicular variant.Appendicetomy speciemen shows features suggestive of acute appendicitis.
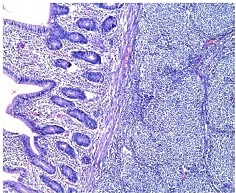
Figure 2:Microscopic view –showing of monomorphic lymphoid cells with scanty stoma. Lymphoid cells are small centrocytic with indented nuclei and large nucleoli .Centroblasts are seen and are 3-4/10HPF –these features are suggestive of ileocolic intussueption with submucosal mass of Non-hodgkins lymphoma-follicular variant.
Discussion
Lymphoma is a type of cancer that affects lymph cells and tissues including white bloodcells, lymph nodes and the spleen. It may arise anywhere outside of the lymph nodes and may develop in the gastrointestinal tract including the stomach, ileum, and colon. Lymphoma is divided into two major categories: HL and NHL. HL most commonly occurs in the cervical lymph nodes. The extra nodal forms are rare and account for less than 1%. The most common site of involvement is the gastrointestinal tract followed by the pulmonary system, thyroid, skin, genitourinary system and central nervous system. NHL is much more common than HL. The gastrointestinal tract is the most commonly involved site for extra nodal NHL accounting for20% to 50% of all extra nodal disease. The most common primary site is the stomach followed by the small intestine, colon, and rarely other gastrointestinal organs. Gastrointestinal NHL represents between 1% and 4% of all gastrointestinal malignancies and 10% to 20% of small bowel .Both of these malignancies may cause similar symptoms but the conditions themselves differ. The distinction between HL and NHL is made upon histopathological examination of the cancerous material. While HL develops from a specific abnormal B lymphocyte lineage, NHL may derive from either abnormal B or T cells. There are five subtypes of HL and about 30 subtypes of NHL. There are many classifications of gastrointestinal tract lymphoma. For simplicity clinical staging is based on the Ann Arbor classification and histopathologic staging is based on the World Health Organization (WHO) classification. According to this classification lymphomas of the gastrointestinal tract generally fall into one of six categories: extranodal marginal zone mucosa-associated lymphoma tissue (MALT lymphoma), follicular lymphoma, mantle cell lymphoma, diffuse large B-cell lymphoma and Burkitt's lymphoma. Many of the NHL subtypes look similar but they are functionally quite different and respond to different therapies with different probabilities of cure. HL subtypes are microscopically distinct and typing is based upon the microscopic differences as well as extent of disease. There are some well-known risk factors for gastrointestinal lymphomas. They include Helicobacter pylori infection, inflammatory bowel diseases, autoimmune disorders, immunodeficiency syndromes, immunosupression, transplantation,celiac disease and nodular lymphoid hyperplasia. The most appropriate treatment modalities for primary gastrointestinal lymphomas are still controversial [5,6,7]. Some Authors advocate that only surgical procedures performed with regard to oncological principles are sufficient while others support that addition of chemotherapy to surgery increases survival. Generally chemotherapy is recommended along with surgery in cases with poor prognostic factors such as high LDH level, T-cell phenotype, extra nodal involvement of≥ 2, Ann Arbor stage of III to IV, age of > 60years and ECOG performance status of ≥ 2. High positivity rates of the Ki67 proliferation index immunochemically correlate with the aggressive course of a tumor. Thus one must take this into consideration when scheduling a treatment approach In localized primary and in low-grade intestinal lymphomas the most appropriate approach is to perform different chemotherapy protocols along with surgery in cases with the afore mentioned poor prognostic factors. In secondary gastrointestinal lymphomas chemotherapy should be performed first with regard to features of primary disease followed by large or limited surgery with regard to the status of disease in the intestinal system. However the size of the surgical procedure should be determined according to intra operative findings in cases requiring urgent surgery because of signs and symptoms of intestinal obstruction. The preoperative diagnosis of adult intussusception is difficult because the clinical presentation is often nonspecific and the condition is rare. An accurate diagnosis is based on a good medical history thorough physical examination [8,9]. Intussusception and gastrointestinal lymphoma diagnosed by specific imaging modalities such as X-rays, ultrasound (US), CT, magnetic resonance imaging(MRI), enteroclysis, endoscopic procedures, diagnostic laparoscopy, scintigraphy, angiography,capsule endoscopy, and FDG-PET/CT. Ultrasound is considered to be a useful tool for the diagnosis of intussusception in both children and adults. Its classical imaging features include the target or doughnut sign in the transverse view and the pseudo kidney, sandwich, or hayfork sign in the longitudinal view. Ultrasound has a sensitivity of 98% to 100% and a specificity of 88% for diagnosing intussusceptions. Abdominal CT is currently considered the most sensitive radiological method for confirming intussusception with a reported diagnostic accuracy of 58% to 100%. On CT a bowel-within-bowel configuration suggested by mesenteric fat and vessels compressed between the walls of the small bowel is pathognomonic .For diagnosing intussusceptions- with laparoscopy (100%), followed by CT (57%-93.9%), colonoscopy (42.1%-45.4%), and barium enema (45.4%-73%) There is no universal approach to the management of adult intussusception. Most of the debate focuses on the issue of primary enbloc resection versus initial reduction followed by resection. Reduction by surgery before resection may theoretically permit a more limited resection. However the risk of potential intraluminal seeding or venous tumor dissemination during the manuplation of a malignant lesion should be considered. The prevalence of malignancy as the cause of enteroenteric intussusception is as high as 30% and the vast majority are metastatic. Conversely in the large bowel and ileocolic region it is more likely that the intussusception will have a malignant etiology (up to 68%). Primary malignant tumors of the small intestine are very rare accounting for less than 2% of all gastrointestinal malignancies. Intestinal lymphoma constitutes 10% to 20% of all small intestine neoplasms and 20% to 30% of all primary gastrointestinal lymphomas. The ileum is the most common site affected by small intestine lymphoma followed by the jejunum and duodenum. While intussusception is a very rare presentation of NHL the most common lymphoma is diffuse large B-cell NHL
The English medical literature published between 2000 and 2011 in the PubMed and GoogleScholar databases was reviewed and 33 reports concerning 36 cases of intussusception due to lymphoma meeting the aforementioned criteria were included in this review. The patients were aged from 16 to 86 years (mean, 48.2 ± 19.0 y).
Twenty-nine were male (mean, 45.8 ± 18.1 y) and seven were female (mean, 58 ± 18.9 y). According to the localization of lymphoma 24 patients had ileo-colic intussusception, 10 had enteric, and 2 had colic intussusception. In terms of the diagnosis 34 patients were diagnosed with various types of NHL and two patients were diagnosed with HL. Adult intussusception almost always requires surgery. The chronicity may not allow successful pneumatic or hydrostatic reduction due to cross-scarring between the intussusceptum and the intussuscipiens. More importantly the lesion at the apex (the „lead point‟) may escape detection. Whereas the intussusception itself has a very good prognosis the decisive prognostic factor is expected to be the nature of the lesion leading to the process. Technically the operation itself is seldom tedious anymore than a conventional resection and anastomosis. A view is held to reduce the intussusception at the operation as much as safely possible followed by appropriate resection. This may preserve bowel length. Also it may avoid injury to the superior mesenteric vessels if the intussusception mass were engulfing major part of the mesentery. Others recommend resecting without reducing too enthusiastically and especially colonic intussusceptions. This is thought to increase the likelihood of bowel injury or ischaemia. In addition manipulation may lead to dissemination or perforation. The overall incidence of malignancy at the apex of an intussusception is 43-56%. Colo-colic intussusception may be secondary to a carcinoma in up to 43-80%. Idiopathic intussusception occurs in only 6.6-15% the adults as compared to the children.
Laparoscopic assisted reduction of intussueption and resection of ileum-end to end anastomosis done along with appendisectomy done in this case. Resected bowel send for histopathological examination. Post operative period uneven full patient discharged without any complications. Histopathological examination of tumor shows features of Non Hodgkin's lymphoma-follicular variant.
Conclusions
Adult intussusception remains a rare cause of persistent or intermittent chronic abdominal pain. In contrast to its paediatric counterpart the treatment almost always is surgical. For intussusception due to Non Hodgkin's lymphoma surgery should perform by following oncological principles is enough in case of localized primary and in low grade intestinal lymphomas.
Ethical Considerations
Consent taken from the patient and from ethical committee for publication.
Conflict of Interests
No conflict of interest from all the authors
Acknowledgements
First all the authors thank full to the patient for giving consent and also to the staff assisted for the case
Learning Points
1. Adult intussusception represents 5% of all intussusceptions and 1% to 5% of all cases of intestinal obstruction in adults. Intussusception occuring in the large bowel is more likely to have a malignant etiology and represents 63% to 68% of cases.
2. In contrast to intussusceptions in children a demonstrable etiology is found in 70%to 95% of cases in the adult population and approximately 40% of them are caused by primary or secondary malignant neoplasms.
3. For intussusception due to Non-hodgkins lymphoma surgery should perform by following oncological principles is enough in case of localized primary and in low grade intestinal lymphomas.
References
1. Agfa F. Intussusception in adults. AJR 1986; 146:527-31.[Pubmed].
2. Orlando R. Intussusception in adults: Bowel obstruction:Differential diagnosis and clinical management. Welch JP(Ed) W B. Saunders Company, Philadelphia, 1990.
3. Taraneh A, Berger BL. Adult intussusception. Ann Surg1997; 226:134-40. [Pubmed].
4. Briggs DF, Carpathios J, Zollinger RW. Intussusception inadults. Am J Surg 1961; 101:109-13.
5. Nagorney DM, Sarr MG, Mcllrath DC. Surgical management of intussusception in the adult. Ann Surg 1981; 193:238 AYDEDE el al.230-6 [Pubmed].
6. Weilbaecher D, Bolin JA, Hearn D, Ogden W.Intussusception in adults: review of 160 cases. Am J Surg 1971; 121:531-5. [Pubmed].
7.Stubenbord WT, Thorbjarnarson B. Intussusception in adults. Ann Surg 1970; 172: 306-10. [Pubmed].
8. Youngson GG. Small bowel lymphoma presenting as chronic adult intussusception. Scott Med J 1981; 26: 260-1. [Pubmed].
9. Bazzocchi R, Palmieri V, Lafratta V, et al. Ileo-ceco-colic invagination. A proposal of a case caused by lymphoma ofthe last ileal loop. Minerva Chir 1980; 15;35:1295-302[Pubmed"]
10. Acay M, Polat M, Çadırcı M, Gencer B. Tumor-induced ileoileal invagination invagination in adults. Am Surg 1994;60: 980-81. [Pubmed]

