Original Article

Gasless single-incision laparoscopic cholecystectomy: Preliminary results
4Nobumi Tagaya, 1Akihito Abe, 2Shoujirou Taketsuka, 3Kazunori Kasama, 4Masatoshi Oya
- 1Second Department of Surgery, Dokkyo Medical University, Tochigi, Japan
- 2Department of Surgery, Horie Hospital, Gunma, Japan
- 3Minially Invasive Surgery Center, Yotsuya Medical Cube, Tokyo, Japan
- 4Department of Surgery, Dokkyo Medical University Koshigaya Hospital, Saitama, Japan
- Submitted: December 26, 2012
- Accepted: January 6, 2012
- Published: January 6, 2012
This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/3.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited
Introduction
Laparoscopic cholecystectomy has usually been performed using three or four ports. As expertise with the technique has improved, however, we have begun to use only one or two ports. Here we report differences between the previous and present methods of gasless single-incision laparoscopic cholecystectomy (SILC).
Patients and methods
Twelve patients (7 males and 5 females aged between 30 and 75 years, mean 56.5 years) were enrolled in this study. The mean BMI was 25.8 (range: 22.5-37.1) kg/m2. They were divided into two groups depending on the procedural period (Group1, November 1997-June 1998, and Group 2, December 2009-March 2010). Under general anesthesia, a 2.5 cm vertical incision was made at the umbilicus, and the operating field was created using the original abdominal wall-lift method with a rigid bar. Two 5-mm ports were placed through the same umbilical incision but through separate fascial incisions. After exposing the Calot triangle, the hilum of the gallbladder was dissected laterally and medially to expose the cystic duct and artery, which were then ligated with clips and divided with scissors or coagulating shears. The gallbladder was retrieved using a retrieval bag.
Results
We performed SILC successfully in 10 cases, and the other 2 in Group 2 required conversion to SILC with pneumoperitoneum due to difficulty with the surgical procedure. However, none of the procedures required conversion to open cholecystectomy or addition of other ports. The mean operation time and postoperative hospital stay was 202 min and 7.0 days, and 115 and 3.2 in Group 1 and 2, respectively. There were no intra- or postoperative complications.
Conclusion
Although evaluation of our operative outcomes is still premature due to lack of sufficient experience, our present series shows that gasless SILC is technically feasible and safe for any surgeon sufficiently experienced in the standard technique of laparoscopic cholecystectomy and has additional aesthetic and cost advantages.
Key words
gasless, laparoscopic cholecystectomy, single-incision, laparoscopic surgery, single port.
Introduction
Laparoscopic cholecystectomy has usually been performed using a four-port technique. As expertise with the technique has improved, operative outcomes achieved by reducing the number of ports have become similar to those for the four-port technique. We have also tried to carry out laparoscopic cholecystectomy using three or two ports [1,2]. Furthermore, Navarra et al., [3] reported a successful one-wound laparoscopic cholecystectomy in 1997. Therefore, we also performed one-port laparoscopic cholecystectomy using the abdominal wall lift method without pneumoperitoneum (gasless method) for 6 patients between November 1997 and June 1998 [4]. Piskun et al., also reported transumbilical laparoscopic cholecystectomy with two transumbilical trocars and two transabdominal stay sutures in 1999 [5]. However, these techniques were not generally accepted into clinical practice because of troublesome intra-abdominal maneuvering of the laparoscopic instruments and the technical demands at that time. After the introduction of natural orifice translumenal endoscopic surgery (NOTES) [6-10], single-incision laparoscopic cholecystectomy (SILC) became an attractive procedure, and its use spread rapidly worldwide [11-14]. However, SILC has generally been performed under pneumoperitoneum, and no reports of gasless SILC have been published. Therefore, we introduced a modified gasless SILC technique based on our previous gasless method.
| Group |
Case |
Age |
Sex |
BMI |
Diagnosis |
|
|
|
(M:F) |
(kg/m2) |
(Stone:Polyp) |
| 1 |
6 |
60 |
3:3 |
25.2 |
5:1 |
|
|
(44-70) |
|
(22.5-32.8) |
|
| 2 |
6 |
53 |
4:2 |
26.5 |
5:1 |
|
|
(37-75) |
|
(23.0-37.1) |
|
( ): Range
Materials and Methods
Twelve patients with gallbladder stone in 10 and polyp in 2 were enrolled in this study (Table 1). Diagnoses were made by abdominal ultrasonography and abdominal computed tomography with three-dimensional reconstruction of the biliary tract or magnetic resonance cholangiopancreatography, as necessary. They were divided into two groups depending on the procedural period. Group 1 was performed SILC between November 1997 and June 1998, and Group 2 between December 2009 and March 2010. The mean patient age was 60 (range, 44-70) years in Group 1 and 53 (range, 30-75) years in Group 2. There were 3 males and 3 females, with a mean BMI of 25.2 (range, 22.5-32.8) kg/m2 in Group 1, and 4 males and 2 females, with a mean BMI of 26.5 (range, 23-37.1) kg/m2 in Group 2.
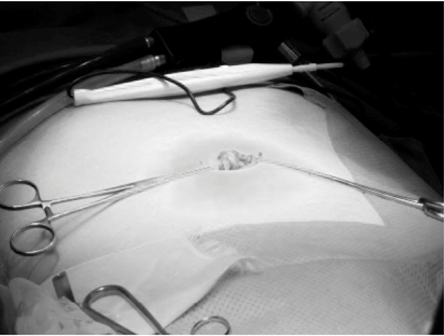
Figure 1: A 2.5-cm vertically oriented incision was made through the center of the umbilicus.
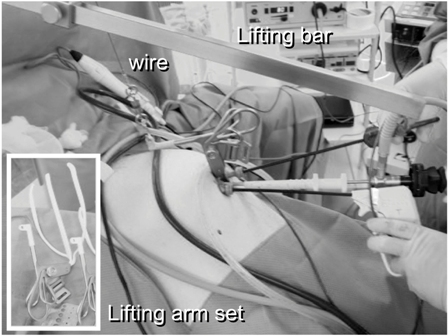
Figure 2: The operating field was created using the original bar abdominal wall-lift method with a rigid bar.
Operative technique
With the patient placed supine under general anesthesia, a 2.5-cm vertically oriented incision was made through the center of the umbilicus (Fig.1). The operating field was created using the original abdominal wall-lift method with a rigid bar (Mizuho Co. Ltd. Tokyo, Japan) (Fig.2). We used all-rigid instrumentations without the use of articulating tools. Two 5-mm ports were placed through the same umbilical incision, but through separate fascial incisions. The patient was then placed in a reverse Trendelenburg position with the right side rotated up. The procedure was performed by one surgeon standing between the legs of the patient, and one laparoscopist on the left side (Fig.3). The procedures were similar to those of three-port technique for cholecystectomy. One grasper was used at the fundus or infundibulum of the gallbladder for retraction laterally or upward (Fig.4). After exposing the Calot triangle, the hilum of the gallbladder was dissected laterally and medially to expose the cystic duct and artery (Fig.5). We were able to obtain a critical view even with this procedure. The cystic duct and artery were ligated with clips and divided with scissors or coagulating shears. The gallbladder was dissected from the gallbladder fossa with coagulating shears. A retrieval bag was inserted into the peritoneal cavity to remove the gallbladder. The fascial defect was repaired with 2-0 absorbable sutures, and the skin was treated by packing a small gauze ball on the wound (Fig.6).

Figure 3: This procedure was performed by one surgeon standing between the legs of the patients and one laparoscopist on the left side.
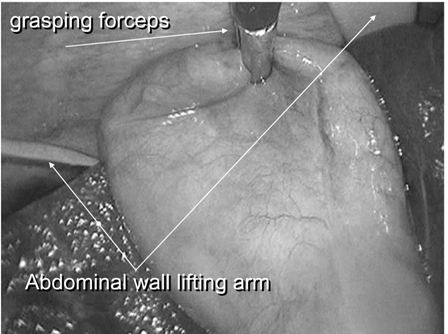
Figure 4: One grasper was used at the fundus of the gallbladder for retraction laterally or upward.
Result
(Table 2) showed outcomes of our study. We performed SILC successfully in all cases of group 1 and 4 cases in group 2, and the other 2 in group 2 required conversion to SILC under pneumoperitoneum. However, no procedures required conversion to open cholecystectomy or additional of another ports. The operation time ranged from 136 to 253 min, with a mean of 202 min in Group 1, and 93 to 151 min, with a mean of 115 min in Group 2. In Group 2, the mean operation time of complete gasless method and conversion to pneumoperitoneum was 95 and 156 min, respectively. Intraoperative bleedings was minimal, and there were no intra- or postoperative complications. The postoperative hospital stay ranged from 4 to 9 days, with a mean of 7.0 days in Group 1, and 2 to 4 days, with a mean of 3.2 days in Group 2. There was no need for any special instruments or ports with this technique. Pathological diagnosis revealed severe cholecystitis in 2 cases of Group 1 and 1 of Group 2.
| Group |
Case |
Operation
time (min) |
IOC |
Conversion
to c- LC |
POH (day) |
Complication |
| 1 |
6 |
202 |
+ |
0 |
7.0 |
- |
| 2 |
6 |
115 |
- |
0 |
3.6 |
- |
| 2-1 |
4 |
95 |
- |
0 |
3.7 |
- |
| 2-2 |
2 |
156 |
- |
0 |
3.5 |
- |
IOC: intraoperative cholangiography,
POH: postoperative hospital stay
c-LC: conventional laparoscopic cholecystectomy
2-1: complete of gasless method, 2-2: conversion to pneumoperitoneum
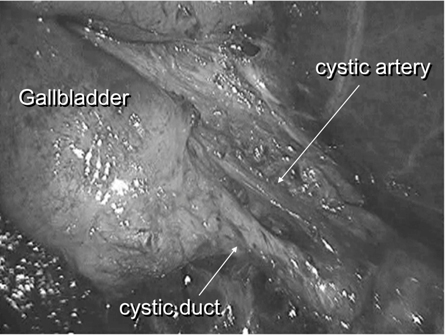
Figure 5: The cystic duct and artery were divided and identified to obtain the critical view.
Discussion
SILC has been performed at many institutions, including rural hospitals, because it can be accomplished using ordinary laparoscopic instruments and yields better cosmetic results. In general, SILC has been performed under pneumoperitoneum with CO2 gas. The main benefit of pneumoperitoneum in comparison with the abdominal wall lifting method is to create a wider operative field. However, it is often difficult to treat accidental events such as bleeding or insufficient CO2 supply immediately within the limited working space. Therefore, we tried to perform SILC using an abdominal wall lifting (gasless) method. Although the present report is still preliminary, it shows that this gasless method has several advantages.
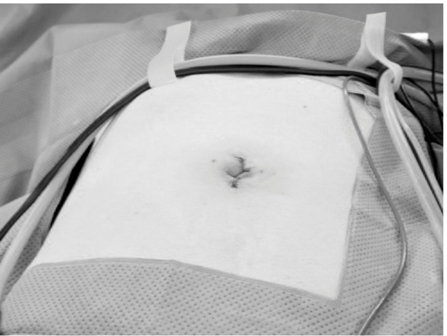
Figure 6: The closed umbilical wound.
The advantages of gasless SILC compared with pneumoperitoneum are
[1] there is no concern about CO2 leakage from the umbilical wound, [2] there is no stress related to the insertion of gauze to clarify the origin of bleeding, or suction to evacuate the blood lake,
[3] the lower cost because no special ports or instruments are needed, and [4] the surgery is clip-less with no need for extracorporeal sutures. On the other hand, the disadvantages of this procedure are
[1] the narrowness of the operative field in which to manipulate the gallbladder,
[2] direct damage to the anterior abdominal wall due to lifting with a rigid bar. On the basis of these considerations, we think that our method considerably reduces the cost of laparoscopic surgery [5].
There have been no previous reports of gasless SILC. Our present operative outcomes were compared with those for pneumoperitoneum, based on a review of reports involving more than 10 (range, 10-100) cases [10-27]. In those reports, the operation time ranged from 40 to 148 min, with a mean of 86 min. Although this result was superior to ours, the outcome was greatly dependents on insertion of a fourth port or the suspension of stay sutures. In fact, Podolsky et al. [28] reported that their operation time using a completely transumbilical approach under pneumoperitoneum without the use of a fourth port ranged from 95 to 168 min, with a mean of 121 min, which is similar to our results. However, this was still longer than for standard laparoscopic cholecystectomy. The rate of conversion to standard laparoscopic cholecystectomy ranged from 0% to 40%. The reasons were difficulty with identification of the cystic duct and artery, bleeding from the cystic artery, use of choledochoscopy for exploration of common bile duct stones, and failure with port insertion, respectively. In our series, although there was no instance of conversion to standard laparoscopic cholecystectomy, pneumoperitoneum was required in order to continue SILC in two cases. This is a disadvantage of the gasless method, which often makes it difficult to obtain a sufficient operative field. Pneumoperitoneum provides an operative field that is adequate for moving the anterior abdominal wall upward, and the intraperitoneal organs surrounding the gallbladder including the greater omentum, colon and duodenum, downward. The reported postoperative complication rate was 3.1 % (14 out of 450 cases). Thirteen of the complications involved subcutaneous hematoma, bile leakage, injury to the right hepatic duct, liver, or mesenterium, urinary retention or pain control issues. Decisions about adequate conversion must be decided on the basis of a low threshold to avoid major complications in the SILC setting. Furthermore, familiarity with the technique of SILC with pneumoperitoneum is essential in case conversion from the gasless method becomes necessary.
Several reports have recommended the insertion of fine-caliber instruments that can act as a functional extra port [19,29], or suspension of stay sutures [11,12,19,25,27] from the right subcostal margin to allow retraction of the fundus or infundibulum of the gallbladder. This maneuver provides optimal visual exposure similar to a standard four-port laparoscopic cholecystectomy and minimizes the operation time. Another report [22] has recommended the insertion of 5-mm grasping forceps as a fourth manipulator via the umbilical wound just below the laparoscope for retraction of the gallbladder fundus. This maneuver also provides the same benefits as SILC with independent manipulation of the fundus and infundibulum. Furthermore, Dominguez et al. [30] have reported the usefulness of retraction and triangulation with neodymium magnetic forceps for single-incision laparoscopic surgery. This magnetic forceps is applicable to many surgical procedures for avoiding damage to the abdominal wall. We have performed SILC using only three instruments comprising one laparoscope and two grasping or dissecting forceps. The operation time was similar to others without the use of fourth instruments. However, this attractive technique requires a steady and safe approach, and there should be no hesitation about adding an extra port or instruments to accomplish it successfully.
The most important consideration when performing SILC, with or without gas insufflation, is how to manipulate the multiple instruments including a laparoscope within the limited working space. In order to avoid or minimize any conflict between the operative instruments and the laparoscope, dissection using the left hand with retraction of using the right hand is an effective approach within the narrow working space. This makes it possible to avoid any parallel or crossing movement of the laparoscope and dissecting forceps during exposure of the cystic duct and artery from the umbilicus incision. In particular, we think that the requirement to for overcoming the difficulties associate with single-incision laparoscopic procedures.
Conclusion
Although evaluation of our operative outcomes is still premature due to the low number of cases experienced, we consider that gasless SILC is technically feasible and safe in selected patients for any surgeon who is experienced in standard techniques of laparoscopic cholecystectomy, and provides both cosmetic and cost advantages.
Authors' Contribution
TN: Prepared literature search and the draft manuscript.
AH, TS, KK: Helped in designing the study.
OM: Helped in writing manuscript.
Conflict of Interests
The authors declare that they have no conflict of interest.
Funding
None
References
[1]. Tagaya N, Kita J, Takagi K, Imada T, Ishikawa K, Kogure H, Ohyama O. Experience with three-port laparoscopic cholecystectomy. J Hepato-Biliary-Panc Surg. 1998; 5: 309-311. [Pubmed].
[2]. Tagaya N, Fukutomi K, Kogure H (1999) New two-port technique for laparoscopic cholecystectomy. Dokkyo J Med Sci 26: 419-422.
[3]. Navarra G, Pozza E, Occhionorelli S, Carcoforo P, Donini I. One-wound laparoscopic cholecystectomy. Br J Surg 1997; 84: 695. [Pubmed].
[4]. Piskun G, Rajpal S. Transumbilical laparoscopic cholecystectomy utilizes no incisions outside the umbilicus. J Laparoendosc Adv Surg Tech 1999; 9: 361-364. [Pubmed].
[5]. Tagaya N, Mikami H, Kogure H (2000) Gasless one port laparoscopic cholecystectomy. Dokkyo J Med Sci 27: 319-322. (Japanese with English abstract)
[6]. Marescaux J, Dallenmagne B, Perretta S, Wattiez A, Mutter D, Coumaros D. Surgery without scars: report of transluminal cholecystectomy in a human beings. Arch Surg 2007; 142: 823-827. [Pubmed].
[7]. Bessler M, Stevens PD, Milone L, Parikh M, Fowler D. Transvaginal laparoscopically assisted endoscopic cholecystectomy: a hybrid approach to natural orifice surgery. Gastrointest Endosc 2007; 66: 1243-5. [Pubmed].
[8]. Marks JM, Ponsky JL, Pearl JP, McGee MF. PEG “Rescue”: A practical NOTES technique. Surg Endosc 2007; 21: 816-9. [Pubmed].
[9]. Zorron R, Maggioni LC, Pombo L, Oliveira AL, Carvalho GL, Filgueiras M. NOTES transvaginal cholecystectomy: preliminary clinical application. Surg Endosc 2008; 22: 542-7. [Pubmed].
[10]. Rao GV, Reddy DN, Banerjee RB. NOTES: Human experience. Gastrointes Endoscopy Clin N Am. 2008; 18: 361-70. [Pubmed].
[11]. Rao PP, Bhagwat SM, Rane A, Rao PP. The feasibility of single port laparoscopic cholecystectomy: a pilot study of 20 cases. HPB (Oxford) 2008; 10: 336-341. [Pubmed].
[12]. Cuesta MA, Berends F, Veenhof AA. The “invisible cholecystectomy”: a transumbilical laparoscopic operation without a scar. Surg Endosc 2008; 22: 1211-1213. [Pubmed].
[13]. Palanivelu C, Rajan PS, Rangarajan M, Parthasarathi R, Senthilnathan P, Praveentraj P. Transumbilical flexible endoscopic cholecystectomy in humans: first feasibility study using a hybrid technique. Endoscopy. 2008; 40: 428-431. [Pubmed].
[14]. Navarra G, La Malfa G, Bartolotta G, Curro G. The invisible cholecystectomy: a different way. Surg Endosc 2008; 22: 2103. [Pubmed].
[15]. Merchant AM, Cook MW, White BC, Davis SS, Sweeney JF, Lin E. Transumbilical Gelport access technique for performing single incision laparoscopic surgery (SILS). L Gastrointest Surg 2009; 13: 1590162. [Pubmed].
[16]. Zhu JF, Hu H, Ma YZ, Xu MZ, Li F. Transumbilical endoscopic surgery: a preliminary clinical report. Surg Endosc. 2009; 23: 813-817. [Pubmed].
[17]. Bucher P, Pugin F, Buchs N, Ostermann S, Charara F, Morel P. Single port access laparoscopic cholecystectomy (with video). World J Surg. 2009; 33: 1015-1019. [Pubmed].
[18]. Langweiler TE, Nimmesgern T, Back M. Single-port access in laparoscopic cholecystectomy. Surg Endosc. 2009; 23: 1138-1141. [Pubmed].
[19]. Tacchino R, Greco F, Matera D. Single-incision laparoscopic cholecystectomy: surgery without a visible scar. Surg Endosc. 2009; 23: 896-899. [Pubmed].
[20]. Hong TH, You YK, Lee KH. Transumbilical single-port laparoscopic cholecystectomy. Scarless cholecystectomy. Surg Endosc. 2009; 23: 1393-1397. [Pubmed].
[21]. Kuon Lee S, You YK, Park JH, Kim HJ, Lee KK, Kim DG. Single-port transumbilical cholecystectomy: A preliminary study in 37 patients with gallbladder diseases. J Laparoendosc Adv Surg tech. 2009; 19: 495-499. [Pubmed].
[22]. Podolsky ER, Rottman SJ, Curcillo II PG. Single port access (SPA) cholecystectomy: two year follow-up. JSLS 2009; 13: 528-535. [Pubmed].
[23]. Philipp SR, Miedema BW, Thaler K. Single-incision laparoscopic cholecystectomy using conventional instruments: early experience in comparison with the gold standard. J Am Coll Surg. 2009; 209: 632-637. [Pubmed].
[24]. Hemandez JM, Morton CA, Ross S, Albrink M, Rosemurgy AS. Laparoscopic single site cholecystectomy: the first 100 patients. Am Surg. 2009; 75: 681-685. [Pubmed].
[25]. Chow A, Purkayastha S, Paraskeva P. Appendicectomy and cholecystectomy using single-incision laparoscopic surgery (SILS): The first UK experience. Surg Innov. 2009; 16: 211-217. [Pubmed].
[26]. Ersin S, Firat O, Sozbilen M. Single-incision laparoscopic cholecystectomy: is it more than a challenge? Surg Endosc. 2010; 24: 68-71. [Pubmed].
[27]. Roberts KE, Solomon D, Duffy AJ, Bell RL. Single-incision laparoscopic cholecystectomy: a surgeon’s initial experience with 56 consecutive cases and a review of the literature. J Gastrointest Surg. 2010; 14: 506-510. [Pubmed].
[28]. Podolsky ER, Rottman SJ, Poblete H, King SA, Curcillo PG. Single port access (SPATM) cholecystectomy: a completely transumbilical approach. J Laparoendosc Adv Surg Tech. 2009; 19: 219-222. [Pubmed].
[29]. Hirano Y, Watanabe T, Uchida T, Yoshida S, Tawaraya K, Kato H, Hosokawa O. Single-incision laparoscopic cholecystectomy: single institution experience and literature review. World J Gastroenterol. 2010; 16: 270-274. [Pubmed].
[30]. Dominguez G, Durand L, De Rosa J, Danguise E, Arozamera C, Ferraina PA. Retraction and triangulation with neodymium magnetic forceps for single-port laparoscopic cholecystectomy. Surg Endosc. 2009; 23: 1660-1666. [Pubmed].

