Original Article

Conventional Versus Neuro-Navigation Guided Shunt Surgery
*Janak Raj*, *VKulwant Singh*, *Divye Prakash Tiwari*
- **Department of Neurosurgery, Institute of Medical SciencesBanaras Hindu University,Varanasi,India
- Sunday, October 13, 2013
- Thursday, October 31, 2013
- Thursday, November 21, 2013
This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/3.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Objective
The aim of study is to evaluate the efficacy of ventricular catheter placement through neuro-navigation versus conventional technique.
Methods
All patients undergone ventriculo-peritoneal shunt from August 2011 to September 2013 were included in this study. Total sixty cases were included and divided into two groups. The first group comprised of shunt surgery using conventional method of shunt placement as per anatomical landmarks. The second group had proximal end placement with help of Frameless Neuronavigation System. The relationship between proximal ventricular catheter position and shunt revision rate was evaluated using postoperative computed tomography by a 3-point scale: 1) Grade I; Position of tip is anterior to foramina of monro , free-floating in cerebrospinal fluid, 2) Grade II; touching choroid plexus or ventricular wall, tip is posterior to foramina of monro 3) Grade III; tip within parenchyma, crossing to opposite side.
Results
Sixty patients were considered, and divided into two groups: 1.Ventricular end insertion through conventional technique, 2. Neuronavigation assisted ventricular end insertion. There were 30 patients in each group. In conventionally treated study group, 20 patients (66.66%) revealed grade 1 placement of ventricular end,8patients (26.66%) had grade 2, and 2 patients(6.66%) showed grade 3 in post operative CT scan. Neuronavigation study group had 28 patients (93.33%) in grade 1 placement and 2 patients (6.66%) in grade 2 while none was in grade 3 on post operative CT scan. Infection rate was same in both groups.
Conclusion
Despite technological improvements, ventriculoperitoneal shunts are still often complicated by malfunction, predominantly with proximal catheter obstruction.Significant proportion of shunt fail¬ures were due to obstruction of the ventricular catheter, and accurate placement of the shunt catheter is highly important to reduce the incidence of shunt malfunction. Frameless navigation is a valuable tool to optimize the trajectory and final position of shunt catheter. The use of navigation in routine shunt surgery can eliminate poor shunt placement resulting in a dramatic reduction in failure rates thus the incidence of revision will go down.
Key Words
Neuronavigation, Hydrocephalus, Ventriculoperitoneal shunt.
Introduction
Accurate placement of ventricular catheter is related with both proper insertion trajectory and catheter tip positioning. So recently, many studies have validated accuracy in VP shunt with the development of frameless neuronavigation in the field of neurosurgery. [1] Proximal catheter obstruction is known to be the most common cause of malfunctioning of ventriculoperitoneal (VP) shunt followed by infection and disconnection. Thus, the chief concern when inserting a VP shunt should be the precise placement of the ventricular catheter. The standard technique of ventricular catheter placement depends on anatomic landmarks; however, this may not be satisfactory to consistently ensure optimal positioning of the ventricular catheter. The optimal position of the catheter tip was focused to reduce potential occlusion of proximal catheter by ventricular parenchyma or choroidal tissues. [2] Many studies including Tuli et al.have shown that a ventricular catheter tip surrounded by cerebrospinal fluid (CSF) could decrease the risk of shunt failure. [3,4] The present study was a done to evaluate and compare the conventional method of ventriculoperitoneal shunt insertion with Neuronavigation.
Patients and Methods
All the patients of CT proven Hydrocephalus who have been managed prospectively in neurosurgery department were included in study. Each patient had a precise chart review with multiple variables including age, causes of hydrocephalus, interval time between the first shunt operation and revision, and reason for shunt failure. All patients had preoperative and postoperative brain imaging to reveal the out¬come of shunt surgery. All cases of CT proven hydrocephalus requiring shunt will be included into study.
1.Acute phase of bacterial and tubercular meningitis presenting as hydrocephalus were excluded from study.
2.Cases were randomly subjected to conventional and navigation guided shunting.
3.On 5th post operative period day plain CT head of all patients were done and position of proximal catheter tip position was evaluated using postoperative CT by a 3-point scale.
1) Grade I; Position of tip is anterior to foramina of monro, optimal position free-floating in cerebrospinal fluid.
2) Grade II; touching choroid plexus or ventricular wall, tip is posterior to foramina of monro.
3) Grade III; tip within parenchyma orcrossing to opposite side.
All patients were divided into 2 groups of 30 cases each according to the use conventional method and navigation guided method of surgery. The first group had catheter inserted using manual method with anatomical landmark. The second group received surgery using neuro- navigation (Stealth Station Treon Plus navigation system, Medtronic, USA) for routine shunt placement. Patients with shunts were followed up for more than 3 months or until the shunt failure in both groups.
Surgical technique
Shunt procedures were performed by neurosurgeons with various training levels. The valve type and catheter were used depending on the surgeon’s preference. In the standard group, skin incision and trepination of the cranium was done by using anatomical landmarks like Kocher’s point or Frazier’s point. Ventricular catheter length was determined based on surgeon’s measurement using brain CT imaging. In Neuronavigation group, after induction of general anesthesia, the head was immobilized in a sugita head clamp. Patient-to-image registration was done based on point-pair matching using the blunt tip registration probe. The entry point was localized at the junction of the plane approximately 2 cm lateral to the midline in the mid-pupillary line intersecting the line drawn from superior aspect of pinna. The target point was determined and set at the foramen of Monro. The patient was then prepared and draped in the usual sterile fashion appropriate for a ventriculoperitoneal shunt placement. A comma-shaped incision was made around the entry point and a subcutaneous pocket was prepared for the shunt valve. Distal tunneling from the entry point passing the retroauricular region to the paraumbilical abdomen was performed in a standard fashion. After position verification, a burr hole through the skull was made following the predefined trajectory. The duramater was cauterized and incised. To introduce a catheter over a shunt insertion trajectory, an image-guided articulating holder was aimed in the exact direction of the trajectory under continuous position verification. The entry point previously located on the skin was converted to the pivoting point of the instrument holder consequently, the neuronavigation workstation showed the trajectory length. A ventricular catheter was marked at the appropriate length. A custom made catheter guidance tube (shaft diameter 3.1 mm) was inserted in the instrument holder. An elongated stylet was used to direct the catheter straight over the shunt trajectory into the ventricle after removal of the stylet. Cerebro Spinal Fluid egression was observed and the catheter was advanced another centimeter. The catheter was then secured to the valve. Before introducing the distal drain tip in the abdomen, flow patency of the shunt was ascertained. Woundclosure was done in a standard manner.
Grading system of shunt placement
Proximal catheter position was graded on postoperative brain CT imaging in each case. All patients were graded according the following 3-point scale developed for this study
Results
Proximal catheter position was graded on the basis of postoperative brain CT imaging on each case. All patients were graded according the following 3-point scale developed for this study (Table). 1)
| Conventional |
|
percent |
Neuronavigation |
|
percent |
| Grade 1 |
20 |
66.66 |
Grade 1 |
28 |
93.33 |
| Grade 2 |
8 |
26.66 |
Grade 2 |
2 |
6.66 |
| Grade 3 |
2 |
6.66 |
Grade 3 |
0 |
0 |
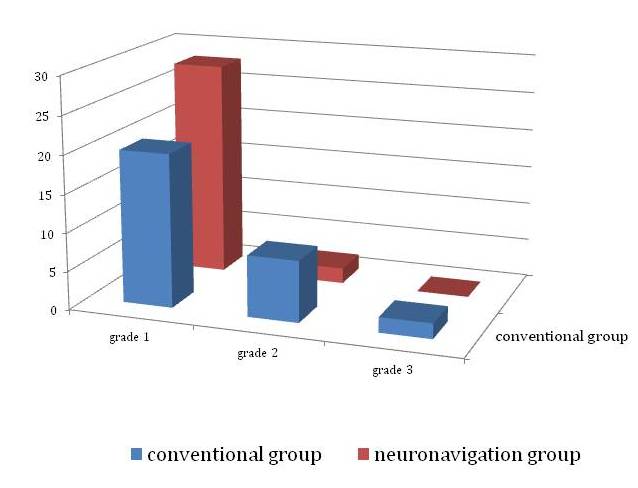
Grade I: Twenty patients of conventional group (66.66%) were in grade 1 while in navigational group it was 28 (93.33%). 2) Grade II: Eight cases(26.66%) were in grade 2 in conventional group and there was two cases (6.66%) in neuro-navigation group 3) Grade III: Grade III placement was observed in 2 cases in conventional group. Neuro-navigation group did not have any patient in this group.In present study of 60 cases, five patients had shunt infection and required removal of shunt. Two cases of conventionally placed shunt (grade 3) did not function well due to proximal obstruction and required shunt revision.(Table2)
| Sr. No. |
Number of patient
Convention Conventional Neuro-navigation
|
Percent |
| nfection |
2 3 |
8.3 |
| Obstruction |
2 2 |
6.66 |
| Over drainage |
2 1 |
5 |
| uncommon |
1
1 |
3.33 |
| malposition |
2 0 |
3.33 |
This study has several statistical limitations. The number of the samples was too small to represent the population of shunt patients. It was necessary to consider other factors that might have influenced the results. However, we tried to include patients who had various factors as possible. All factors except catheter tip position were already proven to have no statistical significance by using multiple regression analysis.
Discussion
According to the results of the previous studies, various methods have been suggested to improve the accuracy of catheter tip position. Pang and Grabbdescribed a method of calculating catheter length based on bony landmarks on skull radiographs and a shunt placement by free-hand passage using simple stereotactic guidance and palpable surface anatomy. Serlo et al. ascertained the catheter position using X-ray imaging by filling the catheter with contrast medium. [5] VP shunts are often complicated by malfunction, predom¬inantly with proximal catheter obstruction despite improved surgical equipment and operative skill. Frameless stereotaxy has been shown to be helpful for precise location of catheter tip and avoiding unnecessary injury to brain tissue, leading to prevent repeated shunt revisions in children with slit ventricles. [6,9] Choroid Choroid plexus has generally been considered to be the most frequent cause of ventricular catheter obstruction. It is well known that the ideal placement of the proximal catheter tip is the frontal horn away from the choroid plexus. The obstruction of catheter tip is caused by connective tissue, inflammatory changes, and foreign bodies which are found frequently at the ventricular end. Astrocytes and fibro-connective tissues are especially capable of proliferation. They may fill the side holes in the 15 mm from their tip and the inside of the catheter, leading to obstruction of the catheter. Choroid plexus and ependymal cells also have proliferative capability under certain conditions. Collins et al.frequently found choroid plexus in catheter tips placed in behind the foramen of Monro, but ependyma predominated in catheters placed in front of it. [5] A ventricular catheter tip surrounded by CSF decreased the risk of shunt failure to one-fifth, whereas a catheter tip touching the brain decreased the risk to one-third compared with a catheter tip surrounded by brain tissue. [4]Tai Hyoung Cho et al found proximal cerebrospinal fluid shunt malfunction due to ventricular catheter occlusion remains the most common source of the shunt problem. The position of the hole-bearing segment of the catheter affects the long term patency of the ventricular catheter of a cerebrospinal fluid shunt. Placement of this segment near the choroid plexus or injured ependyma increases the probability of obstruction. Accurate location of ventriculoperitoneal (V-P) shunt tip in relation to foramen Monro can be well established by plain radiography regardless of age or size and shape of head due to the fact that foramen Monro to the spatial matrix of the skull is constant. [10]Yamada SM et al. found that long-term maintenance of VP shunt function depends on the correct placement of the catheter tip in the lateral ventricle. The relationship between the location of the ventricular catheter tip and VP shunt function was analyzed in 52 patients. The location of the ventricular catheter tip was classified into one of the following five groups: (i) Group A--superior to the foramen of Monro; (ii) Group B--in the center of the lateral ventricle body; (iii) Group C--in the third ventricle; (iv) Group D--contacting the ventricle wall; and (v) Group E--in the septum pellucidum. [11]There are several disadvantages to frameless neuronavigation which include the prolongation of operation time and depen¬dence on expensive technology.6More operation time can have risk to increase intraoperative infection rate and other problem is that framelessstereotaxy is expensive. It requires additional imaging to be used for navigation with additional radiation dosage. It also adds cost to the procedure of neuronavi¬gation and to the use of a navigation stylet. [12] Therefore, the cost-benefit ratio must be carefully established to obviate its need. Wan KR reported that despite technological improvements, VP shunts are still complicated by malfunction, predominantly with proximal catheter obstruction. There is evidence that accurate placement of the ventricular catheter is significantly related to shunt survival. To identify possible risk factors that might lead to suboptimal shunt placement. Accurate placement of ventricular catheter is related with both proper insertion trajectory and proper catheter tip positioning. So recently, many studies have validated accuracy in VP shunt with the development of frameless neuronavigation in the field of neurosurgery. [4] Peter A. Woerdeman, et al. recommended that the use of an image-guided instrument holder is a simple modification of the free-handframeless stereotactic placement of ventriculoperitoneal shunts in undersized ventricles, preventing off-track deflection. This procedure is accurate and can be very useful inthe event of shunt-dependent undersized ventricles when lumboperitoneal shunting isconsidered to be contra-indicated. [13] Gil Z et al. found that the usage of a neuronavigation system is safe and may be beneficial for optimal positioning and trajectory of ventricular catheters in children with small ventricles or an abnormal ventricular anatomy. Frameless navigation is a valuable tool to optimize thetrajectory and final position of shunt catheter in children with small or slit ventricles. [6]This study has demonstrated that neuronavigation in the placement of ventricular catheter assures optimal catheter position within ventricles, reducing incidence of revision.
Conclusions
Frameless navigation is a valuable tool to optimize the trajectory and final position of shunt catheter in the ventricle. Neuronavigation has its own limiting factor like its cost and limited availability. Mechanical malfunction and infection are the most signifi¬cant problems associated with shunts for the treatment of hydrocephalus. Above all, a significant proportion of shunt failure was due to obstruction of the ventricular catheter, and accurate placement of the shunt catheter is highly important to reduce the incidence of shunt malfunction. In conclusion, the use of navigated system in routine shunt surgery can eliminate poor shunt placement resulting in a dramatic reduction in shunt revision rates.
Conflict of Interests
The authors declare that there are no conflicts of interests.
Authors’ Contribution
VS: Concept of study and final approval
DPT: Concept and analysis of study, literature search and preparation of manuscript
JR: Concept and design of study
Funding
Nil
Ethical Considerations
The study was approved by Institute Ethics Committee
Acknowledgement
None
References
[1].Pang D, Grabb PA. Accurate placement of coronal ventricular catheter using stereotactic co-ordinate guided free-hand passage.Technical note.J.Neurosurg.1994;80:750-5.[pubmed]
[2].Bierbrauer KS, Storrs BB, McLone DG, Tomita T, DauserR : A prospec¬tive, randomized study of shunt function and infections as a function of shunt placement. PediatrNeurosurg1990-1991;16 : 287-291.[pubmed]
[3].Serlo W, Heikkinen E, saukkonenAL,Von Wendt L. Classification and management of the slit ventricle syndrome. Child’s Nevr Syst.1985;1:194-199.[pubmed]
[4].Lazareff JA, Peacock W, Holly L, Ver Halen J, Wong A, Olmstead C : Multiple shunt failures : an analysis of relevant factors. Childs Nerv Syst.1998;14: 271-275.[pubmed]
[5].Tuli S, O’Hayon B, Drake J, Clarke M, KestleJ : Change in ventricular size and effect of ventricular catheter placement in pediatric patients with shunted hydrocephalus. Neurosurgery 1999;45 : 1329-1335.[pubmed]
[6].Wan KR, Toy JA, Wolfe R, DanksA : Factors affecting the accuracy of ventricular catheter placement. J Clin Neurosci.2011;18 : 485-488.[pubmed]
[7].Nayoung Jung, M.D., Dongwon Kim, M.D., Ph.D. Effect of Electromagnetic Navigated Ventriculoperitoneal Shunt Placement on Failure Rates J Korean Neurosurg Soc.2013; 53 : 150-154.[pubmed]
[8].Gil Z, Siomin V, Beni-Adani L, Sira B, Constantini S : Ventricular cathe¬ter placement in children with hydrocephalus and small ventricles : the use of a frameless neuronavigation system. Childs Nerv Syst.2002;18 : 26-29.[pubmed
[9].HaaseJ : Neuronavigation. Childs Nerv Syst.1999;15 : 755-757.[pubmed]
[10].Hakim S : Observations on the physiopathology of the CSF pulse and prevention of ventricular catheter obstruction in valve shunts. Dev Med Child Neurol Suppl.1969;20 : 42-48.[pubmed]
[11].Lazareff JA, Peacock W, Holly L, Ver Halen J, Wong A, Olmstead C : Multiple shunt failures : an analysis of relevant factors. Childs Nerv Syst.1998;14: 271-275.[pubmed]
[12].Tai Hyoung Cho, MD;JungYul Park, MD. Radiologic Location of Ventricular Tip and the Patency of Ventriculoperitoneal Shunt journal of korean neurosurgical society 1997; 26(4) : 513-7.
[13].Yamada SMet al. Relationship of the location of the ventricular catheter tip and function of the ventriculoperitoneal shunt. J ClinNeurosci.2013; 20(1):99-101.[pubmed]
[14]Byrne P, Clark S, Kandasamy J, et al. : Effect of electromagnetic-navigated shunt placement on failure rates : a prospective multicenter study. J Neurosurg.2010;113 : 1273-1278.[pubmed]
[15].Peter A. Woerdeman ,Peter W.A., Willems, Kuo S. Han et al frameless stereotactic placementof ventriculoperitoneal shuntsin undersized ventricles:a simple modification to freehand procedures ; British Journal of Neurosurgery.2005;19: 484 – 487.

