Case Report

Duodenal leiomyoma presenting with chronic melena
1Satyendra K Tiwary, 1A K Khanna
- 1Department of General Surgery Institute of Medical Sciences, Banaras Hindu University, Varanasi , 221 005
- Submitted: September 17, 2012
- Accepted: October 15, 2012
- Published: October 17, 2012
This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/3.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Introduction
Duodenal leiomyomas are rare neoplasms, and when present, are usually asymptomatic.
Case Report
We present a patient with leiomyoma arising from the first part of the duodenum who presented with melena for last 15 years and underwent local tumor excision with pyloroplasty.
Discussion
Most cases are detected incidentally either on radiological investigation or laparotomy or autopsy. It is extremely rare to detect by only presentation chronic melena.
Key Words
Duodenum, Leiomyoma, Pyroloplasty, Gastroduodenotomy, Bleeding, Benign, Neoplasms.
Introduction
Leiomyomas are benign neoplasms of smooth muscles. The most common site of leiomyoma is uterus and within the gastrointestinal tract, the commonest site of origin is the stomach. Duodenal leiomyomas are rare and usually asymptomatic. Abdominal pain, mass, obstruction, haematemesis or melena may be presenting feature in only small number of patients [1,2].
Diagnosis is made in most cases after Barium meal study or upper gastrointestinal endoscopy. The treatment of duodenal leiomyomas has been local tumor excision, segmental duodenal resection and pancreaticoduodenectomy [1-4]. A case of leiomyoma of the first part of the duodenum presenting with chronic melena who underwent local tumor excision and pyloroplasty is reported.
Case Report

Figure 1. Barium meal showing filling defect.
A 72 year male presented with recurrent melena and epigastric pain for 15 years. The patient required hospitalization several times & blood transfusion was needed. Upper gastrointestinal endoscopy showed duodenitis and Barium meal examination was normal. On the basis of history, clinical examination and endoscopic findings patient was treated with antibiotics and proton pump inhibitors for the chronic peptic ulcer. After several episodes of profuse melena needing blood transfusion and hospitalization, upper gastrointestinal endoscopy revealed polypoidal mass projecting into first part of the duodenum. Endoscopic biopsy was in favour of leiomyoma. Barium meal examination showed a filling defect in the second part of the duodenum (Figure 1). CT scan of abdomen showed a well differentiated homogenous soft tissue attenuating mass (7cm x 4cm x 4cm) in second part of the duodenum (Figure 2). The patient underwent local excision of tumor with pyloroplasty (Figure 3). On macroscopic examination, the resected specimen was 6cm x 4 cm x 4 cm (Figure 4) fleshy mass with smooth cut surface and arising from second part of the duodenum. Post operative period was uneventful. Histopathology was leimyoma of the duodenum. Presently he is well on a follow up of nearly two months.

Figure 2. CT scan showing heterogenous soft mass.
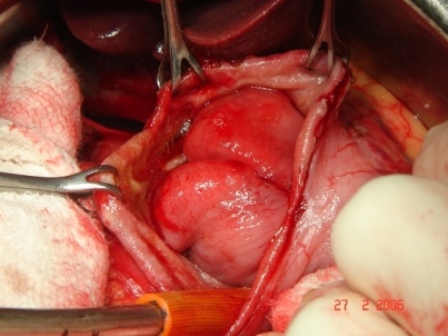
Figure 3. Leiomyoma exposed during surgery.
Discussion
Duodenal leiomyomas are extremely rare neoplasms and when present are usually asymptomatic but anemia, bleeding, and obstruction may be presenting feature [1-4]. Gastro-intestinal hemorrhage leads to melena commonly and hemetemesis rarely. Our patient presented with chronic melena for last 15 years but could not be diagnosed. It is quite unlikely to present with chronic melena in any other condition with such a long duration without any other complication e.g. obstruction, perforation. Epigastric tenderness may be present in some cases [4]. Upper gastro-intestinal endoscopy may reveal the lesion, but histopathological diagnosis is established in only 1/3 cases due to submucosal location of tumor [4]. Barium meal study is quite helpful in suggesting diagnosis for large duodenal leiomyomas visualized as filling defect in duodenum. Abdominal axial CT scan show hyperdense lesion in duodenum. It is very difficult to decide origin of mass in some cases by CT scan, as a large no of structures are situated in adjoining region e.g pancreas, gallbladder, bile duct, portal vein, superior mesenteric artery.

Figure 4. Resected leiomyoma.
In cases with short duration of symptoms, leiomyosarcoma should also be considered in differential diagnosis. Treatment of duodenal leiomyoma is excision once diagnosis is suspected or settled. Small tumors are quite amenable to duodenotomy and local tumor excision. Large tumors may need segmental duodenectomy and duodeno-duodenal anastomosis with sparing of pancreas [5]. Despite benign nature of the lesion, some cases may require pancreaticoduodenectomy (Whipple Procedure) if pancreas or ampulla of vater is involved or there is any suspicion of malignancy [1-3]. Our case was treated with modified technique of local tumor excision. Gastroduodenotomy was performed to expose the tumor as it was located in second part of the duodenum. Closure was done with pyloroplasty after local exision of tumor. Pyloroplasty was required due to gastroduodenal incision and for prophylaxis of gastric outlet obstruction.
Advantages of this technique over classical whipple’s for malignancy are less operating time, less blood loss, less morbidity and techniquely less demanding. So for leiomyomas of proximal duodenum, gastroduodenotomy with local tumor excision and pyloroplasty should be recommended as treatment of choice.
Authors' Contribution
SKT: Did the literature search, prepared the draft manuscript.
AKK: Concept, design and review.
Acknowledgement
None
Funding
None
References
[1]. Blanchard DK, Budde JM, Hatch GF 3rd, Wertheimer-Hatch L, Hatch KF, Davis GB, Foster RS Jr, Skandalakis JE Tumors of the small intestine. World J Surg 2000; 24: 421 -9.[Pubmed]
[2]. Serraf A, Klein E, Schneebaum S, Davidson B, Herzig E, Ben-air G. Leiomyoma of the duodenum. J Surg Oncol 1988; 39: 183 – 6.[Pubmed]
[3]. Dasrathy S, Pandey GK, Bhargava DK, Gupta SS, Gupta SD. Gastrointestinal leiomyomas in a developing country. Trop Gastroenterol 1995; 16: 43 – 6.[Pubmed]
[4]. Rice DC, Bakeen F, Farley DR, Unni KK, Van Heerden JA.Surgical management of duodenal leiomyomas. World J Surg 2001; 25: 562-6.[Pubmed]
[5]. Yadav TD, Sinha S, Kaushik R. Pancreas sparing duodenectomy for leiomyoma of the third part of duodenum. A case report. Indian J Surg 2004; 66:171–3.

