Case Report

Isolated CNS Nocardiosis in an Immunocompetent Patient
Ahmad Alwassia, Bhanu K. Patibandla, Anthony Bartley, Vinod Chaubey MD1
1 Department of Medicine / Saint Vincent Hospital, Worcester, Massachusetts
Submitted June 27, 2013
Accepted July 26, 2013
Published: September 7, 2013
This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/3.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract:
Introduction
Nocardiosis is typically regarded as an opportunistic infection; risk factors For developing Nocardiosis include Diabetes, HIV infection (especially if CD4 count is <100), glucocorticoid therapy, transplantation, and malignancy (most often after recent hemotherapy). However; about one third of patients are immunocompetent; here, we present a case of Nocardiosis in an immunocompetent patient.
Case presentation
A 69 year old female with past medical history of COPD, Invasive ductal carcinoma of breast presented with progressive left sided weakness and headaches of one week duration. Initial evaluation was significant for left sided weakness in the upper and lower extremities along with left sided facial droop. CT brain without IV contrast revealed a ring enhancing mass measuring 2.4 mm * 2.8 mm in the right basal ganglia with significant adjacent edema, effacing the right lateral and third ventricles, and 2 mm leftward midline shift. Stereotactic biopsy of the brain mass identified it as an abscess and histology revealed acute and chronic inflammatory cells with no viable tissue. Gram stain and culture showed aerobic branching gram-positive organisms, which were later identified as Nocardia Farcinica.
Discussion
Although Nocardial brain abscess generally occurs in immunosupressed hosts, they were also reported in immunocompetent individuals. In immunosuppressed patients, involvement of the CNS should be ruled out even without neurologic symptoms.
Key Words
Nocardia Farcinica, Abscess, brain,
Introduction
Nocardiosis is an uncommon bacterial infection caused by the gram positive aerobic actinomyces with the genus Nocardia. Infection with Nocardia is typically regarded as an opportunistic infection; however; about one third of patients are immunocompetent [1-3].
Nocardia species are found in soil, decaying vegetable matter, aquatic environments, and can become airborne, particularly in dust particles [2-5]. Inhalation of the organism is thought to be the most common mode of entry [1-5].
In a previously reported literature review, 64% of patients diagnosed with Nocardiosis were immunocompromised [5-6]. Risk factors for developing Nocardiosis include: Diabetes, HIV infection (especially if CD4 count is <100), glucocorticoid therapy, transplantation, and malignancy (most often after recent chemotherapy) [7]
Pulmonary Nocardosis is regarded as the most common type of primary infection. Isolation of Nocardia from sputum samples is almost always indicative of an infection [4]. Nocardia species have a trophism for the central nervous system [3, 6]. In a previously reported retrospective report of 1050 cases of Nocardosis, CNS involvement occurred in 20% of overall cases and in 44% who had disseminated disease. Isolated CNS involvement can occur, however this most likely represents resolved pulmonary and/or skin infection [1]. The following report presents a case in which Isolated CNS involvement occurred with apparently no primary site of infection.
Case report
A 69 year old female with past medical history of COPD, Invasive ductal carcinoma of the breast which is ER+ve and HER-2 –ve treated with lumpectomy (3 years ago), radiation, and anastrozole therapy presented with progressive left sided weakness and headaches of one week duration.
At the time of initial evaluation, she was afebrile and her vitals were stable. She denied any fevers or chills, dyspnea, cough, and any recent sinus or dental infection. She denied any chronic glucocorticoid therapy, and stated that she did not receive any steroids for COPD over the last 8 years. On physical examination, oral cavity and sinuses were unremarkable. Significant left sided weakness was appreciated in the upper and lower extremities (3/5 compared to 5/5 on the right side) along with left sided facial droop. Laboratory investigations, which included complete blood count and basic metabolic panel, were unremarkable. Chest X-ray showed no acute cardiopulmonary pathology. CT brain without IV contrast revealed a ring enhancing mass [Fig 1] measuring 2.4 mm * 2.8 mm in the right basal ganglia with significant adjacent edema, effacing the right lateral and third ventricles, and 2 mm leftward midline shift. She was started on Decadron to relieve cerebral edema and Keppra for seizure prophylaxis.

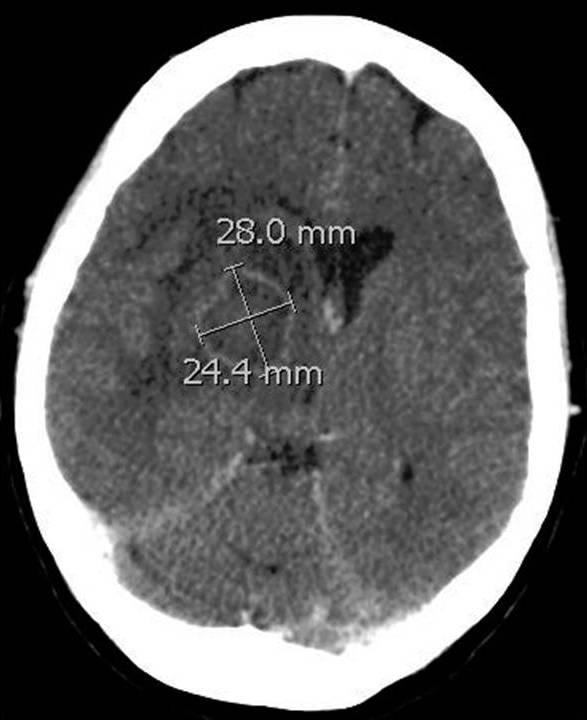
Figure 1 CT scan of brain without IV contrast: A 24.4mm by 28 mm ring enhancing mass is highlighted in the figure. Note the hypodense region surrounding the mass, which represent edema. A leftward midline shift can also be appreciated on this figure.
Stereotactic biopsy of the brain mass identified it as an abscess. Histological evaluation revealed acute and chronic inflammatory cells with no viable tissue. Gram stain and culture showed aerobic branching gram-positive organisms, which were later identified as Nocardia Farcinica. Sputum and blood remained negative for any growth. The patient was treated with IV Bactrim.
She remained clinically stable throughout her hospital course and herneurological deficits gradually improved. A repeat CT brain showed a decrease in the edema previously noted. She later developed hyponatremia, which in the setting of a brain abscess was most likely secondary to SIADH; her serum and urine osmolality were indeed consistent with the diagnosis of SIADH. The patient was placed on water restriction, and it was noted that the IV Bactrim was mixed in D5W, which was later changed to normal saline. Her serum sodium returned to baseline in a few days.
Discussion
Nocardia species can cause localized or disseminated infection that usually affects immunocompromised patients. Patients with AIDS, patients with prior solid organ and hematopoietic stem cell transplantation, hematologic and solid organ malignancies, and chronic systemic steroid use [8-9]. The lungs are the primary source of infection in more than 40% of cases. In most patients, disseminated nocardiosis is from the lung and frequently affected the CNS. Although a nocardial brain abscess generally occurs in immunosupressed hosts, they were also reported in immunocompetent individuals [10-13]. In immunosuppressed patients, involvement of the CNS should be ruled out even without neurologic symptoms [8]. Nocardial abscesses may present as an isolated brain lesion, but are usually multiple [8-9, 14].
Hematogenous spread from the lungs is presumed to be the primary mechanism for the development of CNS nocardiosis. Nocardial pulmonary disease is the predominant clinical presentation of this infection, with more than 40% of reported cases presenting with findings in the lungs [13,15]. Mortality rates have been reported to be as high as 78% with any nocardia species pulmonary infection and up to 90% in patients who present with CNS involvement [12-13].
The patient in this case developed isolated CNS nocardiosis with no apparent primary source of infection. There might have been a transient mild pulmonary illness when the patient first acquired the infection; the pulmonary infection likely resolved or was clinically undetectable at the time CNS infection was detected. The patient has a history of COPD, which may have placed her at greater risk of developing the infection. She was did not receive any systemic steroid for her COPD in the past 8 years. In addition, the patient does have a history of breast cancer, which according to previous reports does place her at higher risk for developing an infection with Nocardiosis [8].
Conclusion
Isolated CNS Nocardiosis can occur in immunocompetent patient.
It is important to consider Nocardia when evaluating CNS abscesses.
Clinically, a primary source of infection may not always be detectable.
Conflict of Interest
None
Consent
Consent could not be obtained as the patient unfortunately had expired.Exemption was obtained from IRB.
Author’s contributions
All the authors were involved in the patient’s care. AA and BKP have written the case report. AB and VC participated through literature search and editing.
Acknowledgements
None
References
[1]. Lerner PI. Nocardiosis. Clin Infect Dis 1996; 22:891.[pubmed]
[2].. Brown-Elliott BA, Brown JM, Conville PS, Wallace RJ Jr. Clinical and laboratory features of the Nocardia spp. based on current molecular taxonomy. Clin Microbiol Rev 2006; 19:259.[pubmed]
[3]Beaman BL, Beaman L. Nocardia species: host-parasite relationships. Clin Microbiol Rev 1994; 7:213.[pubmed]
[4].Lederman ER, Crum NF. A case series and focused review of nocardiosis: clinical and microbiologic aspects. Medicine (Baltimore) 2004; 83:300.[pubmed].
[5]. Sorrel TC, Mitchell DH, Iredell JR, Chen SC-A. Nocardia Species. In: Principles and Practice of Infectious Diseases, 7th ed, Mandell GL, Bennett JE, Dolin R (Eds), Churchill Livingstone Elsevier, Philadelphia 2010. p.3199.
[6]McNeil MM, Brown JM. The medically important aerobic actinomycetes: epidemiology and microbiology. Clin Microbiol Rev 1994; 7:357. [pubmed]
[7]Peleg AY, Husain S, Qureshi ZA, et al. Risk factors, clinical characteristics, and outcome of Nocardia infection in organ transplant recipients: a matched casecontrol study. Clin Infect Dis 2007; 44:1307.[pubmed]
[8]Alijani N, Mahmoudzadeh S, Hedayat Yaghoobi M, Gerami shoar M, Jafari S. Multiple brain abscesses due to Nocardia in an immunocompetent patient. Arch Iran Med. 2013; 16(3): 192 – 194.[pubmed]
[9]Ambrosioni J, Lew D, Garbino J. Nocardiosis: Updated clinical re- view and experience at a tertiary center. Infection.2010; 2: 89 – 94.[pubmed]
[10]Fellows GA, Kalsi PS, Martin AJ : Nocardia farcinica brain abscess in a patient without immunocompromise. Br J Neurosurg 21 : 301-303, 2007[pubmed]
[11]Fleetwood IG, Embil JM, Ross IB : Nocardia asteroides cerebral abscess in immunocompetent hosts : report of three cases and review of surgical recommendations. Surg Neurol 53 : 605-610, 2000.[pubmed]
[12]Malincarne L, Marroni M, Farina C, Camanni G, Valente M, Belfiori B, et al. : Primary brain abscess with Nocardia farcinica in an immune-competent patient. Clin Neurol Neurosurg 104: 132-135, 2002[pubmed][pubmed]
[13]Joung Mk et al. Concurrent Nocardia Related Brain Abscess and Semi-Invasive Pulmonary Aspergillosis in an Immunocompetent Patient. J Korean Neurosurg Soc 49 : 305-307, 2011[pubmed]
[14]Khan BA, Duncan M, Reynolds J, Wilkes DS. Nocardia infection in lung transplant recipients. Clin Transplant. 2008; 22(5): 562 – 566[pubmed]
[15]Hui CH et al. Pulmonary nocardiosis re-visited: experience of 35 patients at diagnosis. Respir Med. 2003; 97(6): 709 – 717.[pubmed]

