Case Report

Solitary extrapleural fibrous tumor of axillary skin diagnosed by fine-needle aspiration cytology, coincident with simultaneous breast fibroadenoma
Yuichi Kinoshita1,2, Kosho Takasu3, Naoki Hosaka4, Naoto Omura5, Takashi Yuri1, Yuko Emoto1, Katsuhiko Yoshizawa1, Airo Tsubura1, Nobuaki Shikata1
1Department of Pathology II, Kansai Medical University, Osaka, Japan 2Division of Diagnostic Cytopathology and Histopathology, Kansai Medical University Takii Hospital, Osaka, Japan.
3Division of Surgical and Cytopathology, Hyogo Prefectural Amagasaki Hospital, Hyogo, Japan
4Department of Diagnostic Pathology, Kansai Medical University Kori Hospital, Osaka, Japan
5Department of Radiology, Kansai Medical University Kori Hospital, Osaka, Japan
This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/3.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Background
Solitary fibrous tumor (SFT) is a rare mesenchymal tumor that usually occurs in pleura, or less commonly, in the extrapleural space (extrapleural SFT).
Case presentation
Here, we report on an extrapleural SFT originating from the right axilla that occurred at about the same time as a fibroadenoma of the right breast in a 37-year-old woman. The patient noticed stiffness in her right axilla; neoplastic masses were detected in her right breast and axilla using ultrasonography. Cytology from a fine needle aspiration biopsy showed oval-to-spindle-shaped atypical cells with ropy fragments from the axilla; the sample was diagnosed as extrapleural SFT. The breast tumor was diagnosed as fibroadenoma.
Discussion
Cytological reports of extrapleural SFT are few. Future case accumulation could provide data on which to base guidelines for discerning benign from malignant SFT.
Key words
Extrapleural solitary fibrous tumor, fine needle aspiration biopsy cytology, fibroadenoma of breast, case report
Introduction
Solitary fibrous tumor (SFT) is a mesenchymal tumor derived from fibroblasts, and was first described by
Klemperer et al. in 1931 [1]. SFT occurs mainly in the lungs, and only rarely as an extrapleural lesion [2]. Extrapleural SFT is classified as an intermediate (rarely metastasizing) fibroblastic/myofibroblastic tumor [3]. However, some reports find SFTs of distinctly malignant character regardless of location [4–6] and opinion is often divided about classification. Furthermore, cytologic reports for SFT are few. We herein report a case of an extrapleural SFT of the right axilla with fibroadenoma of right breast occurring at the same time.
Case presentation
Clinical findings The patient is a 37-year old woman who consulted the Department of Breast Surgery at Kansai Medical University Kori Hospital with a chief complaint of stiffness of her right axilla. Partly marginal inarticulate echo-poor regions in the AC areas of the right breast and axilla (9.9 × 15.1 × 18.5 mm and 16.2 × 33.0 × 37.0 mm in size respectively) were observed by ultrasonography (Figure 1). Fine-needle aspiration (FNA) biopsy cytology was then performed. Malignancy was diagnosed and tumors in the right breast and axilla tumor were resected. FNA was not performed for the breast tumor before surgery. Currently, the patient has been followed up as an outpatient in the six months after surgery, and shows no sign of recurrence or metastasis.
Cytologic findings
For cytologic examination, FNA material was prepared directly and immersed in 95% ethanol. The needle washing sample was centrifuged at 3000 rpm for 5 minutes. The pellet smear was spray fixed using Rapid Spray Gas Free (Muto Pure Chemicals, Tokyo, Japan), and then immersed in 95% ethanol for Papanicolaou staining. Microscopic examination revealed tumor cells with a high nucleus/cytoplasm ratio (include bare nucleii) oval-to-spindle-shaped atypical cells which showed prominent anisonucleosis and increased fine granular chromatin as loose clusters or isolated cells. Vascular-like arrangements and thick collagenous fibers were seen as clusters. Nucleoli were small and mitosis was not found. Cytoplasm was observed as micro-vacuolated with unclear cellular border (Figure 2A–C). Immunocytochemically, tumor cells were positive for vimentin and negative for pan-cytokeratin (Figure 2D). The axillar tumor was cytologically similar to the soft tissue tumor in the right breast.
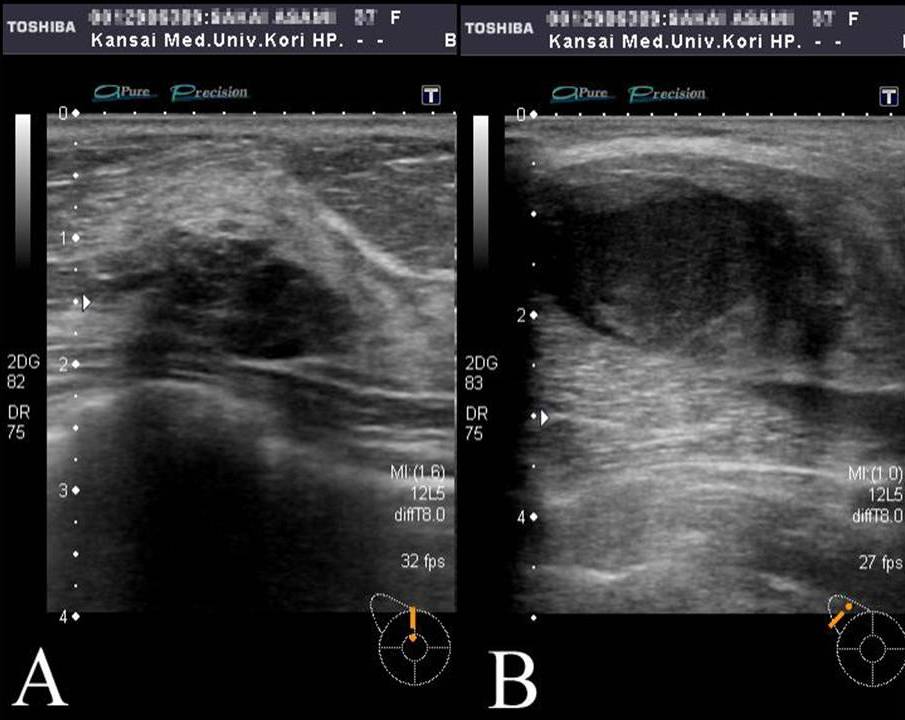
Figure 1. Ultrasound findings. (A) A–C region of the right breast has internal nonuniform low echogram with unclear borders. (B) Right axilla shows internal nonuniform low echogram region.
Pathologic findings
Macroscopic examination revealed a light yellow mass with an unclear margin on the cut surface of the axillar tumor (Figure 3). Histologically, the tumor cells showed oval-to-spindle shapes,solid anisocytosis and a partly hemangiopericytoid pattern with a few collagen-like stroma. Cytologically, the tumor cells had prominent atypical nuclei and small nucleoli. In addition, 4–5 mitoses were observed per 10 high-power fields. The tumor invaded to muscle tissue (Figure 4A, B), but necrosis was not noticeable. Immunohistochemically, tumor cells were positive for vimentin, CD34, and CD99 (Figure 4C), and negative for pan-cytokeratin, CD117 (c-kit), S-100 protein, α-smooth muscle actin, and Factor VIII. The Ki67 labeling index was about 10%. The breast tumor was diagnosed as fibroadenoma with a clear border (Figure 5), whereas the axillar tumor, occurring at the same time, was a malignant extrapleural SFT.
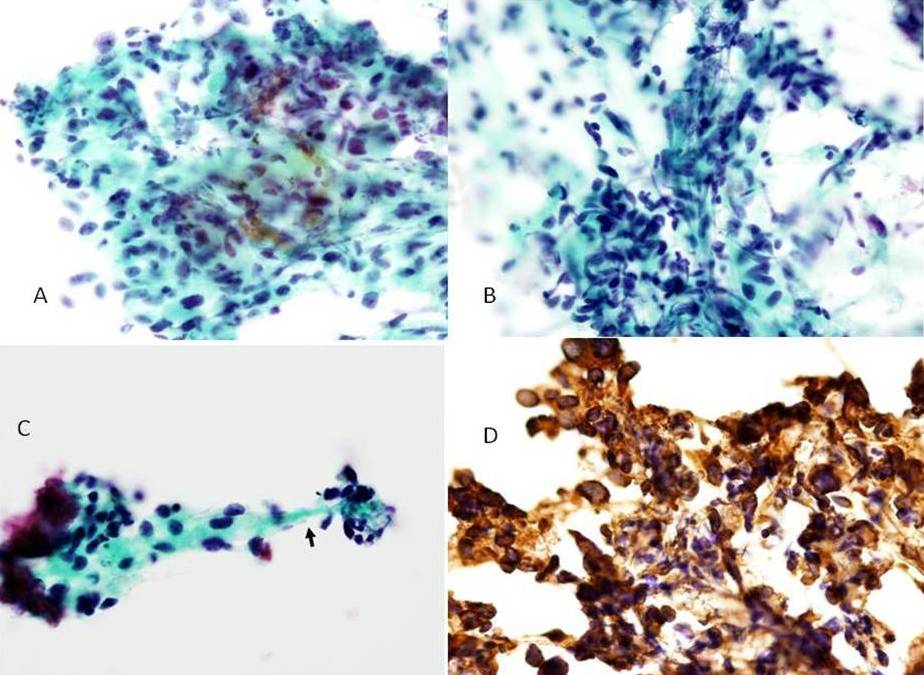
Figure 2. Malignant solitary fibrous tumor cells of right axilla from fine-needle aspiration cytology. (A) Neoplastic cells with moderately atypical nuclei, fine granular chromatin and small nucleoli. (B) Vascular-like structure. (C) Neoplastic cells with ropy collagenous material (Papanicolaou staining ×400). (D) Neoplastic cells were positive for vimentin (immunocytochemical staining ×400).
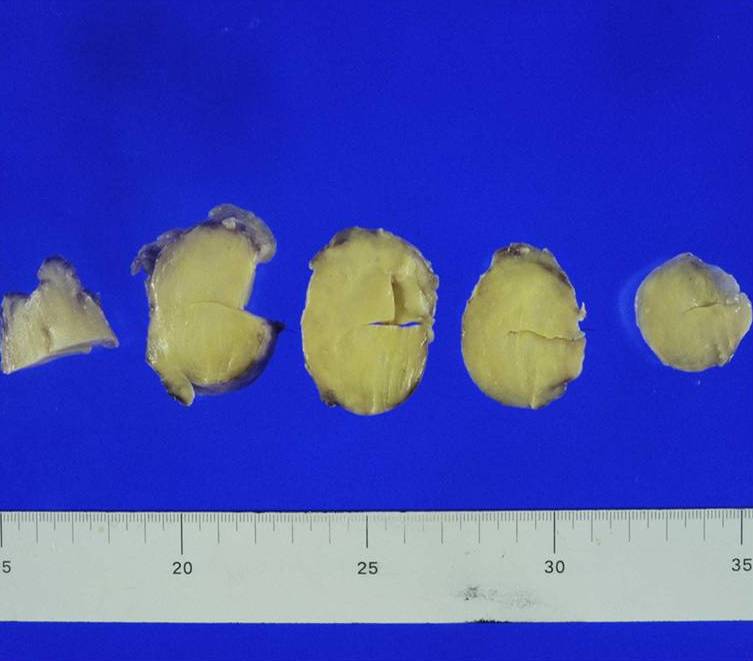
Figure 3. Gross findings. Cut surface of tumor is circumscribed and light yellow.
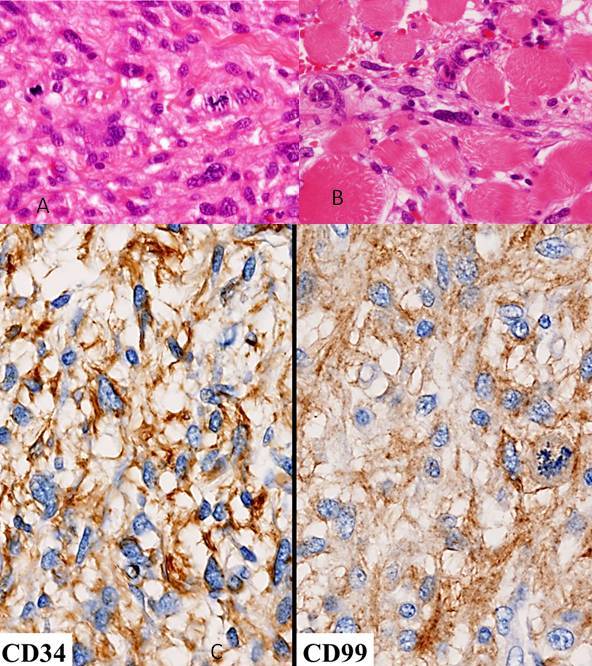
Figure 4. (A) Tumor cells proliferated in a “patternless pattern” with collagen-like stroma. Mitoses were occasionally seen (HE staining ×400). (B) Tumor cells invade to muscle (HE staining × 400). (C) Tumor cells were positive for CD34 and CD99 (immunohistostaining ×400).

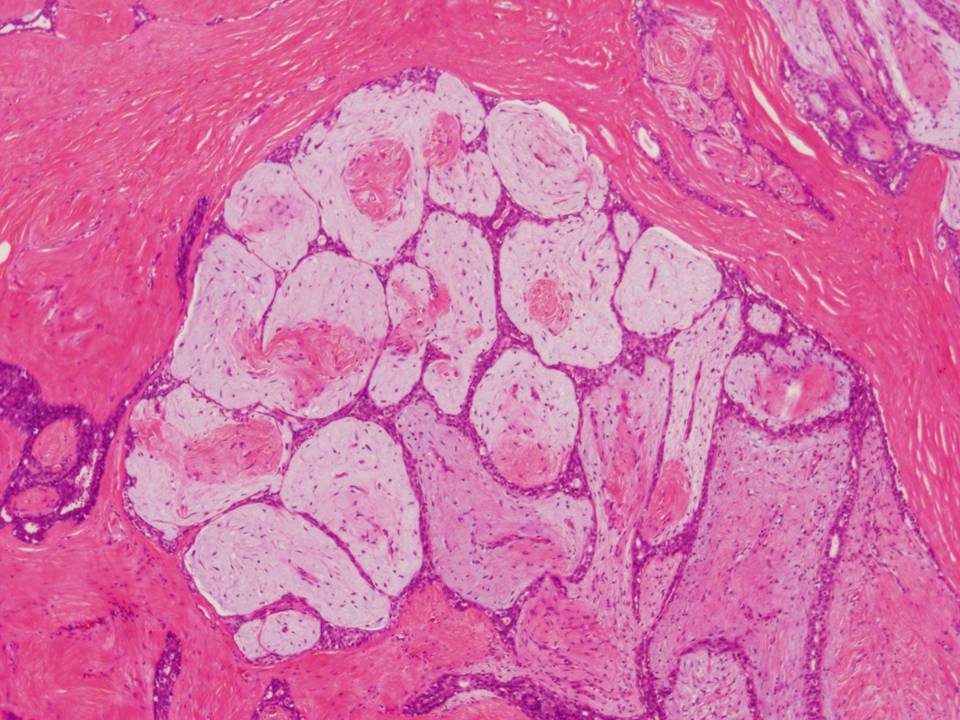
Figure 5. Fibroadenoma of the breast lesion (HE staining ×20).
Discussion
Extrapleural SFTs are uncommon mesenchymal neoplasms that occur ubiquitously, such as in subcutaneous tissue, soft tissue of limbs, orbit, chest wall, mediastinum, cardiac sac, retroperitoneum, abdominal cavity, meninges, spinal cord, periosteum, lungs, mammary floor, thyroid, liver, intestine, adrenal, bladder, prostate, spermatic cord and testis. They are most frequently observed in adults of 20–70 years [3, 7–11]. Histologically, although SFT reportedly shows a hemangiopericytoma-like vascular growth pattern, it does not usually have a characteristic growth pattern (so-called patternless pattern) [2, 3]. Immunohistochemically, the tumor cells are reportedly positive for D34 (90–95% of cases), CD99 (70% of cases), EMA (20–35% of cases) and bcl-2 (20–35% of cases), but negative for cytokeratin [2, 3]. Histologic and immunohistologic differences are not seen in each organ [7–11]. Differential diagnosis of morphology may include high-grade sarcoma and malignant fibrous histiocytoma, but differentiation is possible because both these tumor types are negative for CD34. Generally, criteria for malignant SFT include (a) high cellularity, (b) moderately atypical cells, (c) high rate of mitotic figures (4 per 10 high-power fields), and (d) invasion and/or distinct necrosis [2, 3, 6]. Guo et al. (2008) added the Ki-67 labeling index as a criterion of malignancy (benign SFT: 2–10%; malignant SFT: 15–30%) [5]. A case of malignant SFT was thus reportedly diagnosed from Ki-67 labeling index results [9]. However, in our case, the Ki-67 labeling index was 10%; necrosis was not found and 4–5 mitotic figures were seen per 10 high-power fields. Invasion to muscle tissue was also observed in this present case. We therefore comprehensively diagnosed it as malignant SFT.
Cytological findings of SFT includes (a) round-to-oval, moderately atypical cells, (b) increased fine-grained chromatin, (c) absent or barely noticeable nucleoli, (d) irregular ropy fragments of background collagen, and (e) pale and unclear cytoplasm [11–13]. Although benign and malignant differentiation is difficult to discern through morphology, Ali et al. (1997) pointed out that polymorphism and dyskaryosis of tumor cells are characteristic cytologic findings for malignant SFT [14]. He also noted that the nucleolus is not observed in benign SFT [14]. In the present case, this tumor satisfied these criteria for SFT and strongly atypical nuclei and nucleoli were observed. Thus, we finally diagnosed this tumor as malignant SFT. However, as the breast tumor was not diagnosed preoperatively, we initially confused the diagnosis of the axillary tumor.
Conclusion
Although SFT should be followed up carefully, local recurrence and/or metastasis is rarely present in SFT. Although accurate diagnosis by FNA cytology is important, studies of SFT cytology are limited. Establishment of cytological criteria based on case accumulation, to help discern benign from malignant SFT, is a worthwhile goal.
Authors’ contributions
All authors contributed equally.
Conflict of Interests
None.
Ethical Considerations
Written consent was obtained from the patient for publication of this case report.
Funding
None.
Acknowledgement
None.
References
[1] Klemperer P, Rubin CB. Primary neoplasm of the pleura: a report of five cases. Arch Pathol. 1931;11:385–412.
[2]Travis WD, Chung A, Aubry MC, et al. Mesenchymal tumours. In: Travis WD, Brambilla E, Müller-Hermelink, Harris CC, editor. World Health Organization Classification of Tumours, Pathology and Genetics of Tumours of the Lung, Pleura, Thymus and Heart. Lyon: IARC Press; 2004; p.141–144.
[3]Guillou L, Fletcher JA, Fletcher CDM, Mandahl N. Extrapleural solitary fibrous tumor and haemangiopericytoma. In: Fletcher CDM, Unni KK, Mertens E, editor. World Health Organization Classification of Tumours, Pathology and Genetics of Tumours of Soft Tissue and Bone. Lyon: IARC Press; 2002; p. 86–90.
[4]Yan XJ, Wang YA, Zhu HG, et al. Malignant solitary fibrous tumor of the head and neck: a clinicopathological study of nine consecutive patients. Oral Oncol. 2009;45:678–682.[pubmed] [pubmed]
[5]Guo W, Xiao HL, Jiang YG, et al. Retrospective analysis for thirty-nine patients with solitary fibrous tumor of pleura and review the literature. World J Surg Oncol. 2011; 9:134. [pubmed][pubmed]
[6]Vallat D, Anne V, Dry SM, Fletcher SDM. Atypical and malignant solitary fibrous tumors in extra-thoracic locations: evidence of their comparability to intra-thoracic tumors. Am J Surg Pathol. 1998;22:1501–1511.[pubmed][pubmed]
[7]Rovera F, Imbriglio G, Limonta G, et al. Solitary fibrous tumor of the male breast: a case report of the literature. World J Surg Oncol. 2008; 6:16.[pubmed][pubmed]
[8]Erbag G, Qureshi HS, Patterson JW, Wick MR. Solitary fibrous tumor of the skin: a clinicopathologic study of 10 cases and review of the literature. J Cutan Pathol. 2007;34:844–850.[pubmed][pubmed]
[9] Soldano AC, Meehan SA. Cutaneous solitary fibrous tumor: a case report of 2 cases and review of the literature. Am J Dermatopathol. 2008;30:54–58.[pubmed][pubmed]
[10]Senteusanio G, Schiaroli O, Ortenzi A, Mulè A, Perrone G, Fadda G. Solitary fibrous tumor of thyroid: report of two cases with immunohistochemical features and literature review. Head and Neck Pathol. 2008;2:231–235.[pubmed][pubmed]
[11]Baliga M, Flowers R, Heard K, Siddiqi A, Akhtar I. Solitary fibrous tumor of the lung: a case report with study of the aspiration biopsy, histopathology, immunohistochemistry and autopsy findings. Diagn Cytopathol. 2007;35:239–244.
'[
12]Clayton AC, Salomão DR, Keeney GL, Nascimento GL. Solitary fibrous tumor of six cases diagnosed by fine-needle aspiration. Diagn Cytopathol. 2001;25:172–176.[pubmed]
[pubmed]
[13]Parwani AV, Galindo R, Steinberg DM, Zeiger MA, Westra WH, Ali SZ. Solitary fibrous tumor of the thyroid: cytopathologic findings and differential diagnosis. Diagn Cytopathol. 2003;28:213–216.[pubmed][pubmed]
[14]Ali SZ, Hoon V, Hoda S, Heelan R, Zakowski M. Solitary fibrous tumor. A cytologic-histologic study with clinical, radiologic, and immunohistochemical correlations. Cancer Cytopathol. 1997;81:116–121.
[pubmed][pubmed]

