Case Report

Primary Meningeal Melanocytoma: A Rare Case Diagnosed on Fine Needle Aspiration Cytology
1Adarsh Barwad, 1Nalini Gupta, 1Arvind Rajwanshi, 2Pravin Salunke
- 1Department of Cytology and Gynecological Pathology, Postgraduate Institute of Medical Education and Research, Chandigarh
- 2Department of Neurosurgery, Postgraduate Institute of Medical Education and Research, Chandigarh
- Submitted: February 22, 2013;
- Accepted March 14, 2012
- Published: March 15, 2012
This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/3.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Introduction
Primary meningeal melanocytoma is a benign central nervous system neoplasm derived from melanocytes. This mostly occurs within the posterior fossa, cerebellopontine angle and the pineal body.
Case Report
An 80-year-old male presented with headache and swelling over left temporal region since six months. Contrast enhanced computerized tomography (CECT) revealed a large lobulated enhancing soft tissue density mass lesion in the left temporal region with overlying bone erosion and destruction with soft tissue component in left temporal fossa. FNAC smears were highly cellular and showed tumor cells predominantly in syncytial clusters and dispersed forming vague whorls with interspersed cells containing abundant black melanin pigment. The individual cells exhibited minimal nuclear atypia, with round to oval nuclei and moderate to abundant cytoplasm with cytoplasmic projections. Cell block showed similar cytological features with prominent whorling and abundant melanin pigment. The diagnosis of pigmented melanocytoma was offered which was further supported by immunochemistry.
Conclusion
The present case is the first report of melanocytoma diagnosed on FNAC to the best of our knowledge. Detailed cytomorphological features and differential diagnosis of this rare entity are discussed.
Keywords
Fine needle aspiration cytology, Primary meningeal melanocytoma.
Introduction
Primary melanocytic neoplasms are the rare neoplasms of the central nervous system (CNS) which arise from melanocytes of the leptomeninges [1]. The various entities in this include diffuse leptomeningeal melanocytosis (DLM) or melanomatosis, melanocytoma and primary malignant melanoma. Primary meningeal melanocytoma is a benign CNS neoplasm derived from melanocytes, and was first reported by Limas et al in 1972 [2]. This tumor can have aggressive behavior and frequent relapses [3-6]. Fine needle aspiration cytology (FNAC) has been widely used for diagnostic purposes especially for palpable lesions. FNAC in this tumor is rarely described in literature [7, 8]. We present a case which was diagnose on FNAC and subsequently confirmed on immunochemistry.
Case Report
An 80-year-old male presented with headache and swelling over left temporal region since six months. Patient also complains of left retro-orbital pain. Contrast enhanced computerized tomography (CECT) revealed a large lobulated enhancing soft tissue density mass lesion measuring 37x28x72mm in the left infratemporal region extending intracranially into the basitemporal region and orbital apex on the left side and left periinsular region. There was evidence of destruction of superior wall of left orbit and left temporal bone with periosteal new bone formation and cortical destruction. Magnetic resonant imaging (MRI) revealed a lobulated T2 hyperintense and T1 iso-hypointense lesion centered in left sphenoid triangle with extension into left temporal fossa, inferior orbital fissure, left cavenus sinus, middle cranial fossa as well as with lateral zygomatic, subcutaneous and ethmoid sinus extension (Figure 1). Radiological possibility of malignant neoplasm of bone was suggested and patient was referred for FNAC from the palpable swelling in the left temporal region.
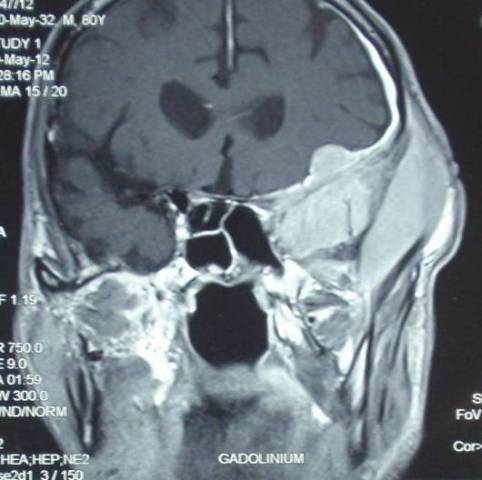
Figure 1- Magnetic resonant imaging (MRI) showing a lobulated lesion in the left sphenoid triangle with extension into left temporal fossa, inferior orbital fissure, left cavernous sinus, middle cranial fossa as well as with lateral zygomatic, subcutaneous and ethmoid sinus extension
Fine needle aspiration (FNA) was performed using 23 G needle from left temporal swelling and the aspirate was collected for cell block preparation along with both air-dried and alcohol fixed smears.
Cytological features: FNAC smears were highly cellular and showed tumor cells predominantly in syncytial clusters and dispersed forming vague whorls with many tumor cells containing abundant black pigment. Per vascular arrangement was noted focally. The individual cells showed minimal nuclear pleomorphism, oval to spindle nuclei and moderate to abundant cytoplasm. The nuclei were vesicular with finely granular chromatin and few conspicuous nucleoli. Intra-nuclear inclusions were seen. The cytoplasm was dense and many cells showed long cytoplasmic processes. Admixed, there were few polygonal cells containing abundant intra-cytoplasmic black colored melanin pigment (Figure 2a & 2b). There was no significant atypia, increased in mitosis or necrosis.
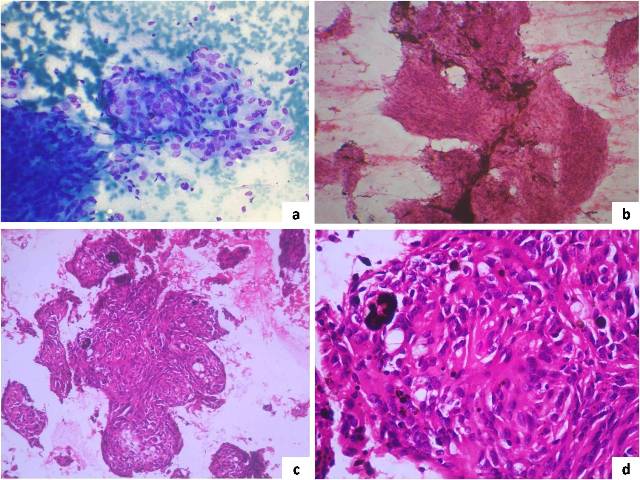
Figure 2- Panel showing a case of meningeal melanocytoma; 2a- Syncytial clusters of oval shaped tumor cells forming whorls (MGGx40X); 2b- Highly cellular tumor with tumor cells showing abundant melanin pigment (H&E x20X); 2c- Cell block showing whorled appearance of tumor cells (H&E x20X); 2d- Cell block showing syncytial tumor clusters with cells containing abundant black pigment (H&E x40X).
Cell block showed similar tumor cells arranged predominantly in syncytium, whorling and at places in perivascular pattern (Figure 2c & 2d). The individual cells were monomorphic with oval to elongated nuclei, fine dispersed chromatin, and inconspicuous nucleoli with moderate to abundant eosinophilic cytoplasm. There were scattered tumor cells and macrophages containing abundant intra-cytoplasmic melanin pigment. Immunochemistry was performed on cell block showed tumor cell immuno-reactive for S-100 and HMB-45. Tumor cells were negative for epithelial membrane antigen (EMA).
Discussion
Primary meningeal melanocytoma is a benign CNS neoplasm derived from melanocytes, and was first reported by Limas et al., in 1972 on electron microscopy examination of heavily pigmented foramen magnum tumor by observing melanosomes and premelanosomes in the neoplastic cells [2]. Although the exact cause of the disease remains unclear, however, melanocytmas are supposed to be derivative of leptomeningeal melanocytes and mostly occur within the posterior fossa, cerebellopontine angle and the pineal body [4, 9-11]. Embryological studies available in literature suggest that melanocytes originate from the neural crest of the epidermis and leptomeninges [3, 4, 9]. Primary meningeal melanocytoma are rarely located in anterior cranial fossa [12-14]. Melanocytomas are usually dura-based tumors, usually solitary, circumscribed, dark brown to black colored, and can be locally invasive [8].
Melanocytomas are usually diagnosed on histological examination and there are occasional case reports in literature describing the cytological features of this rare tumor [7, 8]. Chen et al., had described the cytological features in crush tumor and Kini et al., in intra-operative imprint smears however there is no report in literature where tumor was diagnosed preoperatively using FNAC as diagnostic modality. FNAC is widely used as diagnostic and staging modalities for various tumors worldwide and in the present case, the diagnosis was made solely on FNAC assisted with cell block preparation.
Cytologic features of the tumor in the present case were similar to those described by Kini et al., however in the present case whorling arrangement was more conspicuous. Perivascular arrangement on smears was focally evident as compared to those described in crush smear by Chen et al., [7]. Psammoma bodies were not observed on smears in the present case. Many tumor cells showed long cytoplasmic processes. Pigment containing cells were unevenly distributed and were extensive at places as described in earlier study [8]. The cytomorphology was further supported by cell block preparation which revealed similar nuclear features and additional architectural features for confirming the diagnosis in present case. Further immunochemistry supported the diagnosis and helped to exclude differential diagnostic entities.
Melanocytoma is a rare tumor and hence one must be aware of the light microscopic feature of this tumor both on cytologic smears and histologic examination. This is pigmented lesion and hence the differential diagnosis includes pigmented CNS tumors such as melanotic schwannoma, melanotic meningioma, melanotic medulloblastoms, melanotic ependymoma and also malignant melanoma [8]. Malignant melanoma can be easily excluded as melanocytoma lacks nuclear atypia, mitotic activity, apoptosis and necrosis. Medulloblastoma usually has the morphology of malignant small round cell tumor and is mitotically active tumor. Ependymoma is in differential for the melanocytoma occurring at spinal location and can be excluded considering radiologic and cytologic feature assisted by immunochemistry.
The closest differential diagnosis in the present case was melanotic schwannomas which can be difficult and challenging [15]. However, the schwannoma shows plump to spindle cells with nuclear kinking embedded in pink fibrillary background. Nuclei are hyper chromatic and some may show degenerative pleomorphism and hyperchromasia particularly in long standing case [8]. Fascicular arrangement of tumor cells is more evident in schwannoma. Verocay bodies may be observed in schwannoma [16]. Also, radiologically, schwannoma are well-circumscribed.
Conclusion
We present a case of melanocytoma which was diagnosed pre-operatively on FNAC along with cell block preparation. Knowledge of cytologic features of this tumor is essential for cyto pathologists for diagnosis of this rare entity.
Consent
Written informed consent was obtained from the patient for publication of this case report in World Journal of Medical and Surgical Case reports. A copy of the written consent is available for review with authors.
Authors' contributions
AB: He has been involved in drafting this manuscript after reviewing a lot of literature.
NG: She has reported this case on cytology and was involved in revising the manuscript critically for important intellectual content.
AR: He has provided pictures for this manuscript and has given final approval of the version to be published.
PS: He is the clinician in-charge for this case and he has operated upon this patient later on.
All authors have read and approved the final manuscript.
Each author has participated sufficiently in the work to take public responsibility for appropriate portions of the content.
Conflict of Interests
The author(s) declare that they have no competing interests.
References
[1]. Virchow R. Pigment und diffuse Melanose der Arachnoides. Virchows Arch. 1859;16:180–2.
[2]. Limas C, Tio FO. Meningeal melanocytoma ("melanotic meningioma"). Its melanocytic origin as revealed by electron microscopy. Cancer. 1972;30:1286-94 [Pubmed].
[3]. Clarke DB, Leblanc R, Bertrand G, Quartey GR, Snipes GJ. Meningeal melanocytoma. Report of a case and a historical comparison. J Neurosurg. 1998;88:116-21 [Pubmed].
[4]. Liubinas SV, Maartens N, Drummond KJ. Primary melanocytic neoplasms of the central nervous system. J Clin Neurosci. 2010;17:1227-32 [Pubmed].
[5]. Wang F, Qiao G, Lou X, Song X, Chen W. Malignant transformation of intracranial meningeal melanocytoma. Case report and review of the literature. Neuropathology. 2011;31:414-20 [Pubmed].
[6]. Perrini P, Caniglia M, Pieroni M, Castagna M, Parenti GF. Malignant transformation of intramedullary melanocytoma: case report. Neurosurgery. 2010;67:E867-9; discussion E9 [Pubmed].
[7]. Chen KT. Crush cytology of melanocytoma of the spinal cord. A case report. Acta Cytol. 2003;47:1091-4 [Pubmed].
[8]. Kini JR, Jeyraj V, Jayaprakash CS, Indira S, Naik CN, Rao D. Intraoperative smear cytology of meningeal melanocytoma of the posterior fossa. Cytopathology. 2009;20:59-62 [Pubmed].
[9]. Ali Y, Rahme R, Moussa R, Abadjian G, Menassa-Moussa L, Samaha E. Multifocal meningeal melanocytoma: a new pathological entity or the result of leptomeningeal seeding? J Neurosurg. 2009;111:488-91 [Pubmed].
[10]. Prabhu SS, Lynch PG, Keogh AJ, Parekh HC. Intracranial meningeal melanocytoma: a report of two cases and a review of the literature. Surg Neurol. 1993;40:516-21 [Pubmed].
[11]. Czirjak S, Vitanovic D, Slowik F, Magyar A. Primary meningeal melanocytoma of the pineal region. Case report. J Neurosurg. 2000;92:461-5 [Pubmed].
[12]. Kawaguchi T, Kawano T, Kazekawa K, Nakashima S, Honma T, Kaneko Y, et al. Meningeal melanocytoma in the left frontal region. Brain Tumor Pathol. 1998;15:58-62 [Pubmed].
[13]. Uozumi Y, Kawano T, Kawaguchi T, Kaneko Y, Ooasa T, Ogasawara S, et al. Malignant transformation of meningeal melanocytoma: a case report. Brain Tumor Pathol. 2003;20:21-5 [Pubmed].
[14]. Hino K, Nagane M, Fujioka Y, Shiokawa Y. Meningeal melanocytoma associated with ipsilateral nevus of Ota presenting as intracerebral hemorrhage: case report. Neurosurgery. 2005;56:E1376; discussion E [Pubmed].
[15]. Brat DJ, Giannini C, Scheithauer BW, Burger PC. Primary melanocytic neoplasms of the central nervous systems. Am J Surg Pathol. 1999;23:745-54 [Pubmed].
[16]. Cummings TJ, Liu K, Jordan LK, 3rd, Dodd LG. Fine-needle aspiration diagnosis of psammomatous melanotic schwannoma. Diagn Cytopathol. 2000;23:55-8 [Pubmed].

