Case Report

A unusual case of dislocation of the Foot: A case report
Tomas Belzunegui
- Emergency department, Health Service of Navarre, Navarre, Pamplona, Spain
- Submitted: February 23, 2013;
- Accepted: April 06, 2013;
- Published: April 08, 2013
This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/3.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Sub-talar dislocations are rarely seen in emergency practice and account for approximately 1% of all dislocations and 15% of all talus injuries. Open dislocations are even rarer. The sub-talar dislocation consists of a dislocation of the talar-calcaneus and talar-schaphoid joints. They may be medial or lateral dislocations depending on the position of the foot. We present a case of a 39 year old male with a medial open subtalar dislocation after falling from a one metre height. Early reduction is fundamental to avoid pain and limitation in movement of the subtalar joint in the long term.
Case Report
Open subtalar dislocations are very rare and usually involve high energy mechanisms. Prompt management is required to attain a favorable long term function.
A 39 year old man presented to the emergency department after a work related injury. The patient accidentally fell from a height of approximately 1 metre, with all his weight supported on the left foot while simultaneously producing a twisting motion and inversion of the same foot. This mechanism produced a medial dislocation according to Brocas classification: the deformation of the foot resulted from medial displacement of the calcaneus and scaphoid, while the talus was displaced laterally, its head producing a dorsolateral prominence.
The force of the inversion produced the rupture of the talar-scaphoid and talar-calcaneus joints, in addition to the internal displacement of the whole foot. The talus usually dwells in the mortise cavity though its neck can rotate around the minor apophasis of the calcaneus that acts as a support. When the talar-scaphoid and the sub-talar joints dislocate, the talus moves to a lateral position.
On arrival to the emergency department the patient’s foot was found in the position as shown in figure 1. The figure shows the characteristic deformity of a medial sub-talar dislocation, with a dorsolateral protrusion of the head which just tears the skin leaving it exposed. No abnormalities were found after a doppler exploration of posterior tibial and pedial pulses nor was there any neurological compromise.

Figure 1: The high energy forced inversion of the foot causes talus dislocation leaving the talar head exposed (arrow).
Radiological studies carried out are shown in figure 2

Figure 2: Lateral radiograph of the ankle showing medial displacement of the calcaneus and the tarsal bones while the talus remains in its position (arrow).
The patient's diagnosis was described as a type II Gustilo open medial peri-talar dislocation of the left foot and he was admitted for emergency surgery. The surgical intervention included thorough lavage and debridement, reduction of the dislocation and reconstruction of soft tissue, ligament suture and the Friedrich method was applied to manage the open wound. Intravenous antibiotics were administered for 7 days (genatamycin and metronidazole) and immobilization with a short-leg posterior plaster splint was carried out for 4 weeks. Results of the reduction are shown in figure 3.
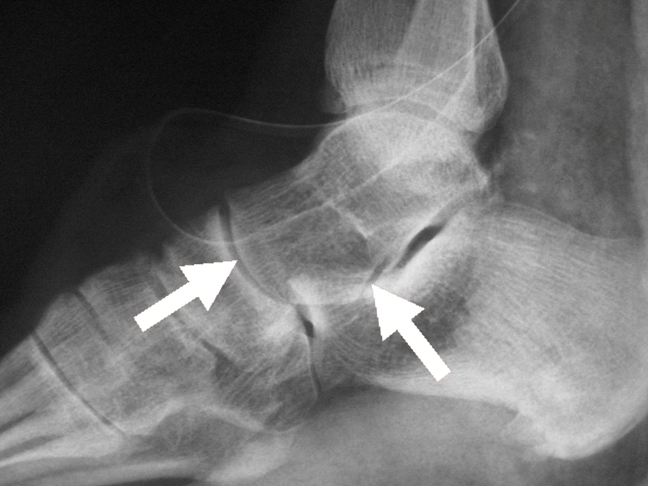
Figure 3: After surgical intervention the dislocation was reduced leaving the talar-calcaneus joint in its normal position (arrow).
The edges of the wound suffered necrosis but healed satisfactorily with no complications. The patient was discharged after 28 days and began walking on his foot after 2 months. Follow up was carried out after 6 and 12 weeks and the patient could walk with no limitation though he complained of mild discomfort when walking on irregular terrain.
Sub-talar dislocations, also known as peri-talar dislocations consist of a dislocation of the talar-calcaneus and talar-schaphoid joints. It is therefore a double dislocation. They may be medial or lateral dislocations depending on the position of the foot. In medial dislocations the head of the talus is displaced laterally while the calcaneus is displaced medially. Both the tibio-fibula-talar and calcaneo-cuboid joints remain intact. The foot is dislocated below the astragalus which remains within the bimaleolar ring. It was first described in 1811 by Judcy and Dufaurets [1, 2].
This rare entity accounts for approximately 1% of all dislocations and 15% of all astragalus injuries. It affects mainly young males (6:1). Open dislocations are even more rare (between 10 and 40%) and are mostly caused by high energy impacts [3, 4].
Patients in which an early reduction is carried out present a favourable clinical course, with mild symptoms in the long term. Some limitation and pain may remain in movements of the subtalar joint, with difficulty in walking on irregular ground [5, 6].
A computed tomography (CT) scan of the ankle and foot should be considered to evaluate any other articular fractures and soft tissue injuries after reduction [7].
Some authors opt for the use of external fixation to allow for an earlier movement of the foot [8, 9]. In our case, early reduction and surgery offered a satisfactory and functional result.
Conflict of interest
The authors declare that there are no conflicts of interests
Author’s Contributions
TB Did the literature search and prepared the manuscript
Ethical consideration
Written consent was obtained from the patient for publication of this case report
Funding
None declared
Acknowledgement
None
References
[1]. DeLee JC, Curtis R. Subtalar dislocation of the foot. J.Bone Joint Surg.Am. 1982 Mar;64(3):433-437. [Pubmed].
[2]. Bohay DR, Manoli A,2nd. Subtalar joint dislocations. Foot Ankle Int. 1995 Dec;16(12):803-808. [Pubmed].
[3]. Goldner JL, Poletti SC, Gates HS,3rd, Richardson WJ. Severe open subtalar dislocations. Long-term results. J.Bone Joint Surg.Am. 1995 Jul;77(7):1075-1079. [Pubmed].
[4]. Huang PJ, Fu YC, Tien YC, Lin GT, Lin SY, Cheng YM, et al. Open total talar dislocation--report of two cases. Kaohsiung J.Med.Sci. 2000 Apr;16(4):214-218. [Pubmed].
[5]. Naranja RJ,Jr, Monaghan BA, Okereke E, Williams GR,Jr. Open medial subtalar dislocation associated with fracture of the posterior process of the talus. J.Orthop.Trauma 1996;10(2):142-144. [Pubmed].
[6]. Palomo-Traver JM, Cruz-Renovell E, Granell-Beltran V, Monzonis-Garcia J. Open total talus dislocation: case report and review of the literature. J.Orthop.Trauma 1997 Jan;11(1):45-49. [Pubmed].
[7]. Sharda P, DuFosse J. Lateral subtalar dislocation. Orthopedics 2008 Jul;31(7):718. [Pubmed].
[8]. Milenkovic S, Radenkovic M, Mitkovic M. Open subtalar dislocation treated by distractional external fixation. J.Orthop.Trauma 2004 Oct;18(9):638-640. [Pubmed].
[9]. Milenkovic S, Mitkovic M, Bumbasirevic M. External fixation of open subtalar dislocation. Injury 2006 Sep;37(9):909-913. [Pubmed].

