Case Report

Neglected Antero- Inferior Dislocation of Hip Treated With Primary Reverse Hybrid THR- A Rare Case Report
1Dr. Kiran S. Patil, 2Dr. Deepesh Daulatni, 2Dr. Monish Bami, 2Dr. Mallikarjun Ithli
- 1Associate Professor, Department of Orthopaedics, BLDEU’S SHRI B.M. Patil Medical College, Bijapur
;
- 2Post- Graduate, Department of Orthopaedics, BLDEU’S SHRI B.M. Patil Medical College, Bijapur
- Submitted: December 10, 2013
- Accepted: December 14, 2013
- Published: January 05, 2014
This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/3.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Introduction
Antero-inferior dislocation of hip is a rare disease with not much literature regarding the reporting and management modalities of this type of dislocation. We here present a case of neglected antero-inferior dislocation of hip.
Case report
We present a case of 25 year old male patient who presented with history of trauma 1 year back fixed flexion deformity of 40 degrees and abduction deformity of 20 degrees of the hip with apparent lengthening of affected limb. Patient did not take any medical treatment but has a history of massage and prolonged immobilization. Patient reported to us one year later with deformities of lower limb. Patient was walking with support of a stick and was unable to squat, sit cross legged and his activities of daily living hampered. X-ray and MRI confirmed antero-inferior dislocation of hip with indentation of femoral head and features suggestive of signs of avascular necrosis of femoral head. Weight bearing dome of acetabulum was flattened. Primary hybrid THR with cementless femoral component and cemented acetabular component was done.
Conclusions
The patient is walking independently with full range of motion at the hip at 1 year of follow up and able to perform all activities of daily living independently.
Keywords
neglected, antero-inferior, hybrid THR, hip dislocation
Introduction
The hip joint is inherently stable, requiring significant force to dislocate. Thus pure hip dislocation or dislocation with femoral head fracture is generally a result of high-energy trauma and is often accompanied by associated injuries[1]. Dislocations of the hip are classified as anterior or posterior according to the position of the femoral head. Anterior dislocations have been further sub-classified as superior, inferior, and luxatio erecta of hip, obturator and pubic type [2,3]. Anterior dislocations of the hip are less common than posterior type, comprising 10-15% of all hip dislocations [4]. For the hip to dislocate, the ligamentum teres and at least a portion of the capsule must be disrupted. Labral tears or avulsions and muscular injury are common. In anterior dislocations the psoas acts as the fulcrum of the hip and the capsule is disrupted anteriorly and inferiorly. Although rare, in extremely high-energy injuries the femoral vessels can be injured or an open dislocation can occur. The initial management for almost all hip dislocations is an attempt at a closed reduction. The reduction should be considered an emergent procedure1. Interposition of soft tissues, including the rectus femoris and iliopsoas muscles and the torn hip capsule, and a “buttonhole” entrapment of the femoral head by the capsule are potential obstructions to reduction5. We here present a case of neglected antero-inferior dislocation of hip.
Case Report
A 25 year old male patient presented with history of trauma 1 year back for which he did not take any medical treatment but massage and prolonged immobilization was done. The patient was on complete bed rest for three months. After three months the patient was walking with the help of a stick but was unable to squat and sit cross-legged. The activities of daily living were hampered and the patient was unable to carry on with his job.
On presentation, there was apparent lengthening of the right lower limb of 7 cm and true lengthening of 5 cm with a fixed flexion deformity of 400 and fixed abduction deformity of 200(Figure 1).


Figure 1- Preoperative clinical pictures showing the deformities
Radiological evaluation was done in the form of X-ray and MRI. X-ray of the pelvis with both hip joints (Figure 2) showed inferior dislocation of the femur with features suggestive of avascular necrosis of the head of the femur and flattening of the weight bearing dome of the acetabulum. MRI (Figure 3) showed a similar picture with conformation of antero-inferior dislocation of hip. The patient was advised total hip replacement and all pre-operative investigations were within normal limits.

Figure 2: X-ray of pelvis with both hips showing inferior dislocation of right hip
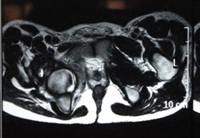
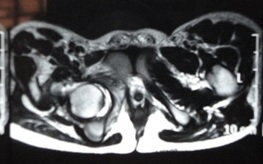
Figure 3- MRI showing hip dislocation.
For the surgical procedure, lateral position and posterior approach was used. Intra-operatively the head of femur and acetabulum were both devoid of the cartilage, their weight-bearing surfaces were damaged and the cavity was filled with fibrous tissue. After adequate preparation of the acetabulum and femoral shaft, reversed hybrid total hip replacement was done. The patient was started on static and active quadriceps exercises post-operatively after anesthesia wore off.
The suction drain was removed on 3rd post-operative day and patient advised assisted walking with the help of a walker. Post-operative period was uneventful and the sutures were removed on 12th post-operative day. The patient was advised not to squat and sit cross-legged. The patient was followed up at 3 weeks, 6 weeks, 3 months, 6 months and a year. Post-operative radiograph was taken at 3 weeks (Figure 4). The patient was advised ROM exercises for the knee and ankle along with quadriceps strengthening exercises. Patient was also advised walking as pain tolerated by the patient. At the end of one year the patient is walking independently without any pain with full range of motion (Figure 5) at the hip joint and a Harris Hip Score of 92 at final follow-up.

Figure 4- Postoperative radiograph showing the implant.


Figure 5- Showing Postoperative range of movement.
Discussion
Hip dislocations are quite rare due to the anatomy of the hip joint: the acetabular cavity is deep and the surrounding ligamentous structures are strong. Anterosuperior dislocations are identified as subspinous, suprapubic or pubic dislocations and anteroinferior dislocations as obturator, perineal or thyroid dislocations [6]. Anterior dislocations of the hip are less common than posterior type, comprising 10-15% of all hip dislocations,and inferior dislocation is the most common type of anterior dislocation, comprising more than 70% of anterior dislocations. The lower incidence of anterior dislocation may be due in part to the strong anterior capsule and Y-shaped ligament of Bigelow, which is a strong disincentive to anterior dislocation [7].
Anterior hip dislocations can be associated with femoral neurovascular injury, femoral head fractures, and acetabular fractures [1,5]. Early reduction of the dislocated joint is necessary to reduce the risk of avascular necrosis, which is seen in 0-5% if the hip is reduced in less than six hours after the injury versus in 50% if the hip is reduced more than six hours after the injury [8]. It has been well documented that delayed reduction of traumatic dislocation of the hip increases the risk of avascular necrosis and arthritis. In view of these poor results, Garrett [9] suggested total hip replacement as the treatment of choice.
Avascular necrosis is the most severe complication that may develop following a traumatic hip dislocation, and it is an indication of bad prognosis. Development of avascular necrosis has been reported to range from 3% to 58% following the traumatic hip dislocations [10]. Among leading factors are advanced age of the patient, delayed time to reduction, severity of the trauma and presence of fractured dislocations [11].
Many treatment modalities for reduction of the dislocated hips are present. In the acute stages closed reduction is an emergency procedure. In cases where closed reduction fails, open reduction is the treatment of choice. Studies on neglected anterior/antero-inferior dislocation are few in number. In a series published by Agarwal N.D.[12], seven patients were treated for anterior dislocation of hip in which trochanteric osteotomy was done in five cases, open reduction and arthroplasty in one each of the patients which showed trochateric osteotomy to give good functional and serviceable hips.
Singaravadivelu et al [13] reported a case of neglected intra-pelvic dislocation of hip which was reported after three months with a FFD of 300 and a small defect of the inferior aspect of the medial wall of acetabulum. The patient was treated with cemented total hip replacement and had good results at 2 year follow-up.
In a study done by Alva et al[14] , they performed a girdlestone arthroplasty in a case of 5 month old unreduced anterior dislocation. In our case, since the acetabulum and femoral head were both devoid of cartilage and the patient, being the sole bread winner of the family, requested for a stable, pain free hip with good range of motion for his work, a decision to perform a total hip replacement was taken. At the end of one year, the patient is walking independently, without any pain and has near normal range of motion. In conclusion, for neglected cases with changes of avascular necrosis of femoral head and acetabular changes, total hip replacement provides a good option for treatment.
Conclusions
Neglected cases of hip dislocation can have devastating complications and early diagnosis and treatment of these can prevent an early replacement. In cases where the patient comes with a neglected dislocation treatment by total hip replacement can give a functional and stable hip.
Learning points
-
Neglected cases of the hip occur in a developing country and a high index of suspicion is needed.
-
MRI of the affected hip is needed for knowing the status of the cartilages and associated acetabular changes.
-
Primary THR gives good results in such cases.
Conflict of interests
There are no competing interests.
Author’s Contributions
KP, DD and MI were the primary operating surgeons. MB designed and made the study.
Funding
None
Acknowledgements
Authors acknowledge the immense help received from the scholars whose articles are cite and include in references of this manuscript. The authors are also grateful to authors/editors/publishers of all those articles journals and books from where the literature for this article has been reviewed and discussed.
Ethical Considerations
References
[1] Bucholz Robert W., Heckman James D., Court-Brown Charles M. Rockwood & Green's Fractures in Adults, 6th Edition. Philadelphia, Lippincott Williams & Wilkins; 2006; Vol (2): p1714-1752.
[2] Phillips AM, Konchwalla A. The pathologic features and mechanism of traumatic dislocation of the hip. Clin Orthop Relat Res 2000;377:7-10.[pubmed]
[3] Epstein HC. Traumatic dislocations of the hip. Clin Orthop Relat Res 1973;92:116-42.[pubmed
[4] DeLee JC, Evans JA, Thomas J. Anterior dislocation of the hip and associated femoral-head fractures. J Bone Joint Surg Am 1980;62:960-4.[pubmed]
[5] Canale Terry S., Beaty James H. Campbell's Operative Orthopaedics, 11th ed. Philadelphia, Mosby Elvesier 2007; vol(3):p3227-3296.
[6] Aggarwal S., Kumar V., Bhagwat K., Shashikanth V.S., Ravikumar H. Inferior dislocation of the hip: a case series and literature review. Chinese J of Traumatology 2012;15(5):317-320. [Full text]
[7] DeLee JC, Evans JA, Thomas J. Anterior dislocation of the hip and associated femoral-head fractures. J Bone Joint Surg Am 1980;62:960-4.[pubmed
[8] Phillips AM, Konchwalla A. The pathologic features and mechanism of traumatic dislocation of the hip. Clin Orthop Relat Res 2000;377:7-10.[pubmed]
[9] Garret JC, Epstein HC, Harris WH, Harvey JP, Nickel VL. Treatment of unreduced traumatic posterior dislocations of the hip. J Bone Joint Surg 1979;61-A: 2-6.[pubmed]
[10] Salisbury RD, Eastwood DM. Traumatic dislocation of the hip in children. Clin Orthop Relat Res 2000;(377):106-11.[pubmed]
[11] Yamamoto K, Ko M, Masaoka T, Shishido T, Imakiire A. Traumatic anterior dislocation of the hip associated with ipsilateral femoral shaft fracture in a child: a case report. J Orthop Surg 2004;12:126-32.[pubmed]
[12] Agarwal N.D., Singh H. Unreduced anterior dislocation of hip. A report of seven cases. JBJS 1967;49(B):288-92.[pubmed]
[13] Singaravadivelu V, Mugundhan M, Sankaralingam K. Neglected intrapelvic dislocation of femoral head. Indian J of Orthopaedics 2010;44:224-26. [Full text]
[14] Alva A, Shetty M, Kumar V. Old unreduced traumatic anterior dislocation of the hip. BMJ case reports 2013; doi:10.1136/bcr-2012-008068. [Pubmed]

