Case Report

Mesenchymal Tumours of the Liver in Children: Report of Four Cases
1,Hemonta K Dutta 1Mauchumi Baruah
- 1Pediatric Surgery, Govt. of Assam, Assam, Dibrugarh, Assam, India
- Submitted Thursday, June 12, 2014
- Accepted:Friday, July 25, 2014
- Published Sunday, August 03, 2014
This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/3.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited
Abstract
Mesenchymal tumours are rare in children. They can be benign tumours like mesenchymal hamartoma or a malignant mesenchymoma. Mesenchymal hamartoma of the liver usually presents as an asymptomatic abdominal mass or abdominal distension. We are presenting four children who presented with mesenchymal tumours of liver, 3 of them had benign mesenchymal hamartomas and one had malignant mesenchymoma. Their clinical presentation, operative findings and post-operative outcome is discussed along with review of relevant literature.
Key-words
Mesenchymal hamartoma; liver; tumor; malignant mesenchymoma
Introduction
Primary liver tumours are rare in childhood and are either epithelial or mesenchymal in origin. Two thirds of these tumours are malignant. Mesenchymal hamartoma (MH) is a benign tumour of the liver usually presents with an painless abdominal mass [1]. Over two thirds are encountered in children under one year of age and 20% occur in neonates [2]. Malignant mesenchymoma is a rare malignant mesenchymal tumour of the liver, usually affects older children between 6 to 10 years of age. We report 4 children with mesenchymal tumours of liver with review of relevant literature. Three of these patients had MH and one had malignant mesenchymoma of the liver.
Case History
Three children, aged 2 months, 10 months, and 3 years respectively presented with lump abdomen of 2 to 3 months duration. In the second child, the mass was big enough to reach the pelvis. None of the patients had history of weight loss or fever during this period. In all the patients, the mass arose from the liver, had smooth surfaces and lobulations. On ultrasonography the mass arose from the left lobe in 2 patients and from the right lobe in one patient. The characteristic solid and cystic components were present in all the cases. Contrast CT scan showed well delineated masses arising from segments II,III & IV in 2 patients (Figure 1). and the mass replaced segments VI, VII & VIII and part of segment V in the third patient. Examination of blood, liver function test and serum alpha-fetoprotein levels were within normal limits in all of them. Left hepatic lobectomy was performed in two and right hepatic lobectomy was done in one patient. The tumours weighed 320 gms, 180 gms and 750 gms respectively. Cut section of tumours showed typical honeycomb appearances (Figure 2). Histology showed cystic and solid component with well differentiated ductal structures surrounded by loose mesenchyme containing fibroblast and confirmed the diagnosis of MH (Figure
3). All the three patients had uneventful recovery and have been on regular follow up for 80, 54 and 32 months respectively.

Figure 1: CT scan showing mesenchymal hamartoma in the left lobe of the liver

Figure 2: Cut section of the tumour shows typical honeycomb appearance
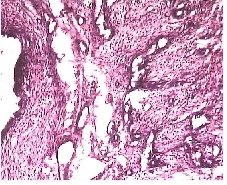
Figure 3: Photomicrograph of mesenchymal hamartoma shows ducts lined by low cuboidal epith., cystic spaces with loose connective tissue stroma
(H & E stain x 100)
The fourth patient was a 6 years old boy presented with a rapidly enlarging mass in the abdomen, loss of appetite and weight loss (> 3kg) of 2 months duration. The abdomen was distended with the mass arising from the liver, mostly on the right side and extending upto the level of the umbilicus. The mass was firm, had smooth surface, slightly tender and moved with respiration. Contrast CT of the abdomen showed a hypovascular, well demarcated mass arising from the right lobe of the liver with areas of necrosis(Figure 4). Abdominal glands were not enlarged. Chest x-ray was normal. Serum ∞-fetoprotein level was normal. Right hepatectomy was performed. Histology confirmed the tumour as malignant mesenchymoma (Figure 5). The patient received 3 cycles of chemotherapy, but died of progressive disease 2 months later.

Figure 4: CT scan of malignant mesenchymoma showing hypovascular, well demarcated tumour with areas of necrosis
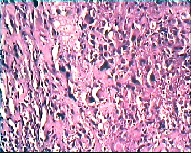
Figure 5: Photomicrograph (H & E stain x100) showing highly pleomorphic cells, some round to oval,others spindle shaped with pleomorphic and bizzare nuclei with occasional multinucleation and giant nuclei suggesting malignant mesenchymoma.
Discussion
MH of the liver is the second commonest benign liver tumor in children less than two years of age. Two thirds of the tumours present within the first year of life; 20% occur in neonates and may have postnatal growth spurt due to rapid accumulation of fluid.[2 3]. The child usually presents with an asymptomatic abdominal lump, but may have unusual symptoms such as, respiratory distress, vomiting or weight loss. MH commonly involves the right lobe (75%), usually multiloculated, and often pedunculated[2]. Rarely it can be multicentric. Liver function tests are usually normal. Occasionally, serum alpha-fetoprotein may be elevated [2]. Ultrasonography shows the typical predominantly cystic transonic mass with solid septa [4]. Contrast CT shows characteristic peripheral hypervascularity [5]. Histologically, there is a mixture of mesodermal and endodermal structures in a loose connective tissue stroma and fluid filled spaces which lacked an endothelial lining. In the 3 patients, the tumours were confined to the lobe of origin and had both solid and cystic elements. The characteristic honey comb appearance was evident on cut section of the tumours. Isaacs reviewed 45 cases of MH from the literature over a period of 35 years. The author reported fatal complications associated with this tumor, ie, fetal hydrops, respiratory distress, and circulatory problems owing to a large space occupying abdominal lesion and sometimes stillbirth, all contributing to the death rate [2].
Etiologically, MH may develop because of ductal plate malformation, vascular insult, toxic injury, or may be neoplastic.[1 2 6]. The ultrastructural appearance of MH contains well differentiated ductal structures surrounded by loose mesenchyme with fibroblast [7]. Okeda proposed a pathogenetic relationship with defective vascularisation, but cytogenetic studies have suggested that the tumor may be a neoplasm rather than a hamartoma [8].
Most tumours gradualsly increase in size, some reaching enormous proportions, which can make surgery challenging. Paradoxically, a few undergo incomplete spontaneous regression and, on rare occasions, others have shown malignant transformation to undifferentiated (embryonal) sarcoma [3]. These unusual pathological and biological features must be taken into account when considering the management of affected children.
Malignant Mesenchymoma is a highly malignant tumour of the liver in children. First described by Stout in 1948, it usually occurs between 6 and 10 years of age and presents with abdominal lump, pain and fever [9,10]. Ishak described the typical appearance of this tumour as a large solitary mass, mostly arising from the right lobe of the liver, well demarcated from surrounding liver, multicystic and mucoid in appearance [11]. Unlike other liver tumours, which are hypervascular on angiography, mesenchymomas are hypovascular [12]. Histologically, this tumour is characterized by large areas of necrosis along with sarcomatous cells showing frequent mitosis. Cysts are lined by single layer of endothelium. Bizarre giant cells and numerous mitosis are common occurance. Local recurrence is common following resection and very few patients survived after surgery [13]. In the present case, although the patient had localized tumour at the time of presentation, and no macroscopic residual tumour or enlarged regional lymph nodes at surgery, the patient presented with abdominal mass after receiving 3 cycles of chemotherapy and died soon after.
Authors' Contribution
HKD: Treated the child, arranged data, prepared the manuscript
MB: prepared the manuscript and searched relevant literature.
Conflict of Interests
The authors declare that there are no conflicts of interests.
Ethical Considerations
Written informed consent was obtained from the patient for publication of this case report.
Funding
None
References
[1].DeMaioribus CA, Lally KP, Sim K, Isaacs H, Mahour H(1990) Mesenchymal hamartoma of the liver. Archives of Surgery, 125;598-600 [Pubmed]
[2].Isaacs H., Jr Fetal and neonatal hepatic tumors. J Pediatr Surg. 2007;42:1797–1803. [Pubmed]
[3].Stringer MD, Alizau NK. Mesenchymal hamartoma of the liver: a systematic review. J Pediatric Surg 2005;40:1681–1690. [Pubmed]
[4].Rosenbaum DM, Mindell HJ (1981) Ultrasonographic findings in mesenchymal hamartoma of the liver. Radiology, 138;425-427[Pubmed]
[5].Stanley P, Hall TR, Woolley MM et al (1986) Mesenchymal hamartoma of the liver in childhood:sonographic and CT findings. American Journal of Roentgenology, 147;1035-1039.[Pubmed]
[6].Wootton-Gorges SL, Thomas KB, Harned RK, Wu SR, Stein-Wexler R, Strain JD. Giant cystic abdominal masses in children. Pediatr Radiol. 2005;35:1277–1288
[Pubmed
[7].Dehner LP, Ewing SL, Sumner HW (1975) Infantile mesenchymal hamartoma of the liver. Archives of Pathology.99;379-382.[Pubmed]
[8].Okeda R (1976) Mesenchymal hamartoma of the liver; an autopsy case with serial sections and some comments on its pathogenesis. Acta Pathologica Japonica. 26;229-236[Pubmed]
[9]Stout AP (1948) Mesenchymoma: mixedtumour of mesenchymal derivatives. Annals of Surgery. 127; 278-290.[Pubmed]
[10].Dehner LP (1978) Hepatic tumours in the pediatric age group: a distinctive clinico-pathologic spectrum. Perspectives in Pediatric Pathology. 4; 217-268.[Pubmed]
[11].Ishak KG (1976) Primary hepatic tumours in childhood. Progress in Liver Disease. 5; 636-667 [Pubmed]
[12].Stanely RJ, Dehner LP, Hesker AE (1973) Primary malignant mesenchymal tumours ( mesenchymoma) of the liver in childhood. An angiographic-pathologic study of three cases. Cancer. 32; 973-984.[Pubmed]
[13].Smithson WA, Telander RL, Carney JA (1982) Mesenchymomas of the liver in childhood: 5 years survival after combined modality treatment. Journal of Pediatric Surgery. 17;70-72.[Pubmed]

