Case Report

Isolated Abdominal Aortic Dissection Presenting with Rectal Bleeding
aNicolas Nicolaou,bGideon Van Wyk, cVeronique Nicolaou, d Nigel Flint
- aDivision of Cardiothoracic Surgery, Flora Clinic Johannesburg, South Africa
- bDivision of General Surgery, Flora Clinic Johannesburg, South Africa
- cDivision of Medicine, University of The Witwatersrand Johannesburg, South Africa,
- dDivision of Radiology, Flora Clinic Johannesburg, South Africa
- Submitted: Monday June 9, 2014
- Accepted: November 24, 2014
- Published: December 8, 2014
This is an Open Access article distributed under the terms of the Creative Commons Attribution License ((http://creativecommons.org/licenses/by/3.0)which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited
Abstract
Isolated Abdominal Aortic Dissection (IAAD) may present in a variety of ways resulting in misdiagnosis. It is a rare clinical entity having been reported infrequently in the literature. Presentation of an IAAD with rectal bleeding to our knowledge has not been documented previously and may be directly attributed to occlusion of the internal mesenteric artery by a dissecting aneurysm resulting in ischemic colitis. Description of the mechanism and management is discussed as well as alternative access to the abdominal aorta in cases of “hostile” abdomen
Introduction
Acute aortic dissection is a disease process that generally
affects the thoracic aorta [1]. Aortic dissection begins as
an intimal tear of the aorta resulting in separation of the aortic layers and
extravasation of blood into a false lumen resulting in a catastrophic scenario
with a high mortality in thoracic aortic dissections. The reported incidence of
all thoracic aortic dissections is around 97% whereas Isolated Abdominal Aortic
Dissection (IAAD) have been reported to be less than 2% of all dissections. IAAD
are clinically very different from the degenerative thoracic aortic dissections
and could easily be misdiagnosed for the more common abdominal causes of pain
[2 3].
Case Report
AnAfrican male, aged 32, presented to a peripheral hospital with acute abdominal pain radiating to the back with associated uncontrollable rectal bleeding and subsequent haemoglobin of 5g/100ml. No CT Scan was available at the admitting peripheral hospital and in view of his ongoing bleeding and serious clinical status he underwent emergency exploration laparotomy and resection of an ischaemic descending and sigmoid colon. A second procedure was required to close a colostomy. He was discharged, but returned complaining of ongoing episodes of lower abdominal pain, diarrhoea and limb weakness. Consequently, he was referred to our institution. On admission, he was apyrexial with a pulse rate of 95 beats per minute and a low blood pressure. Abdominal examination revealed numerous surgical scars with tenderness to palpation. The right femoral pulse was weak and the left femoral absent.
No risk factors such as hypertension, smoking or trauma were noted. He was HIV negative and renal function was normal. ACT scan of the abdomen confirmed an IAAD starting below the renal arteries and extending to the aortic bifurcation with occlusion of the inferior mesenteric artery (IMA)(Figure 1). In view of his previous abdominal surgery, a left flank retroperitoneal approach was used to gain access to the aorta. The aorta was easily approached after lifting the abdominal contents anteriorly.
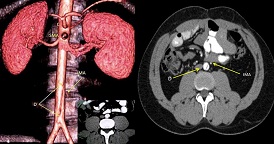
Figure 1: 3D CT of aorta demonstrating a dissection with cut off of the Inferior Messenteric Artery. (C=Coeliac Axis, SMA=Superior Messenteric Artery, IMA=Occluded Inferior Messenteric Artery, D=Aortic Dissection.)
After placing slings around the infra renal aorta and around both common iliac vessels, vascular clamps were applied across thesevessels and the aorta opened confirming a dissection which extended into the orifice of the left iliac artery. A 14mm Haemashield (Boston Scientific) graft was anastomosed to the proximal aorta with 4/0 Prolene and after removing the dissecting flap the graft was anastomosed to the aortic bifurcation
(Figure 2). Anembolectomy with heparin washouts of the peripheral limb vessels was performed prior to closure of the distal anastomosis. He made an uneventful recovery and has been followed up for twenty four months with no further symptoms. Histology of the dissected aorta confirmed cystic medial necrosis.
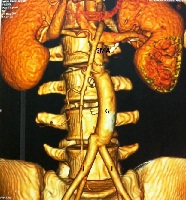
Figure 2: Postoperative 3d CT Scan ShowingAortic Graft(G=Haemashield Graft, SMA=Superior Messenteric Artery, I=Iliac Artery)
Discussion
Isolated dissection of the abdominal aorta is a rare clinical entity described in patients who are usually in their fifth to sixth decades. The most common presenting symptoms are abdominal pain and limb ischaemia. Other reported presentations include neurological deficit (astasia), renal failure and shock due to rupture [3 4 5]. To our knowledge, presentation with rectal bleeding has not been documented and can be directly attributed to occlusion of the (IMA) resulting in ischaemic colitis. The inferior mesenteric supplies the descending colon as well as the rectum which is also supplied by the internal iliac artery and is thus rarely involved in colonic ischaemia.
The clinical presentation in ischaemic colitis varies according to the restriction of blood flow; from mucosal and submucosalhemorrhage, oedema and ulceration progressing to a pathologic picture resembling inflammatory bowel disease and, in severe cases, transmural infarction bleeding and perforation [6]. The site of aortic dissection is usually between the renal and inferior mesenteric arteries and may extend into the iliac arteries. Rarely, a flap may occur at the superior mesenteric level.
Causative factors are not clear but hypertension, blunt abdominal trauma, iatrogenic, spontaneous, aortic disease with calcification and cystic medial necrosis have all been cited as causes[4]. CT angiography is diagnostic and provides accurate definition of branch involvement. Patients that are asymptomatic may be monitored and treated with β blockers although this is the exception rather than the rule [3].
The natural history and long-term outcomes have not been clearly defined, but it is advisable to follow up these asymptomatic patients with yearly CT scans as rupture has been documented to be as high as 14% with an associated high mortality [7].
In view of the rarity and limited experience with IAAD, no scientific studies have been performed to define the appropriate intervention when managing these patients and the limited published data are based on personal experiences and on data gathered from the International Registry of Acute Aortic Dissection. As mortality has been shown to be high in medically treated patients, all symptomatic patients should undergo invasive management by either endovascular stent graft or surgical repair. It has also been suggested that endovascular stenting should be used in high-volume, experienced centres where it has been shown to have a positive impact on outcomes in chronic stable dissections and where significant co-morbidities such as ischaemic heart disease, advanced pulmonary disease, cerebrovascular accidents and or severe renal impairment are present [8]. Surgical results with standard aorto-iliac replacement appear to have superior outcomes especially in the acute forms and can be performed with a low morbidity and mortality [2 3 8]. A left flank retroperitoneal approach has also be shown to be an option especially in a “hostile” abdomen where significant technical difficulties may be encountered and thus can be used in most abdominal aortic repairs as described in this case[9].
Conclusion
ConclusionIAAD, although rare, should be considered in cases presenting with abdominal pain which may also be associated with astasia, back and/or limb pain, decreased femoral pulses as well as rectal bleeding. Surgical or Endovascular intervention is warrantedin this condition [3 10].
Authors’ Contributions
NN: designed and prepared the case report literature review and performed the surgery
GVK: General surgical opinion and manuscript review
VN: Literature review and edited final manuscript
NF: Diagnostic radiologist and manuscript review
Conflicts of Interest
The authors declare that the authors have no conflict to declare
Ethical Considerations
The written informed consent was obtained from publishing this case
Funding
None Declared
References
[1].Rogers AM, Hermann LK, Booher AM, Nienaber CA, Williams DM, Kazerooni EA, Froehlich JB, O'Gara PT, Montgomery DG, Cooper JV, Harris KM, Hutchison S, Evangelista A, Isselbacher EM, Eagle KA; IRAD Investigators. Sensitivity of the aortic dissection detection risk score, a novel guideline-based tool for identification of acute aortic dissection at initial presentation: results from the international registry of acute aortic dissection. Circulation. 2011 May 24; 123(20): 2213-8. doi: 10.1161/CIRCULATIONAHA.110.988568. Epub 2011 May 9.
[Pubmed]
[2].Farber A, Wagner WH, Cossman DV, Cohen
JL, Walsh DB, Fillinger MF, Cronenwett JL, Lauterbach SR, Levin PM. Isolated
dissection of the abdominal aorta: clinical presentation and therapeutic
options. J Vasc Surg. 2002 Aug; 36(2): 205-10.[Pubmed]
[3].Trimarchi S, Tsai T, Eagle KA, Isselbacher EM, Froehlich J, Cooper JV, Rampoldi V, Upchurch GR Jr; International Registry of Acute Aortic Dissection (IRAD) investigators. Acute abdominal aortic dissection: insight from the International Registry of Acute Aortic Dissection (IRAD). J Vasc Surg. 2007 Nov; 46(5): 913-919.[Pubmed]
[4].Mantelas M1, Antonitsis P, Kaitzis D, Hatzibaloglou A, Moros I. Spontaneous isolated dissection of the abdominal aorta: single-center experience. Interact CardiovascThorac Surg. 2009 Apr; 8(4): 398-401. doi: 10.1510/icvts.2008.198051. Epub 2009 Jan 9[Pubmed]
[5].Moses G, Gloviczki P, Park WM, Schultz HL, Andrews JC. Spontaneous dissection of the infrarenal abdominal aorta. SeminVascSurg 2002; 15:128-136
[Pubmed]
[6].Green BT, Tendler DA. Ischemic colitis: a clinical review. South Med J. 2005; 98: 217-222.
[7].Marui A, Mochizuki T, Mitsui N, Koyama T. Acute dissection of the abdominal aorta. J CardiovascSurg 1999; 40: 699-701.[Pubmed]
[8].Eggebrecht H, Nienaber CA, Neuhäuser M, Baumgart D, Kische S, Schmermund A, Herold U, Rehders TC, Jakob HG, Erbel R. Endovascular stent-graft placement in aortic dissection: a meta-analysis. Eur Heart J. 2006 Feb;27(4):489-98. Epub 2005 Oct 14
[Pubmed]
[9].Hepard AD, Tollefson DF, Reddy DJ, Evans JR, Elliott JP Jr, Smith RF, Ernst CB. Left flank retroperitoneal exposure: a technical aid to complex aortic reconstruction. J Vasc Surg. 1991 Sep;14(3):283-91.[Pubmed]
[10].Borioni R1, Garofalo M, De Paulis R, Nardi P, Scaffa R, Chiariello L. Abdominal Aortic dissections: anatomic and clinical features and therapeutic options. Tex Heart Inst J. 2005;32(1):70-3.[Pubmed]

