Case Report

Cervical Chordoma Mimicking a Pottic Abscess
*Khalid Aniba, *Mehdi Laghmari, *Mohamed Lmejjati, *Houceine Ghannane,*Said Ait Benali
- *Department of Neurosurgery, Mohammed the sixth University Hospital, Marrakesh, Morocco.
- Submitted:Thursday, November 21, 2013
- Accepted: Friday, January 24, 2014
- Published: Saturday, March 15, 2014
This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/3.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited
Abstract
Chordomas are rare tumors that arise from the sacrum, spine, and skull base. Surgical management of these tumors can be difficult, given their locally destructive behavior and predilection for growing near delicate and critical structures. Although en bloc resection has proven to be the ideal procedure in other areas, there is controversy regarding this approach in the cervical spine.
En bloc resection can be difficult to perform without damaging adjacent structures and causing significant clinical morbidity. The patient in this case was a 26-year-old woman who presented with quadriparesis. Magnetic resonance imaging demonstrated a large intra and extraspinal vertebral tumor arising from C3-4, a finding that suggested a tuberculous spondylitis. The tumor was completely removed in one stage using the anterior approach, and a corporectomy of C3-4 was also performed. Results from a postoperative histopathological examination confirmed that the tumor was a typical chordoma. The patient’s postoperative course was uneventful.
Keywords
bone tumor • chordoma • cervical spine
Introduction
A chordoma is an uncommon slowly growing locally aggressive tumor, arising from remnants of the notochord. It constitutes between I and 5% of all primary malignant bone tumors [1]. Approximately 50% originate in the sacrum, 35% in the clivus and 15% in the vertebrae proper, with a distribution of 61.1% in the lumbar, 11% in the thoracic and 27.8% in the cervical spine [1]. In half the cases more than one vertebral body is affected. Chordomas occur mostly in the fifth decade and the male to female ratio is approximately 2/ 1 [1].
Chordomas are often difficult to manage, given their locally destructive behavior and predilection to grow near delicate and critical structures. These factors make the
en bloc resection of these tumors with negative margins, currently the gold standard of treatment, difficult to perform without damaging adjacent structures and causing significant clinical morbidity [2].
In this paper, we describe the case of a patient with a large intraspinal and extraspinal chordoma that was completely removed in one operative stage using an anterior approach; we discuss the rationale for our surgical approach, and address the challenge of cervical stabilization after tumor resection.
Case report
Presentation
This 26 year old female patient, previously healthy presented with a 3 year history of constant brachialgia, she also reported occasional numbness in her hands and some unsteadiness of gait due to extremities weakness
Examination
Physical examination revealed a quadriparesis, an altered sensation between C4-C5 bilaterally to pinprick and light touch, as well as extremity spasticity.
Preoperative Planning
Preoperative MR imaging revealed a large mass that expanded into the surrounding soft tissue and spinal canal caused marked spinal cord compression
(Figure 1). On T1 weighted this mass was iso intense (Figure 1a), on T2 image it appeared hyper intense (Figure 1b), on sagittal T2 weighted MRI slice demonstrated that the tumor originated from the C3-4 vertebral body, after administration of gadolinium an inhomogeneous enhancement was observed (Figure 1c) The clinical diagnosis included a neurogenic-based tumor such as an schwannoma, soft-tissue or osseous sarcoma, and a pottic abscess
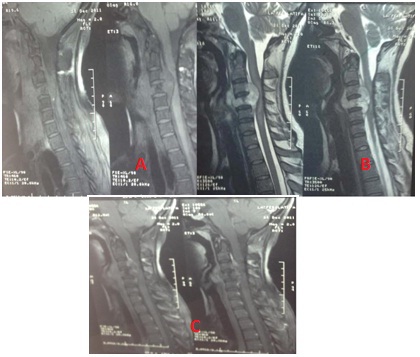
Figure1: preoperative MR images of the cervical spine. A)Sagittal T1-weighted images demonstrating a chordoma involving the C-3 and C-4vertebral bodies with retropharyngeal and epidural extension.B): sagittal T2-weighted image; C) inhomogenous enhancement after contrast.
Operative Technique
She was operated via an anterior approach.The soft-tissue portion of the chordoma was progressively exposed with the typical capsule on its surface. The extraspinal portion of the tumor appeared well encapsulated. A C3-4 corporectomy was achieved by drilling the bone closest to the medial border of the tumor. This resection consisted of removing bone and tumor. Microcurettes and a bipolar cautery were used to carefully dissect the tumor away from the dura mater. After resection had been completed, Hemostasis was obtained using bipolar coagulation and surgicel. To bridge the gap between C2 and C5, an iliac crest graft was used and anterior plate osteosynthesis was carried out, the wound was closed in standard fashion, and the patient was brought to the neurocritical intensive care unit for observation.
Pathological Findings
A postoperative histopathological examination of the tumor showed the typical features of a chordoma, including mesenchymal mucus, physaliphorous cells, and a lobulated structure (Figure 2). No chondroid area was observed on the cut surfaces. Stroma cells stained positively for cytokeratin, epithelial membrane antigen, and vimentin.
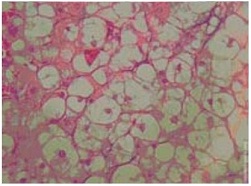
Figure 2: Photomicrograph of operative specimen. The histopathological examination show a typical chordoma features, including mesenchymal mucus, physaliphorous cells with mucus-filled cytoplasm and a lobulated structure. Original magnifications × 400
PostoperativeCourse
The patient was discharged home on postoperative Day 3 without any new neurological deficits or evidence of CSF leak. The patient was seen 7 months postoperatively without evidence of further neurological decline. An MR imaging study performed at that time did not demonstrate evidence of tumor progression or instability. (Figure 3)
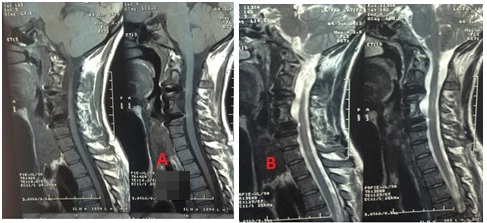
Figure 3: sagittal T1-weighted (A) and T2-weighted (B) MR images obtained 7 months after the operation confirming the complete macroscopic removal of both intra- and extraspinal components of the chordoma without evidence of tumor recurrence or spine instability
Discussions
Chordomas constitute 2 to 4% of all bone neoplasms and 1 to 5% of malignant bone tumors. After plasmacytomas, they are the most frequent primary malignant tumor in the spine [3]. The location of chordomas along the spinal canal is directly related to the location of the notochordal remnants, most frequently at either end of the spinal axis Vertebral chordomas occur in the lumbar, cervical, and thoracic regions, in descending order of frequency. These are slow-growing, low-grade, malignant tumors, which are thought to arise from notochordal remnants [4].
In up to 96%, as in our case, cervical chordomas present by cervical pain with or without brachialgi: pain is caused by bone destruction, nerve compression or by an increased mobility of the vertebral segments.Posterior growth will lead to radicular or even medullary compression with quadriparesis. Anterior growth is reported in 12% leading to loco-regional compression with dysphagia [1].
On standard X-ray it is difficult to detect lesions in their early phase of development. Cervical chordomas may first be manifested as an osteolytic lesion in a vertebral body. In addition to destructive changes, secondary sclerotic changes may present [1]. CT scan is of particular importance to assess bony involvement and soft tissue extension. After intravenous contrast administration, the lesions have been reported to become mottled. CT scan also differentiates between tumoral calcification and bony remnants in lytic areas [1]. MRI is currently the best method to assess the tumoral extension and is particular helpful to identify a local recurrence and islands of tumor in the scar tissue. On T1 images the chordoma may be hypo- or isointense to muscle. On T2 images the lesion returns a high signal. Injection of gadolinium may produce moderate inhomogeneous enhancement of the tumor [1].
by a lobular architecture formed by physaliphorous cells with ample vacuolated cytoplasm and a mucoid intercellular substance. A chordoma cell possesses both antigens with epithelial (cytokeratine), and mesenchymal differentiation (vimentine). Furthermore it can be marked with S100 protein. The dura is commonly invaded. As the correct diagnosis commonly is not evident from the neuroimaging alone, it is necessary to obtain tissue for histological examination [1].
The treatment of chordomas in the cervical spine consists of radical excision and stabilization, followed by adjuvant treatments (radiation and sometimes chemotherapy). Based on well-established principles presented in the Enneking classification [5], the best surgical treatment involves obtaining a wide margin or performing en bloc resection [6 7]. There is no consensus for an accurate oncological definition of en bloc resection [8]. It is generally accepted that it should be a margin-free resection without tumor breach. Boriani recommend en bloc excision of all spinal chordomas when feasible [9].
If a total tumorectomy is not feasible, palliative debulking followed by radiotherapy is worthwhile [1]. Although a chordoma is known to be relatively radioresistant, the value of radiation therapy has been stressed in several reports and series [1]. As most studies cover long periods, during which new techniques were developed, and as the tumor is rather rare, there is no consensus in the literature regarding the optimal radiotherapy scheme for cervical chordomas. Proton-beam and stereotactic radiotherapy are currently being investigated as treatments for these lesions, but there is no clear evidence about the efficacy of these modalities at this time. Currently, chemotherapy does not play a role in the treatment of chordomas, although the use of imatinib mesylate is being investigated [10].
Chordomas have a well-known tendency to recur locally. The recurrence rate seems to be related to the incompleteness of resection [1]. Chordomas of the mobile spine metastasize more often than sacrococcygeal lesions. The reported incidence of metastases varies widely, from 3% to 60%. They are discovered between one and 10 years after the initial diagnosis. The sites of metastases include bone, lungs, lymph nodes, soft tissues, intrathecal space and liver [1]. Only primary and complete resection of the tumor offers a major advantage as far as prognosis is concerned. Clearly the length of follow up in the present study is short, but the extent of tumor resection that could be achieved using these techniques, as well as the limited risk of morbidity encountered and the successful stabilization that was accomplished, has been encouraging.
Conclusions
Chordomas in the cervical spine are rare. Our patient presented with nonspecific symptoms of neck pain with radicular and myelopathic findings. At presentation, the patient had tumor beyond the VB. Intralesional, piecemeal radical tumor resection was performed via anterior approach and successful stabilization was also accomplished. The risk of surgical morbidity was minimal and the patient is able to lead a normal life. It is our opinion that piecemeal removal of the tumor is a viable technique in the management of cervical spine chordomas when the goal is radical tumor removal.
Conflict of Interests
The authors declare there are no conflicts of interests.
Authors’ Contribution
All authors contributed equally in concept, design, literature review and preparation of manuscript.
All authors read the final manuscript and approved it for publication.
Funding
None declared
Ethical Considerations
Written informed consent was obtained from the patient for publication of this manuscript.
References
[1].D’Haen B, De Jaegere T, Goffin J, Dom R, Demaerel P, Plets C Chordoma of the lower cervical spine. Clin Neurol Neurosurg 97:245–248, 1995 [Pubmed]
[2].Hsu W, Kosztowski T.A, Zaidi H.A, Gokaslan. A, Wolinsky JP Image-guided, endoscopic, transcervical resection of cervical Chordoma Technical note J Neurosurg Spine 12:431–435, 2010 [Pubmed]
[3].Barrenechea I.J, Perin N.I, Triana A , Lesser J, Costantino P, Sen C. Surgical management of chordomas of the cervical spine J Neurosurg Spine 6:398–406, 2007 [Pubmed]
[4]Noel G, Feuvret L, Calugaru V, Dhermain F, Mammar H, Haie- Meder C, et al: Chordomas of the base of the skull and upper cervical spine. One hundred patients irradiated by a 3D conformal technique combining photon and proton beams. Acta Oncol 44:700–708, 2005 [Pubmed]
[5].Enneking WF, Spanier SS,Goodman MA: A system for the surgical staging of musculoskeletal sarcoma. Clin Orthop 153: 106–120, 1980 [Pubmed]
[6].Boriani S, Biagini R, De Iure F, Bertoni F, Malaguti MC, Di Fiore M, et al: En bloc resections of bone tumors of the thoracolumbar spine. A preliminary report on 29 patients. Spine 21 :1927–1931, 1996 [Pubned]
[7].Abe E, Kobayashi T, Murai H, Suzuki T, Chiba M, Okuyama K: Total spondylectomy for primary malignant, aggressive benign, and solitary metastatic bone tumors of the thoracolumbar spine. J Spinal Disord 14:237–246, 2001 [Pubmed]
[8].Boriani S, Weinstein JN,Biagini R: Primary bone tumors of the spine. Terminology and surgical staging. Spine 22:1036–1044, 1997 [Pubmed]
[9].Boriani S, Bandiera S, Biagini R, Bacchini P, Boriani L, Cappuccio M, et al Chordoma of the mobile spine: fifty years of experience. Spine 31:493–503, 2006 [Pubmed]
[10].Casali PG, Messina A, Stacchiotti S, Tamborini E, Crippa F, Gronchi A, et al: Imatinib mesylate in chordoma. Cancer 101: 2086–2097, 2004 [Pubmed]

