Case Report

Adjustable Pulmonary Artery Banding: a new strategy now available in Asia
1Ahmad Mahir Shamsuddin1, 2, MD, Mohd Rizal Mohd Zain2,3MMed, Ahmad Mohd Nikman3,1,2Antonio F. Corno
- 1Department of Surgery, Pediatric and Congenital Cardiac Surgery Unit
- 2Department of Pediatrics
- 3Department of Anesthesia School of Medical Sciences
- Health Campus, Universiti Sains Malaysia Kubang Kerian, Kelantan, Malaysia
- Submitted: Friday, May 16, 2014
- Accepted: Sunday, June 01, 2014
- Published: Friday, June 20, 2014
This is an Open Access article distributed under the terms of the Creative Commons Attribution License ((http://creativecommons.org/licenses/by/3.0)which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited
Abstract
The strategy of using the telemetrically adjustable pulmonary artery banding FloWatch-PAB® was introduced in Asia in an infant with multiple ventricular septal defects. A child 3 months old, 4.4 kg, after 2 months of hospitalization because of repeated chest infections due to the presence of multiple ventricular septal defects, atrial septal defect, patent ductus arteriosus and pulmonary hypertension, underwent successful palliative surgery with closure of patent ductus arteriosus and pulmonary artery banding with FloWatch-PAB®. This new strategy available now in Asia can offer a new possibility of treatment of complex congenital heart defects with lower mortality and morbidity.
Keywords
adjustable pulmonary artery banding, congenital heart disease, multiple ventricular septal defects, palliation, pulmonary artery banding
Introduction
The telemetrically adjustable pulmonary artery banding (PAB) FloWatch-PAB® (Leman Medical Technologies, Lausanne, Switzerland) was introduced in Asia for multiple ventricular septal defects (VSDs).
Case Report
A 2 month-old child with multiple VSDs (a large perimembranous and two muscular defects) and patent ductus arteriosus (PDA) (Figure. 1) was admitted at the age of 2 months, weight 4.2kg, after having fever for 2 days, in respiratory distress and heart failure. Chest X-ray (Figure.2) showed cardiomegaly (cardio-thoracic ratio 72%) and evidence of pneumonia. The diagnosis of RSV pneumonia was confirmed, and he remained in hospital with oxygen dependency despite anti-failure treatment (frusemide, spironolactone and enalapril). Single stage repair of the multiple VSDs was judged having too high risk because the clinical conditions of the patient, and therefore a palliative approach with closure of PDA and PAB with the adjustable FloWatch-PAB® was decided.
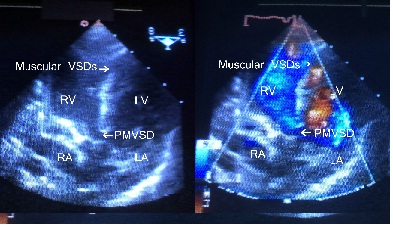
Figure 1 Pre-operative echocardiography showing multiple ventricular septal defects: a large peri-membranous defect and two muscular defects.
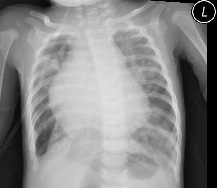
Figure 2. Chest X-ray after admission, showing cardiomegaly and presence of pneumonia.
At 3 months of age, 4.4 kg, the patient underwent surgery. Through median sternotomy the PDA was closed with single metal clip and a FloWatch-PAB® was implanted (Figure. 3) , with increase of the systemic pressure from 57/30 mean 38mmHg to 76/39 mean 51mmHg. During the procedure the percutaneous oxygenation saturation remained around 93% with FiO2=0.5. Echocardiography showed a peak pressure gradient of 27mmHg after tightening the FloWatch-PAB® from 5% to 30%.
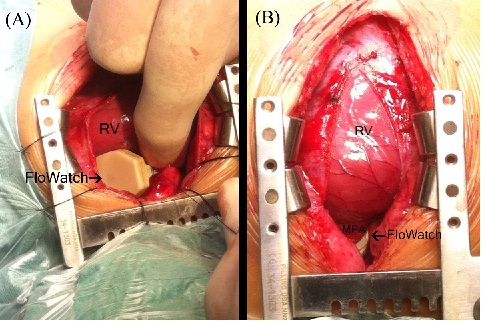
Figure 3. Intra-operative photograph showing the device at the moment of implantation (A) and after the box was moved to the left side before chest closure (B).
The initial post-operative period was complicated by repeated episodes of failed tracheal extubation, without evidence of airways infection, as confirmed but all negative cultures. Eventually after two weeks, the patient was successfully extubated. Progressive adjustments of the FloWatch-PAB® tightening were done throughout the hospitalization, with last one on post-operative day 27th, to reach 65% of tightening. Echocardiography showed a peak pressure gradient across the PAB of 52mmHg with non-invasive systemic blood pressure of 100mmHg and percutaneous oxygen saturation of 97% on room air. The patient was discharged on 29th post-operative day with diuretics and vasodilators. Three months after surgery he is doing well, and the weight increased to 5.6 kg, with percutaneous oxygen saturation of 98% on room air. Last echocardiography showed the complete closure of the two muscular VSDs(Figure.4) with peak pressure gradient across the PAB of 62mmHg. The device tightening has been reduced from 65% to 60%, reducing the pressure gradient to 56mmHg.
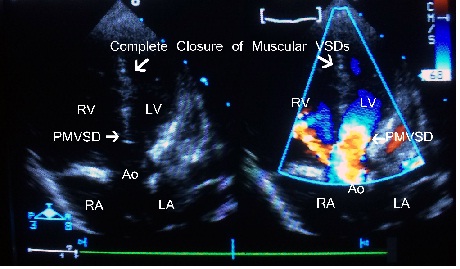
Figure 4. Post-operative echocardiography 3 months after device
implantation, showing complete closure of the two muscular septal defects.
Discussion
FloWatch-PAB® is an implantable, telemetrically controlled device, with the variations in the cross-sectional area achieved by a piston driven by an electric micro-engine. The adjustments are obtained with an external control unit delivering by electro-magnetic coupling the energy and commands to drive the micro-engine.
The device, after long-term experimental studies (1), has been successfully applied for various congenital heart defects in different institutions, with substantial reduction of mortality and morbidity in comparison with the conventional PAB (2,6).
The reasons behind the proven clinical advantages of the FloWatch-PAB® are the progressive tightening of the pulmonary artery over time, with easy adaptation of heart and lungs to the changes in pressures and flows, providing lower early mortality and morbidity, reduced ICU and hospital stay in comparison with the conventional banding (3). In the follow-up repeated both tightening and reopening of the device with the remote control, with the patient awake and not under general anesthesia, for as long as 8 years period were reported (3,5,7). The possibility of successfully releasing the PAB years after implant has never been achieved in any of the adjustable PAB reported in the literature. This is a very important advantages when considering infants with multiple VSDs, where it is possible to release the FloWatch-PAB® endless times when the patient comes for the clinic follow-up with decreasing percutaneous oxygen saturation because of intra-cardiac bidirectional shunt due to the overgrowth. A simple telemetric FloWatch-PAB® adjustment allows to reduce the tightening of the PAB and give to the patient additional time to grow in view of the second stage repair. This allowed to perform the complete repair at the wanted age and body weight, with the patients in good conditions.
In addition, no plasty reconstruction of the main pulmonary artery is required at the moment of device explantation for intra-cardiac repair (4).
In patient with multiple VSDs the “conventional” PAB as well as the one-stage repair were always reported with elevated early and late mortality; substantial morbidity with residual defects, ventricular arrhythmias and biventricular dysfunction was also reported in an elevated percentage of patients after first-stage repair (5). Our new strategy of two-stage approach, with palliation by FloWatch-PAB® followed by later repair, provided good results (5). Spontaneous closure of the muscular VSDs occurred over time, leaving the possibility of closing the remaining VSD at older age and higher body weight, or simply late removal of the device in patients with multiple muscular VSDs (5).
The same strategy was successfully applied in our infant, allowing him to recover from a very precarious clinical condition, and to grow and wait for the complete repair, facilitated by the only need to remove the device and close the peri-membranous VSD in much better condition.
The FloWatch-PAB®, used in several other congenital heart defects as palliation for bi-ventricular and for uni-ventricular hearts (2,5,7) and for left ventricular re-training (3,8), so far has been implanted in 9 European countries (Belgium, Denmak, England, France, Germany, Greece, Italy, Switzerland, Sweeden) and in Saudi Arabia. This is the first implantation in Asia, and the availability of the device in the region can offer a new possibility of treatment of complex congenital heart defects with lower mortality and morbidity.
Conclusion
The advantages of FloWatch-PAB® has been shown markedly reduced the mortality and morbidity of patients required for treatment and its availability in Asia has provides new possibilities of management in complex congenital heart defects.
Funding
This case report has received no specific funding.
Conflicts of Interests Statement
The authors declare that there is no conflict of interests
Authors’ contributions
AMS: carried out the literature search and prepared the draft
manuscript,
MDMZ: carried out the experiments and interpreted the results,
designed the study and performed the analysis
AMN: carried out the
experiments and interpreted the results, designed the study and performed the
analysis
AFC: conceived the study, participated in design and edited the
final manuscript.
All authors read and approved the final manuscript for
submission
Ethical Considerations
The written informed consent was obtained from patient for
publication of this case report.
Acknowledgement
None
References
[1].Corno AF, Sekarski N, Bernath MA, Payot M, Tozzi P, von Segesser LK. Pulmonary artery banding; long-term telemetric adjustment. Eur J Cardiothorac Surg 2003;23:317-22[Pubmed]
[2].Corno AF, Bonnet D, Sekarski N, Sidi
D, Vouhé P, von Segesser LK. Remote control of pulmonary blood flow: initial
clinical experience. J Thorac Cardiovasc Surg 2003;133:461-4[Pubmed]
[3].Corno AF, Ladusans EJ, Pozzi M, Kerr S. FloWatch® versus conventional pulmonary artery banding. J Thorac Cardiovasc Surg 2007;134:1413-9[Pubmed]
[4].Corno AF, Prosi M, Fridez P, Zunino P, Quarteroni A, Von Segesser LK. The non-circular shape of FloWatch®-PAB prevents the need for pulmonary artery reconstruction after banding. Computational fluid dynamics and clinical correlations. Eur J Cardiothorac Surg 2006;29:93-9
[5].Corno AF, Kandakure PR, Dhannapuneni RRV, Gladman G, Venugopal P and Alphonso N. Multiple ventricular septal defects: a new strategy. Frontiers in Pediatric Cardiology 2013;1-16:1-6[Pubmed]
[6].Kalavrouziotis G, Karanasios E, Konstandopoulou G, Paphitis C. Telemetrically adjustable pulmonary artery banding: first application in Greece. Hellenic J Cardiol 2008;49:195-8[Pubmed]
[7].Dhannapuneni RRV, Gladman G, Kerr S, Venugopal P, Alphonso N, Corno AF. Complete atrioventricular septal defect: outcome of pulmonary artery banding improved by adjustable device. J Thorac Cardiovasc Surg 2011;141:179-82[Pubmed]
[8].Sekarski N, Hurni M, von Segesser LK, Meijboom EJ, Di Bernardo S. Adaptable pulmonary artery band for late arterial switch procedure in transposition of the great arteries. Ann Thorac Surg 2012;94:1311-6

