Case Report

Giant Cutaneous Horn Arising from a Burn Scar: A Case Report and Literature Review
1Richard J. Zinn
- 1Division of Plastic and Reconstructive Surgery, Department of Surgery, University of the Witwatersrand, Johannesburg. 14 Via Calabria, Stirling street, Waverley, Johannesburg, South Africa.
- Submitted: Saturday, May 17, 2014
- Accepted: Sunday, June 01, 2014
- Published: Friday, June 20, 2014
This is an Open Access article distributed under the terms of the Creative Commons Attribution License ((http://creativecommons.org/licenses/by/3.0)which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited
Abstract
Cutaneous horn (cornu cutaneum) is a descriptive term for a conical, dense surface projection of adherent keratin that resembles an animal’s horn. The underlying process may be benign, premalignant or malignant.
Historically, cutaneous horns have evoked interest and superstition, at times, resulting in the bearer being socially isolated or outcast. Classically, cutaneous horns occur in sun-damaged skin of elderly (greater than 5th decade), fair-skinned patients, often on the face, ears, penis, extremities and occasionally the trunk.
We present an unusual case of a relatively young (44 year old) black male, who developed an impressive cutaneous horn from a burn scar – a site, rarely described to yield such a lesion.
Key words
Giant cutaneous horn; burn scar carcinoma; cutaneous horn; marjolin’s ulcer
Introduction
Despite numerous but sporadic reports in the literature since circa 1300 A.D., giant cutaneous horns have remained a medical curiosity. Historically, cutaneous horns have evoked significant interest and superstition, at times, resulting in the bearer being socially isolated or outcast. A cutaneous horn (cornu cutaneum) is a descriptive term for a conical, dense surface projection of adherent keratin that resembles an animal’s horn, but lacks an internal bone. The underlying process may be benign, pre-malignant or malignant with incidence of 61.1%, 23.2% and 15.7% respectively. [1, 2, 3]
Case Report
We describe an unusual case of a 44 year old male from an isolated rural area who developed an impressive cutaneous horn from a burn scar. He had sustained deep burn to the right chest and axilla 36 years previously, which was managed conservatively. He presented with a 5-month history of a painful, rapidly growing lesion, reminiscent of a ram’s horn, arising centrally from the burn scar. An 80 x 30 x 15mm cutaneous horn arising from an area of hypopigmented scar tissue was noted
(Figure 1, 2, 3). The cutaneous margins were regular, smooth, mobile and minimaly erythematous. A tight grade IV axillary contracture, with less than 10 degrees of abduction was associated.

Figure 1: 44-year old male with a well developed cutaneous
horn arising from an axillary burn contracture, sustained 36 years previously.

Figure 2: Cutaneous horn arising from right axillary grade 4
burn contracture.

Figure 3: Close up image of a well-developed cutaneous horn
80x30x15mm in dimensions
The horn and surrounding tissue were resected with a 10mm margin
(Figure 4). Histopathological examination confirmed the presence of an underlying moderately well differentiated, keratinizing squamous carcinoma which had been completely resected with uninvolved margins. At a second stage and axillary contracture release and a split thickness graft were performed. Post operative healing was uneventful and abduction to 100 degrees was obtained.
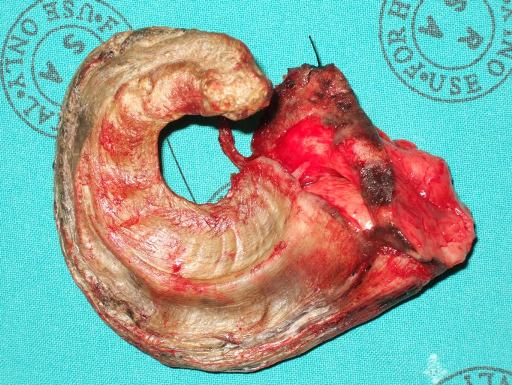
Figure 4: Excision was undertaken with a 10mm margin.
Histological section of the base of the horn demonstrated a moderately well
differentiated, keratinizing squamous carcinoma. It was completely resected with
uninvolved margins.
Discussion
Cutaneous horns arise from the epithelial layer, but it is the underlying cause that is of clinical significance. [4] Classically, the tumour occurs in sun-damaged skin of fair skinned elderly patients, often on the face, ears, extremities and occasionally the trunk.In the largest pathological series, reported by Yu et al., an underlying malignant or pre-malignant lesion was identified in 38.9% of cases.[3] Such malignancies are usually well differentiated squamous carcinomas, although basal cell carcinoma and metastatic renal cell carinoma have also been reported.[2] Premalignant causes include actinic keratosis and bowen’s disease. Benign lesions that may result in a cutaneous horn include seborrheic keratosis, histiocytoma, inverted follicular keratosis, molluscum contagiosum and verruca vulgaris. [5]
Small cutaneous horns are not uncommon, but “giant” horns, such as in this case, are unusual. Surgical opinion is frequently sought early and resection performed. The paucity of reports concerning “giant” cutaneous horns has led to a lack of formal criteria to label a cutaneous horn as “giant”.After a review of the literature, we suggest the following criteria for classification of a cutaneous horn as a “giant”:
The base should be greater than 20 mmThe Height : Base ratio should be greater than 3 : 1
The horn should consist of true keratin, rather than fibrinous crust
The management of such lesions is surgical and is directed at the underlying lesion. As illustrated by this case and supported by the literature, we recommend primary excision of such lesions in conjunction with Moh’s micrographic surgery, or frozen section in cosmetically and functionally sensitive areas. Without these modalities, margins of 4mm should be considered safe if the base is less than 20mm in diameter, and 6 mm margins for lesions with a base greater than 20mm in diameter
[8]
Conclusion
The cutaneous horn stimulates both medical interest and social implications for the patient. Its early diagnosis and management can remedy both social stigmatisation and un underlying premalignant or malignant condition. Size at presentation my be related to delay in presentation and should be taken into account when determining resection margins at extirpation.
Funding
None
Conflicts of Interests Statement
The authors declare that there are no conflicts of interests.
Authors’ contributions
RJZ – concept design, preparation of manuscript and editing.
Ethical Considerations
Written informed consent was obtained from the patient for
publication of this case report.
Acknowledgement
None.
References
[1].Bondeson J, Everard Home, John Hunter and cutaneous horns, A Historical Review. Am J of Dermatopathol 2001; 23(4): 362 - 369 [Pubmed]
[2].Copcu E, Sivrioglu N, Culhaci N, Cutaneous horns, are these lesions as innocent as they appear to be? World J Surg Oncol. 2004; 2:18[Pubmed]
[3].Yu R, Pryce D, Macfarlane A, Stewart T, A histopathological study of 643 cutaneous horns. Br J of Dermatol. 1991; 124: 449 – 52[Pubmed]
[4].Mencia-Gutierrez E, Gutierrez-Dias E, Redondo-Marcos I, et al. Cutaneous horns of the eyelid: a clinocopathological study of 48 patients. J Cutan Pathol 2004; 31: 539 – 543 [Pubmed]
[5].Leppard W, Loungani R, Saylors B, et al. Mythology to reality: Case report of a giant cutaneous horn of the scalp in an African American female. J Plast Reconstr Aesthet Surg. 2014; 67: 22-24[Pubmed]
[6].Copcu E. Aktas A. Sisman N. et al. 31 Cases of Marjolin’s ulcer. Clin Exp Dermatol 2003; 28: 138 – 141[Pubmed]
[7].Turegen M. Nisanci M. Guler M. Burn scar carcinoma with a longer lag period, arising in previously grafted area. Burns 1997; 23: 496 – 497[Pubmed]
[8].Motley R, Kersey P, Lawrence C. Multiprofessional guidelines for the management of the patient with primary cutaneous squamous cell carcinoma. Br J Plast Surg. 2003; 56: 85-91[[Pubmed]

