Case Report

Intrahepatic Pancreatic Pseudocysts Complicating Chronic Calcific Pancreatitis - A Rare Differential for Multiple Cystic Liver Lesions.
* Ramakrishna Narra, *Susheelkumar Kamaraju, *Naganarasimharaju Juluri,
- *Department of Radiodiagnosis, KaturiMedical College, Guntur,Andhra Pradesh, India
- Submitted Saturday, November 22, 2014
- Accepted:Monday, January 05, 2015
- Published Thursday, January 08, 2015
This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/3.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited
Abstract
Pseudocyst is a common complication of acute and chronic pancreatitis. Though relatively common complication of pancreatitis an intra hepatic location is rare. More over multiple pseudocysts of liver are even rare to occur. We present a case report of pseudocysts in a 24 year old female patient with chronic calcific pancreatitis communicating with pancreatic duct and extending into left lobe of liver.
Key-words
Pseudocyst, pancreas, left lobe of liver, falciform ligamentum , ligamentum teres
Introduction
Pseudocyst of pancreas is a common complication of both acute and chronic pancreatitis. The prevalence of pancreatic pseudocysts in acute pancreatitis has been reported from 6% to 18.5% and in chronic pancreatitis 20% to 40% [1]. Common sites of occurrence are body, tail, head of pancreas, lesser sac, perisplenic area, retroperitoneum, mediastinum and pararenal areas [2]. Occurrence of pseudocyst in left lobe of liver is rare. To date only 30 cases are reported. We present a case report of young female presented for an ultrasound to our department with abdominal pain and vomiting. An ultrasound guided aspiration of cystic fluid in liver showed raised amylase levels in the aspirate.
Case Report
A 24 Year old female patient with complaints of abdominal pain in epigastric region and vomiting since one week was referred to our department for an ultrasound examination. Her blood examination was unremarkable except for raised amylase and lipase levels. Ultra sound examination revealed atrophied pancreatic parenchyma, dilated main pancreatic duct with calculi and calcifications of parenchyma, pseudocysts with suspicious communication with main pancreatic duct in body, and extending into left lobe of liver as multiple cystic lesions (Figure 1). Cystic fluid also appears to track along falciform ligament. On contrast enhanced CT, atrophied pancreatic parenchyma with calcifications, dilated duct with calculi (Figure 2) and multiple pseudocysts with enhancing rim and with communication with main pancreatic duct in body noted extending into left lobe of liver. Cystic fluid appeared to track along falciform ligament and ligamentum teres (Figure 3,4,5).
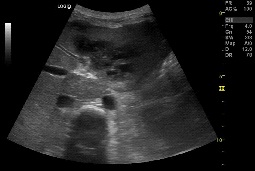
Figure1. Axial ultrasound image showing pseudocyst extending into left lobe of liver. Few calcifications noted in pancreatic parenchyma.
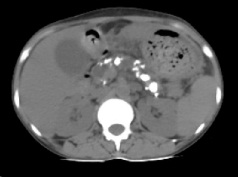
Figure2: Plain axial CT SCAN image showing calcifications in the pancreatic parenchyma and dilated duct

Figure3: Sagittal reformatted CECT image showing a pseudocyst extending from pancreas into left lobe of liver, with communication to pancreatic duct. Multiple pseudocysts of variable sizes seen in liver.
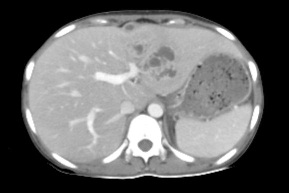
Figure 4: CECT axial image showing multiple cystic lesions in left lobe of liver. Collection noted along ligamentum teres.
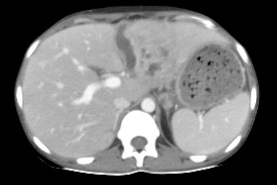
Figure 5: Axial CECT image showing extension of cyst along falciform ligament on to the surface of liver. Multiple small cystic lesions can also be seen in left lobe of liver.
Discussion
Pancreatic pseudocyst is defined as collection of pancreatic fluid & inflammatory exudate encapsulated by fibrous tissue [2]. It is a known complication of both acute and chronic pancreatitis. The prevalence of pancreatic pseudocysts in acute pancreatitis has been reported to range from 6% to 18.5% and in chronic pancreatitis from 20% to 40% [1]. Pseudocysts develops over a period of 4-6 weeks after onset of acute pancreatitis. Location in two thirds is within pancreas (body & tail (85%); head (15%)). One third of pseudocysts occur in lesser sac juxtasplenic region, retroperitoneum & mediastinum, pararenal areas liver and other distant locations [2]. Lesions in left lobe of liver are rare and only about 30 cases are reported in literature to date [3].
Intra hepatic pseudocysts are usually single, most commonly involve left lobe of liver. Because the pathophysiology of pseudocyst formation is by enzymatic destruction, pathology will not be confined to surrounding anatomical spaces in retroperitoneum [4]. Pathophysiological mechanisms involving left lobe of liver are either extension of pseudocyst in lesser sac through lesser omentum or gastrohepatic ligament towards the liver forming subcapsular collections or tracking through hepatoduodenal ligament from head to the porta hepatis resulting in intra parenchymal collections [3 4].
Ultrasonographic findings of a pseudocyst include usually solitary unilocular cyst (multilocular - 6% of cases), fluid-debris level & internal echoes due to autolysis (blood clot/cellular debris), septations (raresign of infection or hemorrhage). Dilated pancreatic duct & CBD, calcification of pancreas are seen in chronic pancreatitis. Usual CT findings in pseudocysts are round or oval, homogeneous, hypodense lesion with a near water density ("mature" pseudocyst). Hemorrhagic, infected pseudocyst appears as lobulated, heterogeneous, mixed density lesion with or without pancreatic calcification. Main pancreatic duct (MPD) & common bile duct (CBD) dilatation can also be noted. On contrast, enhancement of thin rim of fibrous capsule is seen, and contents do not enhance. Gas within pseudocyst suggests superimposed infection. Decompression of pseudocyst into pancreatic duct, stomach or bowel may result in gas within cyst. Pseudoaneurysms can be caused by or simulate a pseudocyst [2].
Our case demonstrated cysts with enhancing rim from body of pancreas into left lobe of liver tracking along falciform ligament and ligamentum teres. Communication of pseudocyst with pancreatic duct noted. Left lobe of liver showed multiple small cystic lesions showing communication with pancreatic duct establishing the diagnosis of left lobe extension of pancreatic pseudocyst.
Differentials include abscess, intrahepatic hydatid cyst, mucinous cystic tumor of pancreas, intraductal papillary mucinous tumor [2]. There is no history of fever and the cystic lesion appears to track from body of pancreas into left lobe of liver through falciform ligament which makes abscess and hydatid unlikely. Confirmation was made by raised amylase levels in aspirate fluid done under ultrasound guidance.
There are no definite guidelines on the management of intra-hepatic pseudocysts. Surgical drainage, radiologically guided percutaneous drainage/aspiration, transpapillary stent or transpapillary nasopancreatic drainage have been successfully used in the treatment of intrahepatic pseudocysts of pancreas [3].
Key Message
Pseudocyst of pancreas is a common complication of acute and chronic pancreatitis; its extension into liver can occur but is rare and must be considered as a differential in these patients
Authors Contribution
RN: carried out the literature search and prepared the draft manuscript, carried out the experiments and interpreted the results, designed the study and performed the analysis, conceived the study, participated in design and edited the final manuscript.
SK: carried out the literature search and prepared the draft manuscript
NJ: carried out the literature search and prepared the draft manuscript, carried out the experiments and interpreted the results, designed the study and performed the analysis, conceived the study, participated in design and edited the final manuscript.
Conflict of Interests
The authors declare that there are no competing interests
Ethical Considerations
Written informed consent was obtained from the patient for publication of this case report.
Funding
None declared
References
[1].Khanna AK, Tiwari SK, Kumar P. Pancreatic Pseudocyst: Therapeutic Dilemma. International Journal of Inflammation 2012; Article ID 279476, 7 pages. http://dx.doi.org/10.1155/2012/279476
[Pubmed]
[2].Federle MP, Anne VS. Pancreatic Pseudocyst. In:Federle. Diagnostic Imaging, 1st ed. Utah:Amirsys ; 2004. P II–3: 24 – 27.
[3].Bhasin DK, Singh SR, Singh VC, Mohit N,Nikhil N, Saroj KS, Nagi Bet al. An Intra-hepatic pancreatic pseudocystsuccessfully treated by endoscopic transpapillarydrainage alone. J Pancreas (Online) 2005; 6(6):593-597.PMID: 16286711
[Pubmed]
[4].Scappaticci F, Markowitz SK.Intrahepatic pseudocyst complicating acute pancreatitis: imaging findings.AJR Am J Roentgenol. 1995 Oct; 165(4):873-4.PMID: 7676984
[Pubmed]
\

