Case Report

Persistent Left Sided Svc Found Incidentally on Central Line Insertion
*Peter Andrawes,*Bishoy Hanna,*KrassimirAtanassov.
- *Department of Surgery, Staten Island University Hospital, 475 Sea View Avenue, Staten Island, NY, United States of America.
- Submitted Sunday, June 21, 2015
- Accepted:Saturday, July 25, 2015
- PublishedMonday, August 03, 2015
This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/3.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited
Abstract
Persistent Left Sided Superior Vena Cava (PLSVC) is a rare vascular anomaly however; it is the most common venous anomaly of the thoracic venous system. It is present in 0.3 to 0.5% of the population [1, 2]. PLSVC is the result of persistence of the embryonic left anterior cardinal vein and is usually considered a normal variant. In this case report, we present a case of persistent left sided SVC in a 64 year old man associated with anterior cerebral artery aneurysm.
Keywords
Persistent Left Superior Vena Cava, Persistent LSVC, Anterior Cerebral Artery Aneurysm, Thoracic Vascular Anomalies.
Introduction
Persistent LSVC was found incidentally during insertion of left sided internal jugular central line. Persistent LSVC is a rare vascular anomaly however; it is the most common venous anomaly of the thoracic venous system. It is present in 0.3 to 0.5 % of the population [1, 2]. Persistent LSVC is associated with congenital anomalies of the heart, great vessels, and cerebral vasculature [3].
We report a case of persistent left sided SVC associated with anterior cerebral artery aneurysm. To our knowledge, this is the first case that describes this association.
Case report
64-year-old man presented to our hospital complaining of headache and left sided weakness. His past medical history was significant for hypertension. Patient’s symptoms started12 hours before coming to the ED and worsened over time. Patient denied any history of fall or recent head trauma.
Patient had a CT scan of the head, which showed a large subarachnoid hemorrhage. Subsequent CTA showed 1.3 x 0.8 x 0.9 centimeters saccular lobulated aneurysm arising from a pericallosal branch of the anterior cerebral artery. The neck of the aneurysm was approximately 3mm in diameter. Patient went for transcatheter angiography of right and left internal carotid arteries and coil embolization of pericallosal aneurysm.
After surgery, patient remained intubated and was admitted to ICU. The patient had a right-sided internal jugular central line placed on post-operative day 1 for access and hemodynamic monitoring. On post-operative day 14, patient had several febrile episodes and leucocytosis. To rule out line infection, the right side central line had to be removed. Therefore, another central line was inserted on the contralateral internal jugular vein. A follow-up chest x-ray was done for verification of line placement [Figure 1a,, 1b,] . The catheter was noted to be in the left chest and not crossing the midline. This raised the question of whether the catheter was placed into the venous or the arterial system.

Figure 1: Chest roentgenogram A): Chest X-ray showing right and left Internal Jugular central lines with the left side central line in the left chest without crossing the midline.
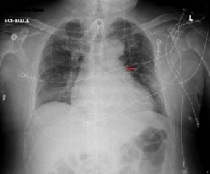
1. B) Chest X-ray showing the left side central line after removal of the right sided catheter (Red arrow).
Blood gas measurements, taken from the line showed(pH: 7.35, PO2: 37, PCO2: 42, HCO3: 24) a gas equivalent to venous blood. We then connected the catheter to a transducer however; no arterial waveforms were noted. CT Chest from a previous admission [Figure 2a,,2b,]was reviewed and showed an atretic left brachiocephalic vein with persistent left superior vena cava draining into the right atrium. The right-sided SVC was draining into the right atrium normally. Additionally, the patient was also found to have a tracheal bronchus supplying portions of the right upper lobe. This is also considered a rare anomaly of the bronchial tree.
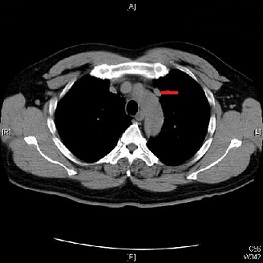
Figure 2: Computed Tomography A) CT Chest showing persistent Left SVC (Red arrow)
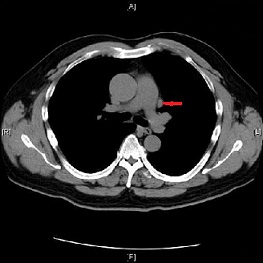
2.B) CT Chest showing Persistent LSVC at a lower level in the chest (Red arrow).
Discussion
Persistent LSVC is a rare vascular anomaly however, it is the most common venous anomaly of the thoracic venous system. The persistent left superior vena cava has been described as the most frequent variation in the central venous return and thorax venous system. Persistent left superior vena cava may occur alone i.e. without a contralateral SVC or in combination with a right-sided SVC. Having bilateral SVCs occurs in 4.08% of the population (range 0.2–8%) [4]. Having a left SVC in the absence of a right superior vena cava is very rare with an estimated frequency of approximately 0.1% [4]. Usually the persistent LSVC drains via the coronary sinus into the right atrium but in rare cases it may draininto the left atrium creating a small right-to-left shunt. PLSVC is the result of persistence of the embryonic left anterior cardinal vein and is usually considered a normal variant. One superior vena cava will be present on each side of the mediastinum with or without a rudimentary left innominate vein as a communication between the two.
Persistent LSVC is associated with other congenital cardiovascular abnormalities like atrial septal defects, endocardial cushion defects, tetralogy of Fallot, aortic coarctation, ventricular septal defects and transposition of great arteries[3]. This case describes an association between LSVC and cerebral vascular abnormalities namely the anterior cerebral artery aneurysm, which has been rarely described in the literature. Another interesting observation in this patient was the presence of the tracheal bronchus supplying portions of the right upper lobe. Tracheal bronchus is another normal variant of the tracheobronchial tree with prevalence of 0.1-3%[5].
Diagnosis of left SVC is usually made incidentally during placement of central venous catheter, pacemaker, implantable cardioverter defibrillator or during thoracic surgery. In this case the diagnosis was made after insertion of central line catheter. After obtaining a chest x-ray, abnormal course of the catheter was noted to go downwards instead of crossing the midline.
Conclusions
Persistent LSVC is a rare vascular anomaly however; it is the most common venous anomaly of the thoracic venous system. Although it may be associated with cardiovascular anomalies, in this case it was associated with cerebrovascular aneurysm. Awareness of this anomaly may avoid the patient unnecessary interventions and investigations in the future. Clinicians should also be aware of this variant when evaluating central venous line placement.
Authors’ Contributions
PA: Corresponding author: contribution to this study included Study design, collection of data, literature search, analysis of the data, writing and editing the final manuscript and supervision.
BH: contribution to this study included collection of data, literature search and writing the final manuscript.
KA: contribution to this study included Study design, literature search and supervision.
Conflict of Interests
The authors declare that there are no conflicts of interests
Ethical Consideration
The written informed consent was taken from the patient for publication of this case report.
Funding
None declared
References
[1] Coblentz MG, Criscito MA, Cohn JD: Persistent left superior vena cava complicating hemodynamic monitoring catheterization.Crit Care Med 1978, 6:32-35 [PubMed]
[2] Danielpour PJ, Aalberg JK, El-Ramey M, Sivina M, Wodnicki H: Persistent left superior vena cava: an incidental finding during central venous catheterization-a case report.Vasc Endovascular Surg2005, 39:109-111 [PubMed]
[3] Goyal SK, Punnam SR, Verma G, Ruberg FL: Persistent left superior vena cava: a case report and review of literature.Cardiovascular ultrasound 2008, 6:1-4.[PubMed]
[4] Tobias JD, Russo P: Anesthetic care during modified fontan procedure without cardiopulmonary bypass.J CardiothoracVascAnesth2005, 19:612-619.[PubMed]
[5] Bakir B, Terzibasioglu E: Images in clinical medicine. Tracheal bronchus.N Engl J Med 2007, 357:1744.[PubMed]

