Case Report

Cecal Perforation Secondary to Appendicitis-But not at the Base of Appendix
* Ravi Shankar J C, *Narayan Hebsur, * Hosmani Ramesh, * K N Praveen, * Kumar Abhishek,
- *Department of General Surgery, Karnataka Institute of Medical Sciences, Hubli, Karnataka, India-580022
- Submitted: Sunday, September 6, 2015
- Accepted: Tuesday, December 29, 2015
- Published: Sunday, February 7, 2016
Abstract
Introduction
Acute appendicitis is the most common surgical emergency. It is associated with a variety of complications among which cecal perforation is a rare and technically difficult condition. Usually cecum perforates at the base of the appendix.
Case presentation
A 19 year old female came with complaints of fever and vomiting since 5 days; and pain abdomen since 1 day. On examination, she was toxic and had features of peritonitis. Radiological investigations confirmed the presence of peritonitis. On exploration, appendix was found inflamed and perforation was found at the posterior wall of cecum. Primary omental patch repair was performed. Histopathology report confirmed that the perforation was due to periappendicitis.
Conclusion
Cecal perforation, itself is a diagnostic and therapeutic challenge to all surgeons and is associated with a high mortality. Here we sensitise the medical fraternity to such a challenging case and the therapeutic options.
Keywords
appendicitis, cecal perforation, acute abdomen, right hemicolectomy
Introduction
We surgeons generally consider appendicitis as a case to be done by the junior-most person in the unit. But as there is a saying, “no surgery is minor”, we all should give utmost care to a case of appendicitis as well. Because the complications associated with appendicitis are challenging, we need to have a high index of suspicion to diagnose such conditions. This report is an unusual complication of appendicitis, wherein there was a cecal perforation, not at the base of appendix, but due to periappendiceal inflammation in the posterior cecal wall.
Appendicitis needs to be considered in the differential diagnosis of nearly every patient with acute abdominal pain. It can be easily diagnosed by history and clinical examination, supplemented by blood investigations and imaging studies. The mortality rate for acute appendicitis with treatment is reported to be <1%. The overall rate of perforated appendicitis is 19.2%. Children <5 years of age and patients >65 years of age have the highest rates of perforation. It has been suggested that delays in presentation are responsible for the majority of perforated appendices. Worldwide, perforated appendicitis is the leading surgical cause of death. Appendiceal rupture occurs most frequently distal to the point of luminal obstruction along the antimesenteric border of the appendix. It can also rupture near base of appendix to involve cecal wall. Perforation of cecum may be impossible to distinguish from appendicitis and is associated with a high mortality rate[1, 2].
Case presentation
A 19 year old young girl presented to casualty with history of fever and vomiting since 5 days and pain abdomen since 1 day. Her past history, family history and menstrual history were insignificant. On examination, she was febrile, tachycardic, tachypneic and hypotensive. Abdominal examination revealed a tense abdomen, with tenderness maximal in right iliac fossa, with diffuse guarding, rigidity and rebound tenderness. On auscultation, bowel sounds were sluggish. Digital rectal examination showed formed stools.
Total leucocyte count was 14,000 cells/cumm; Erect x-ray abdomen showed air under diaphragm; Ultrasonogram showed moderate free fluid in peritoneal cavity with dense internal echoes, edematous bowel loops, air pockets in peritoneal cavity, septic peritonitis features. A probable diagnosis of appendicular perforation was made.
Patient was immediately taken for exploratory laparotomy. Intra-op, appendix was found inflamed but the perforation was neither found at the tip of appendix nor at the base. Perforation was found 2cm away from the base of appendix in the posterior wall of cecum measuring about 6x3 mm. The intervening cecal wall found inflamed (Figure 1).

Figure 1: Intra-op picture of perforation of cecum with appendicitis.
There was no evidence of distal obstruction. Primary closure of perforation with omental patch repair was done with absorbable suture along with appendicectomy. There was no evidence of any other intra-abdominal pathology like colonic growth or distal obstruction. Patient was allowed to take orally once the bowel sounds returned and was discharged on 7th post-op day. Histopathology report revealed features of acute appendicitis with periappendicitis. Cecal perforation specimen showed necrotic areas with edematous submucosa and muscular layer and inflammatory infiltrate comprising predominantly of lymphocytes (Figure 2). There were no evidence of malignant cells or feature suggestive of tuberculosis in representative cecal biopsy.
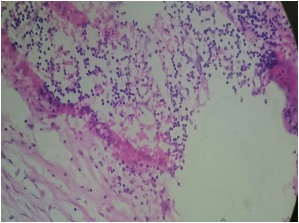
Figure 2: Histopathology picture showing periappendicitis with perforation
Discussion
Appendicitis perforations, commonly occur at the tip of the appendix, are associated with the presence of a faecolith on CT scan and not the anatomical location of the appendix (retrocaecal appendix) as previously thought [3]. Cecal perforation is a diagnostic challenge, as it is an unusual, less well-known [4].
There are a variety of causes for cecal perforation like trauma, distal obstruction, inflammatory, tumors. Trauma in the form of penetrating and non-penetrating injury, surgery or foreign body is the most common cause for cecal perforation [5]. Few case of non-traumatic [6] and spontaneous [7]cecal perforations have been described in literature. But cecal perforation secondary to appendicitis occurring in the posterior wall of cecum is not described. This is probably the first such case to be described in literature.
Primary repair, cecostomy, and ileocecal resection with ileostomy are among the therapy options for cecal perforation[6]. In the presence of an uncomplicated perforation, absence of severe infection, and well controlled localized haemostasis - a less invasive surgical approach with post-operative intravenous antibiotics would be the management of choice [8]. Diversion ileostomy was the other treatment option in this case. Because there was minimal contamination and a small perforation, we went ahead with primary omental patch repair. Right hemicolectomy carries a higher morbidity and mortality and is generally recommended in cases of severe inflammation, torsion, haemorrhage, and inflammatory mass, necrotic cecum or if cecal neoplasm is found intraoperatively. A larger prospective study is needed to compare different surgical approaches and long termoutcome [8]. The representative biopsy from the cecal wall showed features of periappendicitis. In this case there was no other cause for cecum to perforate apart from periappendicitis initiated by appendicitis which is an usual presentation.
Conclusion
Cecal perforation is one of the dreaded complication of appendicitis. Perforations in cecum can occur not only in the base of appendix, but in its posterior wall as well. A high index of suspicion is required to thoroughly search for perforation, or else it is likely to be missed. Primary omental patch repair, diversion ileostomy and right hemicolectomy are the treatment options. Here we report a rare complication of a common ‘acute abdomen’ condition and the probable aetiologies and treatment modalities for the same.
Learning points
-
Appendicitis, though considered minor surgery, can be associated with serious complications
-
Posterior cecal wall perforations can occur not only in tuberculosis, Crohn’s and malignancy, but also in appendicitis as well.Right hemicolectomy is not always required for cecal perforation. Primary omental patch closure also has good results in selected cases.
Ethical Consideration
Written informed consent was obtained from the patient for publication of this Case Report and any accompanying images. The consent is available with authors.
Competing interests
The authors declare that there are no competing interests.
Authors’ Contribution
RS carried out the literature search and prepared the manuscript,
NH and RH edited the manuscript, PKN and
AK participated in literature search and edited the manuscript. All authors read and approved the final manuscript for submission.
References
[1].Zinner MJ, Ashley SW. Maingot’s abdominal operations, Twelfth edition, McGraw Hill medical, 2013. Chapter 31,” Appendix, Meckel’s and other small bowel diverticula”, Page 623-647.
[2].Townsend CM, Beauchamp RD, Evers BM, Mattox KL. Sabiston textbook of surgery, 19th edition, Elsevier Saunders publication, Philadelphia 2013. Chapter 51, “The Appendix”, Page 1279-1293.
[3].Herscu G, Kong A, Russell D, Tran CL, Varela JE, Cohen A, Stamos MJ. Retrocecal appendix location and perforation at presentation. Am Surg 2006; 72(10):890-3. [PubMed]
[4].Dirican A, Unal B, Bassulu N, Tatli F, Aydin C, Kayaalp C. Isolated cecal necrosis mimicking acute appendicitis:A case series. J Med Case Rep. 2009;3:7443. doi: 10.4076/1752-1947-3-7443 [PubMed].
[5].Albers JH, Smith LL, Carter R. Perforation of the cecum. Ann Surg 1956; 143, 251-255. [PubMed]
[6].Cetinkaya Z, Girgin M, Ozercan IH, Ayten R. Non-traumatic cecal perforation on a female patient:Report of a case. Fusabil 2006; 20: 445-46 [Full
text].
[7].Yeo R. Spontaneous perforation of the caecum case series and a review of the literature. Postgrad. Med. J. 1967; 43:65-67. [PubMed]
[8].Wong CS, Naqvi SA. Appendicular perforation at the base of the caecum, a rare operative challenge in acute appendicitis, a literature review. World J Emerg Surg. 2011;6:36. doi: 10.1186/1749-7922-6-36 [PubMed].

