Case Report

Idiopathic Orbital Inflammation with rare Parotid Extension
Okoturo Eyituoyo1, Ogunbanjo Olabode2, Oestreicher James3, Popoola Abiodun4, Faduile Adedayo5, Banjo Adekunbiola6
- 1Department of oral and Maxillofacial Surgery, Faculty of Dentistry, Lagos State University College of Medicine, Lagos, Nigeria
- 2Unit of Oral & Maxillofacial Surgery, Department of Dental Surgery, Lagos State University Teaching Hospital (LASUTH), Lagos, Nigeria
- 3Department of Ophthalmology, University of Toronto, Toronto, Canada
- 4Oncology Unit, Department of Radiology, Lagos State University Teaching Hospital, Lagos, Nigeria 5Department of Pathology and Forensic Medicine, Lagos State University Teaching Hospital (LASUTH), Lagos, Nigeria
- 5Department of Pathology and Forensic Medicine, Lagos State University Teaching Hospital (LASUTH), Lagos, Nigeria
- 6Department of Morbid Anatomy, Lagos State University Teaching Hospital (LASUTH), Lagos, Nigeria
- Submitted: February 1, 2012
- Accepted February 10, 2012
- Published: February 13, 2012
This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Objective:
Idiopathic orbital inflammation (IOI) is a benign inflammatory process usually confined to the orbit, with preponderance for extraorbital extension (EOE). We describe a case of IOI with possible extension to the parotid gland, a presentation yet to be reported in the literature
Case report:
A 38-year-old man was referred from a psychiatric unit with a 9 year history of swelling of the right parotid region, with periorbital swelling and proptosis of the right eye. Eleven years earlier, the orbital swelling was treated with steroid and surgery. At our center, the parotid swelling was treated with steroid therapy and adjunct chemo-radiotherapy. Patient was eventually lost to follow up.
Discussion:
Diagnosis of IOI is based on clinical, imaging and histological examination. EOE of IOI, though rare has been reported with 41 cases reported to date. But an EOE to the parotid gland is yet to be reported. The significance of which is the possible addition of parotid gland scanning to all other previously known extraorbital sites, during an EOE survey; being part of IOI management.
Introduction
Idiopathic orbital inflammation (IOI) is a benign inflammatory process usually confined to the orbit, with preponderance for extraorbital involvement [1,2]. Originally described as Busse & Hochheim in 1903 was labelled as a psuedotumor by Birch-Hirschfield in 1905 [2].
Jackson in 1958, probably described the earliest report of an extraorbital extension of IOI [2]. In this report, we describe a case of IOI with possible extraorbital extension (EOE) to the parotid gland. This is probably the first reported case in English Literature.
Case Report
A 38-year-old man was referred to the Oral/Maxillofacial Surgery (OMFS) Clinic, Lagos State University Teaching Hospital (LASUTH), Lagos, Nigeria, from a psychiatric centre. He presented with a 9 year history of right parotid swelling with associated right orbital proptosis

Figure 1: showing clinical appearance at Presentation at OMFS clinic, LASUTH
and periorbital swelling (Figure 1). History taking revealed a 26 year history of peri-orbital swelling, proptosis and poor vision of the right eye (Figure 2). An 11 year old CT Scan report obtained from the Ontario Cancer Institute, University of Toronto Teaching Hospitals (OCI-UTTH), detailed a right upper and lower eyelid mass measuring 4.0 x 2.5 cm and 2.9cm in dimension and diameter respectively.
At OCI-UTTH, the orbital swelling was managed with multiple courses of prednisolone therapy, 30mg per day and gradually tapered to 5mg per day over 2 months. A year after the prednisolone therapy, a right anterior orbitotomy plus tumour debulking surgery and adjunct radiotherapy of the right orbit was carried out at the Ophthalmic Unit of UT
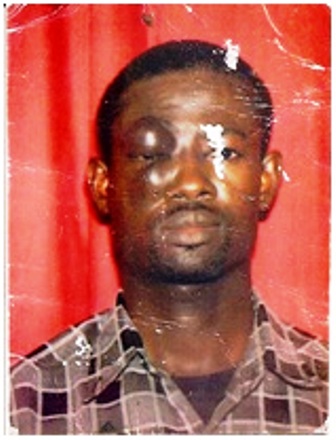
Figure 2: Presentation at OCI-UTTH 10 Years ago
TH. The histopathology report obtained at the UTTH, detailed extensive replacement of orbital soft tissue with dense collagen. The collagen contained many blood vessels with small collections of inflammatory cells (lymphocytes), scattered macrophages, multinucleated giant cells, plasma cells and eosinophils. The inflammatory reaction involved skeletal muscles. A diagnosis of Sclerosing Inflammatory Pseudotumour (SIP) was made. Molecular analysis by Polymerase Chain Reaction (PCR) indicated no evidence of B- or T- cell monoclonality or involvement of BCL-2 genes. These were consistent with the diagnosis of an inflammatory pseudotumour. Following this course of treatment, the swelling reduced significantly and vision of the right eye became normal.
Presently, patient had a history of psychosis that was being managed at the referral psychiatric centre. Examination at the presentation revealed a massive swelling of the right parotid region measuring 14cm by 11cm at its widest diameters (Fig 1). It was painless and soft to firm in consistency. There was associated mild periorbital swelling of the right eye which was proptosed, but vision was normal. No facial nerve branch palsy. All blood parameters appeared normal. A working diagnosis of pleomorphic adenoma of the right parotid gland was made, to exclude recurrent parotitis.
An axial CT scan of the head at 5mm slice thickness and 5mm interval after administration of IV contrast medium detailed a well circumscribed, markedly enlarged superficial lobe of the right parotid gland, measuring 45mm x 38mm with mixed density pattern. There was also fusiform enlargement of the inferior rectus muscle of the right orbit measuring 30mm x 16mm x (24mm) with displacement of the eye globe anterior inferiorly. Other extraoccular muscles and the optic nerve appeared normal. There was no evidence of bony erosion.
Fine needle aspiration cytology reported an inconclusive hemorrhagic smear. The histopathology report following a biopsy, detailed
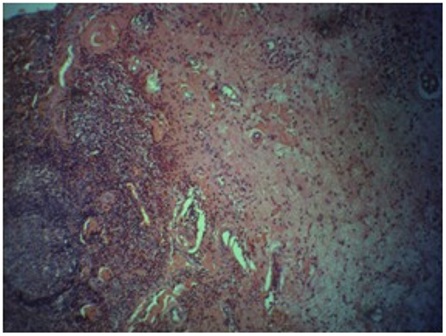
Figure 3: Photomicrograph from light microscope showing myxoid background with infiltrates of macrophages and plasma cells. H & E x 100
a picture of infiltrates of focal granulomatous lesion in a myxoid background. The granulomatous lesion comprised central areas with foam macrophages and some plasma cells surrounded peripherally by polymorphonuclear leucocytes and lymphocytes (Figure 3). The features were consistent with idiopathic orbital inflammation. The ophthalmologist review reported essentially normal vision of the right eye.
Patient was commenced on oral prednisolone 80mg/day in three divided doses, which resulted in significant reduction in parotid swelling after 2weeks, as seen in (Figure 4). Steroid dosage was reduced by 20mg every two weeks until therapy was concluded. By the 4th week, swelling had reduced significantly, adjudged using circumferential measurements at its widest diameter. The parotid swelling continually remained reduced until the 6th week at dosage of 20mg daily when a recurrence was observed. It was eventually noticed that any dosage below 30mg resulted in a recurrence of the parotid swelling. Post steroid side effects included insomnia and constipation which improved over the duration of the steroid therapy.
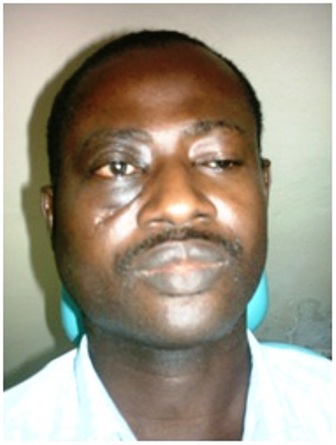
Figure 4: Clinical photograph 2weeks post steroid therapy
Based on a previous history of radiosensitivity of the IOI, patient was referred to the oncologist for adjunct radiotherapy. The oncologist decided to administer chemotherapy: intravenous cyclophosphamide 1000mg and methotrexate 100mg. Ondansetrone 8mg was also administered by slow intravenous injection. The patient received 6 courses at 3weeks interval. Parotid swelling reduced significantly. Patient was not keeping his review appointment and was lost to follow up, only to present at the oncology clinic 9 months post chemotherapy with a recurrence of the parotid swelling. Radiotherapy was then commenced at 60 greys in 30 fractions. Swelling reduced post radiotherapy. Patient was reviewed one month post radiotherapy and no evidence of recurrence was observed. Patient was eventually lost to follow up after this period. Thus, it was difficult to verify if treatment was successful.
Discussion
Idiopathic orbital inflammation (IOI) is a benign, non-specific, space occupying inflammatory process characterised by soft tissue infiltration by inflammatory cells with varying degree of fibrosis depending on its chronicity [2]. There are three main histopathological subtypes: lymphocytic, granulomatous and sclerosing type [3]. IOI may involve extraocular muscles, fat, sclera, the optic nerve or lacrimal gland [4]. Symptoms are primarily proptosis, diplopia, decreased ocular movement, decreased vision and pain [5,6]. The term orbital pseudotumour was originally introduced to include all non-neoplastic disorders, but now the term is limited to those lesions that are idiopathic in nature. However, the term idiopathic orbital inflammation is more appropriate [6].
The cause is unknown but the likelihood of autoimmunity with viral, genetic and environmental triggers, have been reported [7,8,9]. Diagnosis is based on clinical and imaging evidence of orbital inflammatory disease in the absence of any known localised or systemic cause, combined with histological evidence of marked fibrosis and chronic inflammatory infilterates [1,5]. IOI rapid response to corticosteroids maybe a useful diagnostic indicator, but with reports of orbital cellulites, thyroid and malignant eye diseases all responding similarly, while crucial, may not be solely dependable [10,11]. The differential diagnoses will include: infections, lipogranuloma, histiocytosis, fibromatosis, Wegener’s granulomatosis and lymphoma [4].
Extraorbital extension (EOE) of IOI though not very common has been previously reported. To the best of our knowledge, and if our case is inclusive, there would be 42 cases of IOI with EOE reported in the literature as illustrated in Table 1. Sites would include: intracranial(21), paranasal sinus(10), infratemporal fossa(2), pterygopalatine fossa(4),greater wing sphenoid (1), optic canal (1) cheek (1)infra orbital fissure (1),parotid (1) [1,3,4,5,12,13].
The differentials for this EOE to the parotid would include: chronic sialadenitis of the parotid and an inflammatory pseudotumour of the parotid gland [14]. Chronic sialadenitis of the parotid gland is a common recurrent clinical condition, characterised by painful swelling, pus discharge and associated inflammatory changes to the parotid gland [15,16]. Treatment is by antibiotic therapy or/and parotidectomy [15].
Inflammatory pseudotumour of the parotid gland is a rare benign lymphoproliferative disorder with characteristic histologic picture of granular cytoplasm interspersed with inflammatory cells of plasma cells and lymphocytes [14,17]. It is characterised by a fairly constant sized swelling and often no accompanying symptoms [14]. There is no consensus on the mode of treatment, but surgery is carried out for a number of cases [14]. Other modes of treatment will include: radiotherapy, chemotherapy, azathioprine, antibiotics and steroids with steroids in particular, rapidly reducing the swelling [14,17].
So, it is plausible to suggest that the parotid swelling in our report is an inflammatory pseudotumour of the parotid gland. The question then arises, is it an EOE or a solitary pseudotumour?
While reports in the literature adequately documented inflammatory process initiated within the orbit extending to adjacent sites, the clinical findings of some cases of EOE, does not allow any definite conclusion on the initial site of the inflammatory process to be made [12,19,20]. Some authors have advocated that when more extensive IOI is seen compared to the EOE, its origin is probably orbital [4,21].
Some have suggested the following clinical observations for IOI with an EOE: That both histological pictures are similar, that EOE is usually more aggressive than the IOI and the sclerosing subtype of the IOI has a higher propensity to extend outside the orbit than other subtypes [2,12,22].
Our case presentation of IOI involving the right upper and lower eyelids appears to depict both swellings having an overall larger mass volume than the supposed EOE according to the CT Scan reports. Also, the IOI was of the sclerosing variant. All features appear to suggest an IOI with preponderance for EOE. However, the EOE showed no evidence of bony destruction or aggression, which is at variant with an IOI EOE.
The methods for treatment of IOI remain controversial. The use of corticosteroids, immunosuppressive agents like azathioprine, cyclophosphamide and cyclosporine, radiotherapy and surgical debulking have all been advocated, but there have been no randomised or controlled trial studies [2,4,5,7,11].
The initial treatment of IOI in this case was with a multitude of corticosteroid regime. The tumour was steroid resistant and eventually surgical debulking was done. This proved to be effective. The EOE was also initially treated with high dose corticosteroids. Tumour was or became steroid resistant, thus immunosuppressive agents and then radiotherapy was used. Unfortunately patient was lost to follow up and the success or failure of the treatment regime could not be objectively assessed.
It was observed that steroid therapy below 30mg in daily divided doses resulted in a recurrence of the parotid swelling. The reason and significance of this was not known. We suspect the loss of the patient to follow-up may not be unconnected with the patient’s psychotic episodes. Reports have been made of the link between prolonged steroid therapy and psychosis [22]. In the review of the 27 clinical, surgical and referral notes of the patient made over ten years ago, obtained from the Ophthalmic unit and OIC-UTTH, no mention was made of any psychotic episodes. However, we were unable to implicate the long term steroid therapy to the psychosis.
The significance of this parotid EOE to a clinician is vital in that a patient may present with an IOI EOE to the parotid mass that may be considered an unrelated finding as was initially thought in this case. Hence, in the management of IOI, the parotid gland should be considered a possible EOE site and thus should be scanned during EOE survey in the management of IOI [4].
This study had a limitation. The final outcome of the patient being unclear due to the loss of patient to follow-up. However, our objective was to present, the orbito-parotid similarity and possible spread and not to significantly add to the controversy on management of IOI. The treatment result of this chronic lesion being mostly a controlled outcome.
Conclusion
We report a case of IOI with a recurrent parotid swelling with common histopathology. This orbito-parotid relationship and possible parotid EOE is to draw attention to the broadening clinicopathological spectrum of IOI, than was initially thought.
Acknowledgement
The authors wish to acknowledge the efforts of the nurses in all the units involved in this report during the course of patient management
Source of Funding:
None
Competing interest:
The authors declare that there are no competing interests.
Authors’ contribution
OE: Managed the patient, conceived the study, carried out the literature search, designed the study, analysed and interpreted the result, drafted and edited the manuscript
OO: Contributed in managing the patient, contributed in designing, analyzing and interpreting the study and edited the manuscript
OJ: Managed the patient, contributed in analyzing and interpreting the result and edited the Manuscript
PA: Contributed in management of the patient and edited the Manuscript
FA/BA: Reported the histology slide, contributed in managing the patient and edited the Manuscript
All authors have read and endorsed the manuscript.
Ethical Consideration
This observational study was a case of a patient with a prior history of right ocular swelling, who presented at our center with a swelling on the right parotid region. This case was managed with the knowledge of the ethical committee of the Lagos State University Teaching Hospital who adjudicated the need for ethical clearance.
References
[1]. Mahr MA, Salomao DR, Garrity JA. Inflammatory orbital pseudotumour with extension beyond the orbit. Am J Ophthamol 2004;138:396-400
[2]. Zborowska B, Ghabrial R, Selva D, McCluskey P. Idiopathic orbital inflammation with extraorbital extension: case series and review. Eye 2006;20:107-113
[3]. Clifton A, Borgstein R, Moseley I, Kendall B, Shaw P. Intracranial extension of orbital pseudotumour. Clin Radiol 1992;45:23-26
[4]. de Jesus O, Inersni JA, Gonzalez A, Colon LE. Idiopathic orbital inflammation with intracranial extension: case report. J Neurosurg 1996;85:510-513
[5]. Hsuan JD, Selva D, McNab AA, Sullivan TJ, Saeed P, O'Donnell BA. Idiopathic sclerosing orbital inflammation. Arch Ophthalmol 2006;124:1244-50
[6]. Kaye AH, Hahn JF, Craciun A, Hanson M, Berlin AJ, Tubbs RR. Intracranial extension of inflammatory pseudotumour of the orbit. Case report. J Neurosurg 1984;60:625-629
[7]. Swamy BN, McCluskey P, Nemet A, Crouch R, Martin P, Benger R, Ghabriel R, Wakefield D. idiopathic orbital inflammation syndrome: Clinical features and treatment outcomes. Br J Ophthalmol 2007;91:1667-1670
[8]. Jacobs D, Galetta S. Diagnosis and management of orbital pseudotumour. Curr Opin Ophthalmol 2002;13:347-51
[9]. Yuen SJA, Rubin PAD. Idiopathic orbital inflammation: ocular mechanisms and clinicopathology. Ophthalmol Clin North Am 2002;15:121-126
[10]. Mombaerts I, Goldschmeding R, Schlingemann RO, Koornneef L. What is orbital pseudotumour? Surv Ophthalmol 1996;41:66-78
[11]. Jacobs D, Galetta S. Diagnosis and management of orbital pseudotumour. Curr Opin Ophthalmol 2002;13:347-351
[12]. Cruz AA, Akaishi PM, Chahud F, Elias JJ. Sclerosing inflammation of the orbit and in the pterygopalatine and infratemporal fossae. Ophthal Plast Reconstr Surg 2003;19:201-206
[13]. Eshaghian J, Anderson RL. Sinus involvement in inflammatory orbital pseudotumour. Arch Ophthalmol 1981;99:627-630
[14]. Barrios-Sanchez GM, Dean-Ferrer D, Allamillos-Granados FJ, Ruiz-Masera JJ, Zafra-Camacho FM, Garcia de Marcos JA, Calderon-Bohorquez JM. Inflammatory pseudoyumor of the parotid gland. Med Oral Patol Oral Cir Bucal 2005;10:371-375
[15]. Wang S, Marchal F, Zou Z, Zhou J, Qi S. Classification and management of chronic sialadenitis of the parotid gland. J Oral Rehab 2009;36:2-8
[16]. Motamed M, Laughine D, Bradley PJ. Management of chronic parotitis: a review. J Laryngol Otol 2003;117:521-526
[17]. Mielcarek MW, Bates C, Uppal S, Nadig S, Coatesworth AP. Benign inflammatory pseudotumour of the parotid gland: A case report and literature review. Int J Clin Pract 2004;58:527-529
[18]. Kaye AH, Hahn JH, Craciun A, Hanson M, Berlin AJ, Tubbs RR. Intracranial extension of inflammatory pseudotumour of the orbit. J Neurosurg 1984;60:625-629
[19]. Borruat FX, Vuilleumier P, Ducrey N, Fankhauser H, Janzer RC, Regli F. Idiopathic orbital inflammation (orbital inflammatory pseudotumour): an unusual cause of transient ischaemic attack. J Neurol Neurosurg Psychiatry 1995;58:88-90
[20]. Frohman LP, Kupersmith MJ, Lang J, Reede D, Bergeron RT, Aleksic S, Trasi S. intracranial extension and bone destruction in orbital pseudotumour, Arch Ophthalmol 1986;104:380-384
[21]. Som PM, Brandwein MS, Maldjain C, Reino AJ, Lawson W. inflammatory pseudotumour of the maxillary sinus: CT and MRI findings in six cases. AJR Am J Roentgenol 1994;163:689-692
[22]. Pagonis TA, Koukoulis GN, Hadjichristodoulou CS. Psychiatric side effects induced by supraphysiological doses of combinations of anabolic steroids correlate to the severity of the abuse. Eur Psychiatric 2006;21:551-562

