Original Article

Isolated Intra Fourth Ventricular Neurocysticercosis
*Divye Prakash Tiwari, *Vivek Sharma, *Deepak Patil, *Amrita Ghosh
- *Department of Neurosurgery and Pathology, Institute of Medical Sciences, Varanasi, India
- Submitted: December 05, 2013
- Accepted: December 09, 2013
- Published: December 15, 2013
This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/3.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Introduction
Neurocysticercosis is one of the most frequently observed central nervous system parasitic infection caused by the larvae of the pork tapeworm, Taenia solium. The fourth ventricle is the most frequent location of intraventricular neurocysticercosis that carries a higher risk for CSF blockage and resulting in hydrocephalus.
Methods
We report a series of cases of 13 patients with symptomatic obstructive hydrocephalus due to cysticercus in the fourth ventricle presenting to us over a period of 7 years.
Conclusion:
The excision of fourth ventricular cysts typically requires a microsurgical approach via suboccipital craniotomy.
Key words
neurocysticercosis, fourth ventricle, hydrocephalus, Neurosurgical procedure.
Introduction
Neurocysticercosis (NCC) is a parasitic disease caused by infection with the larval form of Taenia solium or pork tapeworm and is the most frequent parasitic infestation of the central nervous system.[1,2] Neurocysticercosis is acquired when T. solium eggs are consumed, either via fecal–oral contact with a tapeworm carrier or ingestion of food or water contaminated by T. solium eggs. Persons harboring adult tapeworms in their intestines may also acquire neurocysticercosis via fecal–oral autoinfection. After ingestion, the tapeworm egg hatches and penetrates the intestine, and travels through the bloodstream to develop into cysticerci in the central nervous system, muscles, or eyes. Although the medical management of neurocysticercosis with cysticidal drugs is controversial, neurosurgical resection of fourth ventricular neurocysticercosis cysts is the treatment of choice. In this series we focus on the management of neurocysticercosis presenting in the fourth ventricle with resultant hydrocephalus.
Patients and Methods
All cases of fourth ventricular neurocysticercosis reported to neurosurgery in last 7 years were taken into study. They were analysed in respect to age, sex, symtoms, radiology and management. Their incidence, a etiology and treatment protocol were discussed.
Observation
We have encountered 13 cases of fourth ventricular neurocystercercosis presenting with acute hydrocephalus. The maximum incidence (6 cases) were found in the age group 21-30 years, while 2 cases were found in 0-10 years group, 3 cases were in 11-20 years group, whereas 2 cases were in 31-40 years group.[Table 1]
Table 1:Incidence of intrafourth ventricular neurocysticercosis.
|
Age(years) |
Sex |
Incidence |
| 0-10 |
Male |
1 |
| Female |
1 |
| 11-20 |
Male |
1 |
| Female |
2 |
| 21-30 |
Male |
2 |
| Female |
4 |
| 31-40 |
Male |
1 |
| Female |
1 |
Eleven patients presented with headache, nine patients with vomiting, and unconsciousness, decreased visual acuity in five patient, and blindness in one patient. [Table 2]
Table 2:Clinical findings
|
Clinical features |
No. of patients |
|
Headache |
11 |
|
Vomiting |
09 |
|
Unconsciousness |
01 |
|
Blurred vision |
05 |
|
Blindness |
01 |
Management
MRI is the investigation of choice depicting the well defined cyst with or without small enhancing dot with CSF all around. [Fig.1,2,3] There may be associated hydrocephalus depending upon the degree of block.

Figure 1: Coronal section of T1 weighted MRI showing cyst in fourth
ventricle

Figure 2: Axial section of MRI T1 weighted showing well defined cyst in 4th
ventricle

Figure 3: Sagittal section of brain
The treatment of fourth ventricular NCC is defined by the clinical presentation. The first thing to define is the presence or risk of acute hydrocephalus thereby the option of ventriculostomy or ventriculoperitoneal shunt. [Table 3] Intraoperative ultrasonography may help in localising the cyst. [Fig.4] Histopathology confirmation was done in all cases. [Fig.5]
Table 3 Surgical options
|
Procedure |
No. of patients |
|
Ventriculoperitoneal shunt followed by posterior
fossa decompressive craniotomy and cyst removal |
4 |
|
Direct posterior fossa decompressive craniotomy
and cyst removal |
9 |

Figure 4: Intraoperative ultrasound of brain
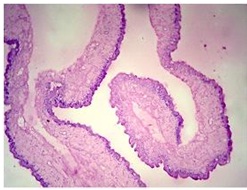
Figure 5 : Histopathological examination of cyst wall
Discussion
Isolated fourth ventricular neurocystercercosis can cause acute hydrocephalus by mass effect resulting in CSF outflow obstruction. Isolated fourth ventricular neurocysticercosis presents with headaches in 77% to 100% of patients, whereas parenchymal neurocysticercosis have seizure as presenting feature in 70% of patients. Isolated intra fourth ventricular neurocysticercosis presents as throbbing headache and blurred vision, syncopal event, bradycardia as it is in close proximity to the floor of the fourth ventricle. [3-16].
The diagnosis of neurocysticercosis is made by classic imaging finding of a cystic lesion containing a ‘‘nodule’’, which represents the ‘‘scolex’’ of the T. solium larva.
MRI is the preferred in a patient with possible neurocysticercosis, as it is more sensitive and specific than CT scan. The fourth ventricular neurocysticercosis is often isodense or isointense with CSF, posing difficulty in diagnosis. Occasionally, the scolex can be seen as a hyperintense dot within the cyst being diagnostic of cysticercal cyst. [19] The cornerstone of most neurocysticercosis management is symptomatic therapy. This includes the use of anti-epileptic drugs for seizure control, treatment of hydrocephalus, and the use of corticosteroids to attenuate the host immune response, especially when giving cysticidal therapy (albendazole, praziquantel) or attempting cyst resection. Indication for neurosurgical resection of neurocysticercosis cyst is generally limited to intraventricular cyst, giant subarachnoid cyst (usually located within the Sylvian fissure), and cyst causing spinal cord compression.
In a series of 45 patients with intraventricular cysticercosis, the fourth ventricle was the most common location for cyst (53%) followed by the third ventricle (27%), lateral ventricles (11%) and Sylvian aqueduct (9%). [20] Hydrocephalus associated with intraventricular cyst usually does not require shunt surgery after excision of the cyst. Shunt has also been known to be the cause of migration of fourth ventricular cyst into the third or lateral ventricles due to a siphon effect. Excision of fourth ventricular cyst typically requires microsurgical approach via suboccipital craniotomy. [17, 18]
The available treatment options are: medical, external cerebro-spinal fluid diversion, microsurgical, or endoscopic removal alone or in combination. Albendazole (15 mg/kg/day for 3-4 weeks) is recommended for IVNCC even after surgical procedures. [21] Praziquantel (100 mg/kg/day for 3-4 weeks) may cause rapid regression of large cyst of the fourth ventricle thus avoiding the need for surgery.[22,23] Direct surgical excision through sub- occipital approach is better option than shunt as shunt associated complication rate is high. [24] Shunt surgery only may be contemplated if pericystic enhancement without mass effect are seen in MRI. [25] Endoscopic neurosurgery is a minimally invasive technique enabling removal of intraventricular cyticercal cyst from all locations, thus avoiding major craniotomy/posterior fossa exploration and shunt. [26]
Conclusion
The intra fourth ventricular cysticercosis is relatively uncommon and prersent with raised intracranial pressure due to hydrocephalus. The investigation of choice is MRI. Surgical option is better than medical but there are few reports where lesion disappeared on antihelmenthic treatment. The excision of fourth ventricular cyst typically requires microsurgical approach via suboccipital craniotomy.
Conflict of Interest
The authors declare that they have no conflict interests.
Authors' Contribution
VS: Concept of study and final approval
DPT: Concept and analysis of study, literature search and preparation of manuscript
DP: Concept and design of study
AG: Histopathological examination
Ethical Considerations
Not declared
Funding
None declared
References
[1]. Obrador S. Cysticercosis cerebri. Acta Neurochir 1962;10:320-364. [Pubmed].
[2]. Cuetter AC, Garcia-Bobadilla J, Guerra LG, Martinez FM, Kaim B. Neurocysticercosis: focus on intraventricular disease. Clin Infect Dis 1997;24:157-164. [Pubmed].
[3]. Patharangkura P, Jariya P, Tandhavadhana. Cysticercus racemosus in the fourth ventricle: report of two cases. Southeast Asian J Trop Med Public Health. 1980;11(4):532- 534. [Pubmed].
[4]. Palmer J, Poulgrain P. Cysticercosis of the fourth ventricle: a report of two cases. Aus N Z J Surg. 1980 Feb;50(1):60-63. [Pubmed].
[5]. Elliott EM, Fried RA. Cerebral cysticercosis of the fourth ventricle: a problem in primary care diagnosis. J Fam Pract. 1984;19(4):553-557.[Pubmed].
[6]. Gupta RK, Jain VK, Kumar S, Gupta S, Haque I, Gujral RB. Unusual MRI appearances of cysticercus within the fourth ventricle. Neuroradiology. 1993;35(6):457-458. [Pubmed].
[7]. Flisser A, Madrazo I. Evagination of Taenia solium in the fourth ventricle. N Engl J Med. 1996;335(10):753-754. [Pubmed].
[8]. Govindappa SS, Narayanan JP, Krishnamoorthy VM, Shastry CH, Balasubramaniam A, Krishna SS. Improved detection of intraventricular cysticercal cysts with the use of three-dimensional constructive interference in steady state MR sequences. AJNR Am J Neuroradiol. 2000;21(4):679-684. [Pubmed].
[9]. Savindra TL et al. Neurocysticercosis in Asia. The Internet Journal of Infectious Diseases 2002:1(2):21-23.
[10]. Singh S, Gibikote SV, Shyamkumar NK. Isolated fourth ventricular cysticercus cyst:MR imaging in 4 cases with short literature review. Neurol India. 2003;51(3):394-396. [Pubmed].
[11]. Hortobágyi T, Alhakim A, Biedrzycki O, Djurovic V, Rawal J, Al-Sarraj S. Cysticercosis of the fourth ventricle causing sudden death: a case report and review of the literature. Pathol Oncol Res. 2009;15(1):143-146.[Pubmed].
[12]. Prashantha DK, Netravathi M, Ravishankar S, Panda S, Pal PK. Reversible parkinsonism following ventriculoperitoneal shunt in a patient with obstructive hydrocephalus secondary to intraventricular neurocysticercosis. Clin Neurol Neurosurg. 2008;110(7):718-721.
[13]. Das A, Kesavadas C, Radhakrishnan VV, Nair NS. Teaching NeuroImages: Bruns syndrome caused by intraventricular neurocysticercosis. Neurology. 2009 Aug 18;73(7):34. [Pubmed].
[14]. Roongpiboonsopit D, Shuangshoti S, Phanthumchinda K, Bhidayasiri R. Positional vomiting as the initial manifestation of Bruns syndrome due to cysticercosis in the fourth ventricle: a symptom reminiscent of an old disease. Eur Neurol. 2012;67(3):184-185. [Pubmed].
[15]. Hanak BW, Walcott BP, Codd PJ, Jones PS, Nahed BV, Butler WE, Asaad WF. Fourth ventricular neurocystercercosis presenting with acute hydrocephalus. J Clin Neurosci. 2011;18(6):867-869. [Pubmed].
[16]. Singh S, Gibikote SV, Shyamkumar NK. Isolated fourth ventricular cysticercus cyst: MR imaging in 4 cases with short literature review. Neurol India. 2003;51(3):394-396. [Pubmed].
[17]. Madrazo I, Proaño J. Tratamiento quirúrgico de la neurocisticercosis. En: Arriagada C, Nogales-Gaete J, Apta W, eds. Neurocisticercosis. Santiago: ARRYNOG 1997; 299-321.
[18]. García HH, Gonzalez AE, Evans CA, Gilman RH; Cysticercosis Working Group in Peru. Taenia solium cysticercosis. Lancet. 2003; 362: 547-556. [Pubmed].
[19]. García HH, Del Brutto OH. Imaging findings in neurocysticercosis. Acta Trop 2003;87:71–8 [Pubmed].
[20]. Apuzzo ML, Dobkin WR, Zee CS, et al.Surgical considerations in treatment of intraventricular cysticercosis. An analysis of 45 cases. J Neurosurg 1984;60: 400–7. [Pubmed].
[21]. Husain M, Rastogi M, Jha DK, Husain N, Gupta RK.Endoscopic transaqueductal removal of fourth ventricular neurocysticercosis with an angiographic catheter. Neurosurgery. 2007;60(Suppl 2):249-253.[Pubmed].
[22]. Anandh B, Mohanty A, Sampath S, Praharaj SS, Kolluri S. Endoscopic approach to intraventricular cysticercal lesions. Minim Invasive Neurosurg. 2001;44(4):194-196. [Pubmed].
[23]. Proaño JV, Madrazo I, García L, García-Torres E, Correa D.Albendazole and praziquantel treatment in neurocysticercosis of the fourth ventricle. J Neurosurg. 1997;87(1):29-33.[Pubmed].
[24]. Allcut DA, Coulthard A. Neurocysticercosis: regression of a fourth ventricular cyst with praziquantel. J Neurol Neurosurg Psychiatry. 1991;54(5):461-462.[Pubmed].
[25]. Zymberg ST, Paiva Neto MA, Gorgulho AA, Cavalheiro S. Endoscopic approach to fourth ventricle cysticercosis. Arq Neuropsiquiatr. 2003;61(2A):204-207. [Pubmed].
[26]. Citow JS, Johnson JP, McBride DQ, Ammirati M. Imaging features and surgery-related outcomes in intraventricular neurocysticercosis. Neurosurg Focus. 2002 Jun 15;12(6):6. [Pubmed].

