Case Report

Sudden death due to cerebral malaria in a Nigerian adult: a rare post mortem finding
1Sunday Soyemi, 1Adedayo Faduyile, 1Olajide Lawal, 1Adokie Benebo, 1John Obafunwa, 1Victor Mordi
- 1Department of Pathology and Forensic Medicine, Lagos State University Teaching Hospital, Ikeja, Lagos, Nigeria
- Submitted: February 09, 2013;
- Accepted March 28, 2013;
- Published: April 04, 2013
This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/3.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Cerebral malaria is uncommonly diagnosed amongst adult in endemic areas in Africa and South-East Asia. It is the most common neurological complication of plasmodium falciparum malaria. It has few specific clinical symptoms with differences in presentation between children and adults. Sequestration of infected red blood cells within cerebral vessels is the main pathological basis of this disease.
We present a case of a- 45 year old Nigerian who died of cerebral malaria despite living all his life in Nigeria (A malaria endemic area for years). Investigation also did not reveal any form of immune suppression.
In this case, autopsy findings show enlarged salty-grey liver and brain with global punctuate hemorrhages in the grey and white matter. Cut surfaces of the slightly enlarged spleen revealed dark red diffluent.
Histopathological examination revealed the presence of parasitized red blood cells with malaria pigment (haemozoin) in blood capillaries within the brain and the lungs.
This case presents a paradox that contradicts the epidemiological impression that the development of immunity during childhood offers protection against severe infection in adult life. It is also presented for pathologists, most importantly forensic pathologist to bear in mind the possibility of an elderly person having cerebral malaria as a cause of sudden death in malaria endemic regions.
Key words
Cerebral malaria, P. Falciparum, parasitized red blood cells.
Introduction
Malaria is a common and potentially fatal disease with an estimate of about 300 million cases yearly and between 1.5 and 2.7 million deaths each year [1].
Of a number of severe manifestations of infection with plasmodium falciparun, Cerebral Malaria is an important cause of malaria mortality worldwide [2] and represents 20% mortality rate in adult and children. It is also an important cause of acute non-traumatic encephalopathy in tropical countries [3].
The incidence of cerebral malaria in known endemic areas is 1-2 cases per 1000 children per year [4]. In areas of intense transmission clinical diseases is rare in children less than six months due to vertical transmission of antibodies from the mother [5] while the burden of the diseases falls on infants in the first two years of their lives [6].
According to the World Health Organization (WHO) definition cerebral malaria is present in a patient who [7]: cannot localize a painful stimulus and with a Glasgow coma scale of 9 or less, has peripheral asexual falciparium parasitaemia and has no other identifiable cause of an encephalopathy. The definition effectively excludes children who have had a single seizure and children with other causes of cerebral dysfunction such as bacterial or viral meningitis or toxic or metabolic encephalopathy [7].
Abnormal corneal reflexes and reduced muscle tone are more frequent in children than in adults [8], in addition to fever, headache, irritability and coma.
Increased intracranial pressure is often seen in children with cerebral malaria which is typically not seen in adults [9]. Other clinical features seen in children with cerebral malaria include hepatosplenomegaly, jaundice, respiratory distress, retinal abnormalities, renal dysfunction, disseminated intravascular coagulation, hypotension, lactic acidosis, hypoglycemia and anemia [10-13].
Cerebral malaria in adult affects multiple organs [14]. Seizures are less common in Southeast Asian adults compared with African children and the incidence seems to be declining generally.
Case Report
Mr. X was a 45 - year old Nigerian businessman who had been residing in South Western Nigeria. He felt sick and was admitted into Lagos State University Teaching Hospital, Ikeja, Lagos in December 2010 with a working diagnosis of hepatic encephalopathy. This diagnosis was based on the severe jaundice, fever and delirium. He died couples of hours later when investigations requested for were yet to be made available.
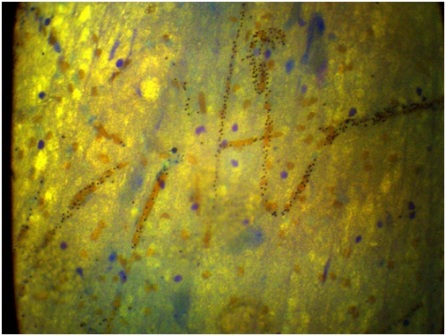
Figure 1: Histological section of the brain shows malaria pigments in cerebral blood vessels. X400 May-Grunwld Giemsa stains.
The body was subjected to a post mortem examination. External examination was that of a black adult with physical appearances consistent with the stated age. The height was 1.85 meters with weight of 92 kg and BMI of 27.8 There were no evidences of trauma or violence. The sclera however, showed marked jaundice.
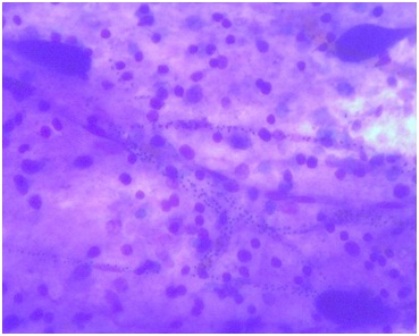
Figure 2: May-Grunwld Giemsa stain showing malaria pigments within cerebral blood vessels Mag x400.
Internal examination revealed slightly enlarged heart of 400 gm with normal valvular lengths. The coronary arteries show normal distribution and are widely patent with no significant artheroma. The epicedium shows petechiae bleedings while the pericardium, endocardium and myocardium were unremarkable.
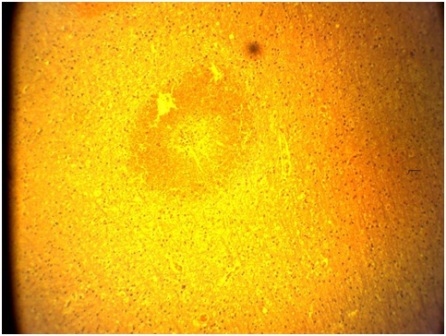
Figure 3: H&E Stain: Section of the brain showing ring hemorrhage, Mag x4.
The Neck structures were also unremarkable with no pleural adhesions or effusion within the chest cavity. The left and right lungs weigh 500 and 550gm respectively. Cut sections show congestion and oedema with no focal lesions.
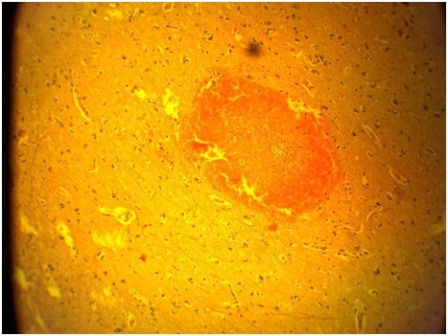
Figure 4: H&E Stain: Section of the brain showing ring haemorrhage within the cortex, Mag x4.
The gastrointestinal systems were generally unremarkable except the salty-grey enlarged liver and spleen which weigh 2050 and 300 gm respectively. Cut surfaces of the moderately enlarged spleen revealed a dark red diffluent.
The brain revealed a salty-grey appearance with weight of 1450 gm. Serial sections of the cerebral hemisphere at 1.0cm interval revealed global punctuate hemorrhage in the gray and white matter.
Histological Examination of the brain revealed capillaries and arterioles packed with parasitized red cells. Ring hemorrhages were also striking features.
Duck’s granuloma which consists of aggregates of parasitized red blood cells, inflammatory cells, and necrotic brain tissue in the perivascular regions were also seen.
Discussion
Consideration for the diagnosis of cerebral malaria should be made in any individual with delirium and fever who lives in malaria endemic region or has recently travelled to malaria endemic areas. However, the diagnosis can be excluded with at least three negative blood smears on microscopy 8-12 hours apart [3]. Although recent study has shown that PCR tests are more sensitive than microscopy, it is usually expensive and do not provide the amount of parasite load [15].
The main pathology in cerebral malaria is the presence of infected and non infected erythrocytes packed within cerebral vessels [3]. Binding of the parasite is mediated by groups of surface antigens expressed on the red cell.The best described of these protein is P falciparum erythrocytes membrane protein-1 (P fEMP1) which is coded for by about 60 variant genes [16].
(P fEMP1) binds to many receptors on endothelial cells of vessels, these include CD36 and intercellular adhesion molecule 1 (ICAM1) [17]. Infected red cells binding to ICAM1 has been implicated in the aetiology of cerebral malaria [18]. This is further corroborated by the up regulation of ICAM1 expression on cerebral vascular endothelium in cerebral malaria [19].
This binding results in sequestration of infected and non- infected erythrocytes and subsequently reducing the cerebral microvasculature flow. The parasite in the erythrocytes also reduces the ability of the red cell to deform, such that red cells have difficulty in passing through the microvasculature [3]. The reduction in cerebral blood flow would cause reduced metabolic substrate to the brain including causing hypoxia. This is further exacerbated by increased demand during seizure and fever, and further complicated in severe anemia [20].
A study done in Thai adults also showed a strong correlation between low red cell deformability and cerebral malaria in adults [21]. The role of increased production of interleukin and tumour necrosis factor in the aetiology of the disease also cannot be over emphasized. This is further supported by a post mortem study of Malawian children with cerebral malaria [22].
Cerebral oedema has also been implicated in cerebral malaria. It was seen in 8 patients out 21 adults in a study in India, two of whom died [23]. In cerebral malaria, most deaths occur within 24 hours and mortality rate both in children and adults is 20% [3]. Deaths usually result from one or combination of the followings: Global cerebral ischemia, multiple organ failure, Transtentorial herniation and brainstem compression.
In a Nigerian study, four out of seven children had cerebral oedema or features of herniation at autopsy [24]. It has been shown that most adults usually die of renal failure or pulmonary oedema [3]. In this case presentation, there was pulmonary oedema, cerebral oedema, ring hemorrhage within brain parenchyma and hepatosplenomegaly.
Death most likely occurred from respiratory failure either from pulmonary oedema or from compression of brain stem as a result of cerebral oedema.
Consent
Consent was obtained from the department. This is for the publication of case report and accompanying images.
Authors' Contribution
SSS: Is a post-fellowship senior registrar who performed the literature search and prepared the manuscript.
LOL: Performed the autopsy and grossed the specimen.
FFA, BAS: Supervised the autopsy.
VPNM, OJO: are professors of pathology who supervised, reviewed the autopsy and reported the microscopic findings.
Conflict of Interests
The authors declare that they have no competing interests.
Acknowledgement
We thank the histotechnologist who prepared the slides and the morticians who assisted during the autopsy. We are grateful to the department for given us the approval to report this case.
References
[1]. World Health Organisation. World malaria situation in 1994. WHO wkly Epidemic Rec 1997;72: 269 -74. [Pubmed].
[2]. Makani J, Matuja W, Liyombo E, Snow RW, Marsh R, and Warrell DA. Admission diagnosis of cerebral malaria in adults in an endemic area of Tanzania: implication and clinical description. QJM 2003: 96(5): 355-362. [Pubmed].
[3]. Idro R, Jenkins NE, Newton CRJ. Pathogenesis, clinical features and neurological outcome of cerebral malaria. Lancet Neurol 2005;4: 827-40. [Pubmed].
[4]. Snow RW, Craig MH, Newton CRJC, Steketee RW. The public health burden of plasmodium falciparum malaria in Africa: deriving the Working paper No 11. Diseases control priorities project, Bethesida, MD: Forgarty International center, National Institutes of Health, August 2003.
[5]. Newton CR, Krishna S. Severe falciparium malaria in children. Current understanding of pathophysiology and supportive treatment. Pharmacolther 1998;79: 1-53. [Pubmed].
[6]. Reyburn H, Mbatia R, Drakeley C, et al. Association of transmission intensity and age with clinical manifestation and case fatality of severe falciparum malaria. JAMA 2005; 293: 1461-70. [Pubmed].
[7]. Severe falciparum malaria. World Health Organisation (WHO) communicable disease clusters. Trans R soc Trop Med Hyg – 2000; 94 (Suppl 1): 51-590. [Pubmed].
[8]. Newton CR, Taylor TE, whitten RO. Pathophysiology of fatal falciparum malaria in African children. Am J Trop Med Hyg 1998;58: 673-683. [Pubmed].
[9]. Newton CR, Crawley J, Sowunmi A, et al. Intracranial hypertension on Africans with cerebral malaria .Arch Dis child 1997; 76: 219-226. [Pubmed].
[10]. Molyneux ME, Taylor TE, Winma JJ, Borgstein A. Clinical features and prognostic indications in paediatric cerebral malaria: a study of 131 comatoses in Malawian children. QJ Med 1989; 71: 441-459. [Pubmed].
[11]. Waller D, Krishna S, Crawley J, et al. Clinical features and outcomes of severe malaria in Gambian children. Clin infect Dis 1995; 21:577-587. [Pubmed].
[12]. Esomai F, Nabakwe E, Mining et al. Clinical presentation and diagnosis of cerebral malaria in children in the highlands of Western Kenya. East Afr Med J 1999; 76: 9-92. [Pubmed].
[13]. Olumese PE,Gbadegesin RA, Adeyemo AA, et al. Neurological features of cerebral malaria in Nigerian children. Ann Trop Paediatr. 1999;19: 321-325. [Pubmed].
[14]. Newton CR, Hien TT, White N. Cerebral malaria. J Neurol Neurosurg Psychiatry 2000; 69:433-441. [Pubmed].
[15]. Farnert A, Arez AP, Babiker HA, et al. Genotyping of Plasmodium falciparum infections by PCR: a comparative multicentre study.Trans R Soc Trop Med Hyg 2001; 95: 225–32. [Pubmed].
[16]. Roberts DJ, Craig AG, Berendt AR, et al. Rapid switching to multiple antigenic and adhesive phenotypes in malaria. Nature 1992; 357: 689–92. [Pubmed].
[17]. Craig A, Scherf A. Molecules on the surface of the Plasmodium falciparum infected erythrocyte and their role in malaria pathogenesis and immune evasion. Mol Biochem Parasitol 2001; 115: 129–43. [Pubmed].
[18]. Berendt AR, Simmons DL, Tansey J, Newbold CI, Marsh K. Intercellular adhesion molecule-1 is an endothelial cell adhesion receptor for Plasmodium falciparum. Nature 1989; 341: 57–59. [Pubmed].
[19]. SenGupta SK, Naraqi S. The brain in cerebral malaria: a pathological study of 24 fatal cases in Papua New Guinea. P N G Med J 1992; 35: 270–74. [Pubmed].
[20]. Idro R. Severe anaemia in childhood cerebral malaria is associated with profound coma. Afr Health Sci 2003; 3: 15–18. [Pubmed].
[21]. Dondorp AM, Angus BJ, Hardeman MR, et al. Prognostic significance of reduced red blood cell deformability in severe falciparum malaria. Am J Trop Med Hyg 1997; 57: 507–11. [Pubmed].
[22]. Brown H, Rogerson S, Taylor T, et al. Blood-brain barrier function in cerebral malaria in Malawian children. Am J Trop Med Hyg 2001;64: 207–13. [Pubmed].
[23]. Patankar TF, Karnad DR, Shetty PG, Desai AP, Prasad SR. Adult cerebral malaria: prognostic importance of imaging findings and correlation with postmortem findings. Radiology 2002; 224: 811–16. [Pubmed].
[24]. Walker O, Salako LA, Sowunmi A, Thomas JO, Sodeine O, Bondi FS. Prognostic risk factors and post mortem findings in cerebral malaria in children. Trans R Soc Trop Med Hyg 1992; 86: 491–93. [Pubmed].

