Case Report

Infantile (Desmoid type) Anterior Mediastinal Fibromatosis-A Case Report
1,S. K. Andola, 1Vatsala Kishore, 1S. J Rajshekhar 2, Shivanand Melkundi, 3S. R. Harwal
- 1Department of Pathology, M. R. Medical College, Gulbarga, India
- 2Department of Radiology, M. R. Medical College, Gulbarga, India
- 3Department of Surgery, M. R. Medical College, Gulbarga, India
- Submitted July 4, 2014
- Accepted:Thursday, July 31, 2014
- PublishedWednesday, September 03, 2014
This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/3.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited
Abstract
Introduction
Desmoid-type fibromatosis is fibroblastic proliferation occurring in the deep soft tissues and is characterized by infiltrative growth and tendency towards local recurrence but does not metastasize. It represents 3.5% of fibrous tumors and 0.03% of all neoplasms. Desmoid fibromatosis are rare in children, may occur in head and neck region but are extremely rare in the mediastinum with only five cases being reported in the literature till date. This case is being presented for its rarity
Case presentation
Three year old male child presented with a gradually progressive, firm 17x10cm swelling, fixed to the chest wall with dilated veins. Radiological imaging revealed possibility of soft tissue sarcoma/Ewing’s sarcoma. Cytological diagnosis of spindle cell tumor of intermediate grade, possibly of neuronal origin was made. Thoracotomy and excision of tumor was performed. Grossly there was a single, partially skin covered, grey white mass measuring 17x10x5cm, C/s showing grey white areas of whorling and cartilage projections. Microscopically interlacing fascicles of bland spindle cells in a collagenous background were seen with fusiform nuclei, uniform chromatin and inconspicuous nucleoli. No pleomorphism, mitoses were seen. Surrounding adipose tissue and bone was infiltrated by tumor. On Immunohistochemistry the tumor showed diffuse positivity for vimentin, focal positivity for S-100 and was negative for desmin. A diagnosis of mediastinal fibromatosis was made. However, the Patient succumbed to intraoperative cardiac arrest.
Conclusions
Fibromatosis should be considered in differential diagnosis of any spindle cell tumor of anterior mediastinum. It is impossible to give a preoperative definite diagnosis of fibromatosis on FNAC but with a core needle biopsy and IHC, the differential diagnoses can be narrowed.
Key words
Fibromatosis, Infantile, Mediastinum, Desmoid Tumor
Introduction
Mesenchymal tumors, either benign or malignant are rare in the mediastinum, constituting less than 2% of all mediastinal tumors and tumor-like lesions. Fibromatosis, otherwise known as desmoid tumor, is one type of mesenchymal tumors [1]. Desmoid-type fibromatoses of the deep tissue are rare soft tissue tumors characterized by proliferation of fibroblast and myofibroblast-type spindle cells, which infiltrate musculoaponeurotic tissue. They represent 3.5% of fibrous tumors and 0.03% of all neoplasms [2]. Only five cases of anterior mediastinal desmoid fibromatosis have been reported in the literature till date [3]. Although they are considered to be benign tumors, they are aggressive locally with a high risk of local recurrence after surgical excision, but do not metastasize[2]. The estimated incidence of desmoid tumors in general population is 2 -4 new cases per million per year [4]. The peak incidence among pediatric patients occurs between 5 to 8 years of age[5]. . In newborns and infants, most frequent sites are extremities and head & neck with higher incidence in males than females. The principal sites of involvement in fibromatosis are the shoulder, thigh, arm, back and buttocks [1].
Case presentation
A three year old male second born child presented with a gradually progressive swelling on left anterior chest wall since 14 months. Other sibling was normal. On examination swelling was firm measuring 17x10 cm size and fixed to the chest wall, prominent and dilated veins were noted over the chest (figure 1a). Radiological imaging revealed a fairly large anterior mediastinal solid mass measuring 9.1x8.6 cm with extrathoracic extension and erosion of left 3rd and 4th ribs on left side (figure 1b) displacing mediastinal structures, cardia and major vessels posteriorly with no nourishing vessels and possibility of soft tissue sarcoma/Ewing’s sarcoma was considered. On FNAC, aspirate revealed pleomorphic spindle cells with wavy cytoplasm and fusiform nucleus, many cells with hyperchromatic nucleus and 1-2 small nucleoli along with few binucleate and multinucleate cells (figure 1c ). No necrosis or mitosis was seen. A cytological diagnosis of spindle cell tumor of intermediate grade, possibly of neuronal origin, was made. Intraoperatively tumor was involving ribs and part of sternum. Thoracotomy and excision of tumor was performed by excision of ribs and part of sternum and separation of tumor from pericardium by blunt dissection. Residual tissue was left over pericardium and around great vessels. Patient suffered multiple cardiac arrests during surgery and succumbed to it. The specimen was sent for histopathological examination.
Grossly a single, partially skin covered, grey white mass measuring 17x 10 x5 cm was received (figure 1d). The cut section revealed grey white whorl like areas and cartilage projections (figure 1e). H&E stained sections revealed well circumscribed, unencapsulated mass with interlacing fascicles and clusters of bland fibroblasts in a dense collagenous stroma (figure 2a). The cells were spindle shaped with moderate eosinophilic cytoplasm and elongated nucleus with vesicular chromatin and inconspicuous nucleoli (figure 2b). These cells were also infiltrating into the surrounding adipose tissue and focally encroaching upon bony fragments i.e. ribs (figure 2c, d). Mitosis was 0-1/10 HPF. Immunohistochemical staining revealed diffuse positivity for vimentin (figure 3a), focal positivity for S-100 (figure 3b) and negative staining for desmin. A final diagnosis of mediastinal fibromatosis was made.
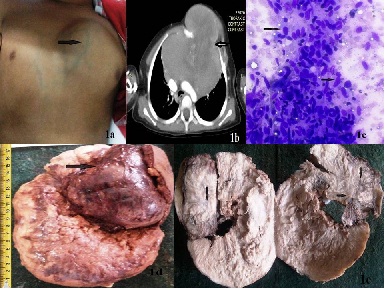
Figure 1: Showing clinical, radiological and gross pathological findings. A) Swelling measuring 17x 10 cm size with dilated veins noted over the chest; B) Contrast enhanced CT scan showing large anterior mediastinal solid mass with extrathoracic extension and erosion of left 3rd and 4th ribs; C). Photomicrograph of FNAC showing pleomorphic spindle cells with wavy cytoplasm and fusiform nucleus, many cells with hyperchromatic nucleus and 1-2 small nucleoli (Giemsa x400); D) Partially skin covered, grey white mass measuring 17x10 x5 cm; E) Cut section revealed grey white whorl like areas and cartilage projections
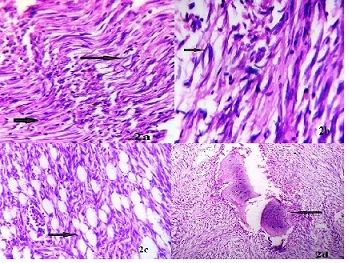
Figure 2: Photomicrograph showing hematoxylin eosin staining: A) H&E stained sections revealed well circumscribed, unencapsulated mass with interlacing fascicles and clusters of bland fibroblasts in a dense collagenous stroma (H&Ex100); B) The cells were spindle shaped with moderate eosinophilic cytoplasm and elongated nucleus with vesicular chromatin and inconspicuous nucleoli(H&Ex400); C) The tumor cells were also infiltrating into the surrounding adipose tissue(H&Ex100); D) Tumor cells focally encroaching upon bony fragments(H&Ex100)
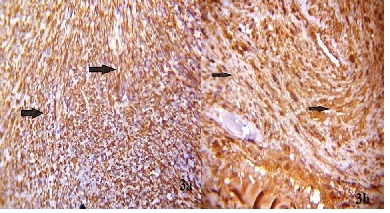
Figure 3: Photomicrograph showing Immunohistochemical staining A) diffuse positivity for Vimentin (x400); B) focal positivity for S-100 (x400)
Discussion
called deep fibromatoses, were first described in the abdominal wall by Mac Farlane in 1832. Extra-abdominal types were described later, in particular in the limbs and the scapular belt. Tumors in the chest wall have only been reported in 10 to 20% of cases, while anterior mediastinal locations are very rare [1, 2].
The generic term fibromatosis was originally proposed by Stout, for a group of related conditions having the common features as proliferation of well-differentiated fibroblasts, infiltrative pattern of growth, presence of a variable (but usually abundant) amount of collagen between the proliferating cells, lack of cytologic features of malignancy, scanty or absent mitotic activity, aggressive clinical behavior characterized by repeated local recurrences but lack of capacity to metastasize distantly [6].
The fibromatosis can be broadly divided as- Superficial (fascial) and deep fibromatosis. In addition to the typical forms of deep fibromatosis, several specific types are known in children which differ in their clinical presentations. These are classified as-Fibrous hamartoma of infancy, Infantile digital fibromatosis, fibromatosis colli, infantile myofibromatosis, infantile (desmoid type) fibromatosis, hyaline fibromatosis, gingival fibromatosis and calcifying aponeurotic fibromatosis [7].
Desmoid type fibromatosis of deep tissues are rare soft tissue tumors representing 3.5% of fibrous tumors and 0.03% of all neoplasms [2]. Clinically they are deep seated, firm, poorly circumscribed slow growing, painless mass which can cause decreased mobility of adjacent joints and neurologic complications like tingling, numbness, shooting pain if tumor compresses the nearby nerves. Symptoms are rare and result mainly from the local mass effect of tumor encroachment on vital structures or erosion of adjacent bone or joint tissue. Radiologically it presents as soft tissue mass that interrupts the adjacent intermuscular and soft tissue planes and it may encroach on adjacent bones causing pressure erosion [3 5 8].
Grossly the tumor is confined to musculature and overlying aponeurosis or fascia but large tumors may infiltrate the subcutaneous tissue and occasionally cause bone erosion [1 2 3].
Microscopically, tumor consists of proliferating fascicles of elongated, slender, spindle shaped fibroblasts of uniform appearance, surrounded and separated by abundant collagen with little or no cell to cell contact. Constituent nuclei are small, pale staining, sharply defined with inconspicuous nucleoli. Nuclei lack hyperchromasia or atypia and cellularity varies from area to area within the tumor [1 2 3] Immunohistochemically the spindle cells stain with vimentin, smooth muscle actin and beta catenin. Some also stain focally with desmin and S-100 [3 9]. In the present case, immunohistochemical stains revealed diffuse positivity for vimentin, focal positivity for S-100 and negative staining for desmin.
Ultrastructural studies show that these tumor cells are mainly fibroblasts with some myofibroblasts. Histologically, reactive fibrosis and fibrosarcoma should be primarily considered in the differential diagnosis of fibromatosis. The lesions of reactive fibrosis may closely resemble fibromatosis, though they exhibit more variable growth patterns and the presence of focal hemorrhage. Factors against fibrosarcoma are the uniform growth pattern, mature appearance of tumor cells, and the paucity of mitotic figures [1].
Despite bland microscopic appearance, this tumor frequently behaves in a locally aggressive manner, often recurs and rarely causes death only if it invades or compresses a vital structure [4,8].
In the present case, though the histological features were more of benign nature but there was involvement of bone and adjacent soft tissue in an aggressive manner and the patient died because of postoperative complications.
Treatment of choice is wide local excision and Post operative radiotherapy, if tumors are incompletely excised. Regular follow-up imaging is mandatory even when surgical margins are free of tumor. Reexcision is recommended for local recurrent disease. Other treatment methods, including radiation, chemotherapy, c-AMP modulation, estrogens, and prostaglandin inhibition, have been tried with varying success [8]. The prognosis of fibromatosis is generally quite favorable with a 5-year survival rate of more than 90% but the outcome seems to be dependent on the location of the tumor [1,3].
Conclusion
Fibromatosis can occur in anterior mediastinum, can attain large size, be well circumscribed, have extensive hypocellular and myxoid region. Therefore it should be considered in differential diagnosis of any spindle cell tumor of anterior mediastinum. It is impossible to give preoperative definite diagnosis of fibromatosis in FNAC and core needle biopsy but with immunohistochemical study, list of differential diagnoses can be narrowed. Although it is considered to be a benign lesion, this tumor can be locally very aggressive, and has a high local recurrence rate depending upon the efficacy of surgical resection. This case is being presented for its rarity with only few cases reported in the literature.
Learning Point
For the mediastinal tumors a core needle biopsy is mandatory before deciding treatment option. If a soft tissue tumor is suspected on H & E staining, further immunohistochemical staining and molecular analysis should be done. Any attempts at unplanned treatment should be avoided.
Conflict of Interests
The authors declare that there are no conflicts of interests.
Ethical Considerations
Written informed consent was obtained from the patient’s father for publishing this case report
Author’s contribution
SKA: Contributed to the pathological diagnosis, literature search, drafting and edited the final manuscript.
VK: Literature search and drafting of manuscript.
RSJ: Literature search and interpretation of results.
SM: Helped in radiological diagnosis
SRH: Operated on patient & provided clinical details
All authors read and approved the final manuscript for submission.
Acknowledgement
None
References
[1].Inase N, Ichioka M, Akamatsu H, Usui Y, Miyake S, Yoshizawa Y. Mediastinal fibromatosis presenting with superior vena cava syndrome. Respiration. 1999;66(5):464-6. [PMID: 10516545[[Pubmed]
[2].Zehani-Kassar A1, Ayadi-Kaddour A, Marghli A, Ridene I, Daghfous H, Kilani T, El Mezni F. Desmoid-type chest wall fibromatosis. A six cases series. Orthop Traumatol Surg Res. 2011 Feb;97(1):102-7. doi: 10.1016/j.otsr.2010.09.017. Epub 2011 Jan 15. [PMID: 21239240][Pubmed]
[3]Sanei MH, Tabatabaie SA, Mahzooni P, Sanei B. A large anterior medistinal fibromatosis. Case Rep Clin Pract Rev 2006; 7: 100-102.
[4]. Lakhan SE, Eager RM, Harle L. Aggressive juvenile fibromatosis of the paranasal sinuses: case report and brief review. J Hematol Oncol. 2008 May 28;1:3. doi: 10.1186/1756-8722-1-3. [PMID: 18577255]
[Pubmed]
[5]Honeyman JN1, Quaglia MP. Desmoid tumors in the pediatric population. Cancers (Basel). 2012 Mar 9;4(1):295-306. doi: 10.3390/cancers4010295. [PMID: 24213241
[Pubmed]
[6]Stout AP. Juvenile fibromatosis. Cancer 1954; 7: 953-978
[7]Sailukar MG, Yuvraja TG, Ramadwar MR, Kurkure PA, Tongaonkar HB. Infantile Fibromatosis of Scrotum. Indian J Surg.2005;67:273-5. http://www.bioline.org.br/pdf?is05085
[8].Saw E, Yu GS, Mell M. Desmoid tumor of the sternum presenting as an anterior mediastinal mass. Eur J Cardiothorac Surg. 1997 Feb;11(2):384-6. [PMID: 9080173
[Pubmed]
[9].Kim NR, Chung DH, Lee JI, Jeong SH, Ha SY. Intrathoracic desmoid tumor mimicking pleural mass: A case report. Tuberc Respir Dis. 2009 Nov; 67(5):449453.http://dx.doi.org/10.4046/trd.2009.67.5.449

