Case Report

Giant cystic Lymphangioma of Pancreas –A Rarity
1 Cicy P. J.,2 Sansho E. U., 1 Lekshmidevi P, 2 Philip Umman, 22Sandeep Varghese,2 John S. Kurien
- 1.Department of Pathology, Govt. Medical College, Kottayam, Kerala, India.
- 2.Department of Surgery, Govt. Medical College, Kottayam.
- Submitted Tuesday, July 29, 2014
- Accepted:Thursday, September 04, 2014
- PublishedSunday, September 14, 2014
This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/3.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited
Abstract
Lymphangiomas are rare benign neoplasms common in head and neck region. Intraabdominal lymphangiomas are rare and pancreatic cystic lymphangiomas (PCLs) account for only 1%of such neoplasms. To the best of our knowledge only about 75 cases have been reported including this case and the average size was 20cms.Though benign, PCLs can cause severe abdominal discomfort and may even rupture. Here we report a case of PCL in a 21 yr old male who presented with abdominal pain and epigastric mass .Clinicoradiological evaluation revealed a multicystic septate mass in association with the pancreas about 40x30cms.With the preoperative differential diagnosis of pseudocyst pancreas/cystic neoplasm we proceeded with exploratory laparotomy. A distal pancreatectomy and splenectomy was done since the lesion was arising from the body of the pancreas. Histological examination revealed a multicystic lesion lined by endothelial cells with lymphocytes in the wall and the diagnosis of PCL was made.
Key words
Cystic, Distal pancreatectomy, Lymphangioma, Pancreas
Introduction
PCLs are rare neoplasms and usually present as a palpable mass or vague abdominal pain. They constitute only 0.2% of pancreatic neoplasms and show a female predilection (29:16). Our case was of a 21yr old male and the size was 40x30cm.Though Lymphangiomas can attain any size review of literature shows that most were below 40cm.
Case report
A 21yr old male admitted with fullness of abdomen early satiety and decreased appetite of 2 weeks duration. He had jaundice 6 months back but no medical records are available. History of alcoholism was present but stopped 6 months back. There was no associated history of vomiting, loss of weight, TB or any other illness.
General examination was normal. Abdominal examination showed distended abdomen with flanks full and dilated veins over the anterior abdominal wall. Abdomen was non tender, tense with fluid thrill, and without any shifting dullness or any definitive mass or pulsations. Hernial orifices, external genitalia and supraclavicular areas were normal. Distal pulsations were normally palpable. Bowel sounds were normally present. All other systemic examinations were normal. All the routine investigations, liver function tests, renal function tests, random blood sugar, serum amylase and lipase were normal.
Radiological Evaluation
Chest X-ray was normal. USG abdomen revealed a large complex cystic lesion suggestive of pseudocyst of the pancreas, CECT abdomen (Figure 1). suggested a large intra peritoneal cystic lesion possibly a pancreatic pseudocyst.
Figure 1: Suggests large intraperitoneal cysticlesion possibly Pseudo cyst pancreas
After Clinico-radiological discussion, with the differential diagnosis of pseudocyst pancreas/cystic neoplasm we decided to do exploratory laparotomy for the patient.
Intra operative findings
The picture below shows the appearance of the lesion on midline laparotomy (Figure 2).

Figure 2: Shows the appearance of lesion on midline laparotomy
Multiloculated cystic lesion of 40x30 cm size in the Supra colic Compartment (Figure 3) arising from the body of pancreas and encasing middle colic artery ,vein and Superior Mesenteric Vein. Stomach was pushed Antero superiorly with a definite plane between stomach & the cyst. Rest of the viscera was normal. We had to decompress the larger cyst to do excision of cyst with distal pancreatectomy and splenectomy (Figure 4)

Figure 3: suggests the bulge in the transverse Meso colon which is pushed down due to the giant cystic mass
Figure 4: Picture showing the resected specimen
Pathological Findings
Gross examination revealed a partially collapsed cystic mass with pancreatic tissue and spleen. Cut section showed a multicystic septate mass with most of the locules filled with sero sanguinous fluid.
Microscopy revealed multiple cystic spaces lined by flattened endothelial cells, lumen showing eosinophilic secretions. Intervening stroma showed lymphocytic collections smooth muscles, fibrocollagenous tissue; cholesterol cleft formation and giant cell reaction. Pancreatic acini were seen in the periphery and also in between the cystic spaces (Figure 5) Immunohistochemistry revealed CD34 positivity for the lining cells (Figure 6).
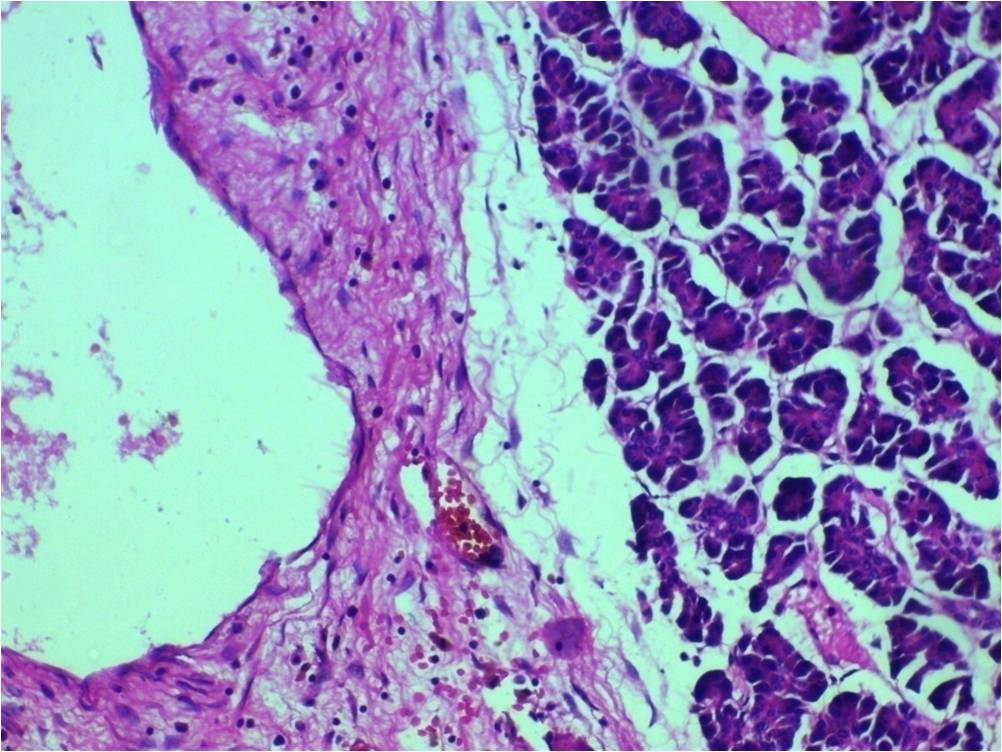
Figure 5: shows cystic spaces with endothelial lining and pancreatic acini
in the periphery.
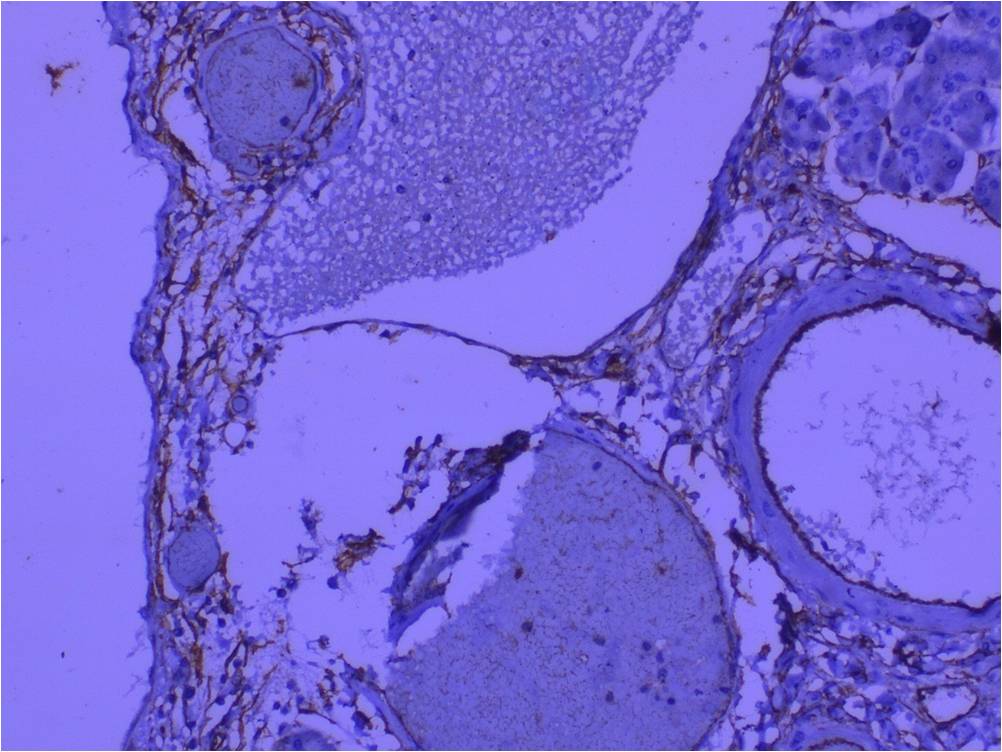
Figure 6: IHC showing CD34 positivity for the lining cells
Discussion
Lymphangiomas are benign tumors developing from congenital malformations of lymphatic vessels. The etiology in adults is thought to be lymphatic obstruction secondary to trauma or inflammation [1]. Though common in head and neck region, pancreas is a rare site. To term it as Pancreatic Cystic Lymphangioma (PCL), the neoplasm should arise within the pancreatic tissue substance or should be attached to the pancreas by a pedicle or should be adherent to it [2].
Histologically, lymphangiomas are of three types.- cystic, cavernous and capillary. Most reported cases are of cystic type. Any age group is affected but the mean age group is 40 years, with a wide range from 2-81 years [3]. Females are more affected than males (29:16) [3]. Macroscopically they are soft cystic masses filled with serous or
serosanguinous or lymphatic fluid [4].Rarely phlebolith like calcification may be present. Histology shows interconnected vascular channels of varying sizes separated by thin septae. The vascular spaces are lined by endothelial cells positive for CD31,CD34 or D240 (specific marker) [5] and the walls contain variable amounts of collagen, connective tissue, irregular smooth muscle fascicles, occasional adipocytes and lymphocytic collections. The smooth muscles found in the wall of a cyst in combination with lymphocytes both in the wall and vascular lumina are most suggestive of diagnosis.
The common presentations are as palpable masses or abdominal pain. Smaller lesions are asymptomatic and are detected incidentally during imaging or surgery for unrelated diseases. Vomiting and nausea are infrequent symptoms and rarely PCLs can present as acute abdomen [6 7 8 9 ]. Since first reported by Koch et al., in 1913
[10 ]only less than 100 cases have been reported till date. Sonological studies can reveal a multi cystic
septate mass. CECT abdomen can provide additional information about the capsule, septations of the cyst, its thickness and the characteristics of the fluid within [11]. However a definitive diagnosis cannot be made preoperatively by imaging alone. Some authors suggest the use of Endoscopic Ultrasound guided FNA study of cyst fluid for preoperative diagnosis [12 13 14]. But in our case it was not done because the clinical differentials considered were pseudocyst pancreas and other cystic neoplasms of pancreas like serous and mucinous cystadenomas. More over due to the huge size and symptoms an immediate surgery was planned. Huge PCLs can cause a significant discomfort with compression of adjacent organs. Ideally a complete surgical resection is mandatory to prevent recurrence (7%) [15]. In our case in order to obtain a complete resection, we did a distal pancreatectomy along with splenectomy. Follow-up USG abdomen and random blood sugar level after two years are within normal limits.
Conclusion
PCLs are very rare benign cystic neoplasms of the abdomen. Although rare, this should be considered in the differential diagnosis of multicystic lesions of pancreas especially those presenting as abdominal masses. Surgical excision is the only known modality of treatment and is usually curative with excellent prognosis.
Authors' Contribution
CPJ: Conception, preparation of manuscript and final approval
of the version to be published.
SEU: Conception and design of manuscript.
Drafting the article and revising it critically for important intellectual
content
LDP: Conception, design and preparation of manuscript
PU:
Conception, design and preparation of manuscript
SV: Conception and design
of manuscript
JSK: Design and preparation of manuscript
Conflict of Interests
The authors declare that there are no conflicts of interests.
Ethical Considerations
The written informed consent was obtained for publication of
your case reports.
Funding
None
Acknowledgement
None
References
[1].Colovic RB, Grubor NM, Micev MT, Atkinson HD, Rankovic VI, Jagodic MM. Cystic lymphangioma of the pancreas. World J Gastroenterol, 2008; 14: 6873–6875 [Pubmed]
[2].Casadei R, Minni F, Selva S, Marrano N, Marrano D. Cystic lymphangioma of the pancreas: anatomoclinical, diagnostic and therapeutic considerations regarding three personal observations and review of the literature. Hepatogastroenterology 2003; 50:1681-6.
[3].Igarashi A, Maruo Y, Ito T, Ohsawa K, Serizawa A, Yabe M, Seki K, Konno H, Nakamura S. Huge cystic lymphangioma of the pancreas: report of a case. Surg Today. 2001; 31: 743–746. [Pubmed]
[4].Koenig TR, Loyer EM, Whitman GJ, Raymond AK, Charnsangavej C. Cystic lymphangioma of the pancreas. Am J Roentgenol. 2001;177:1090-1090 [Pubmed]
[5].Gray G, Fried K, Iraci J. Cystic lymphangioma of the pancreas: CT and pathologic findings. Abd Imaging, 1998; 23: 78–80,. [Pubmed]
[6].Allen JG, Riall TS, Cameron JL, Askin FB, Hruban RH, Campbell KA. Abdominal lymphangiomas in adults. J Gastrointestinal Surg, 2006; 10: 746–751 [Pubmed]
[7].Kawaguchi K, Motoi F, Ohtsuka H, Fukuyama S, Rikiyama T, Katayose Y, Egawa S, Satoh M, Asakura T, Shimosegawa T, Unno M. Cystic limphangioma of the pancreas with spontaneous rupture: report of a case. Report Gastroenterol, 2011; 5: 288–294 [Pubmed]
[8].Goh BK, Tan YM, Yap WM, Wong CY. Hemorrhage into a pancreatic lymphangioma after blunt trauma mimicking a post-traumatic pancreatic pseudocyst. J Trauma Injury Infection Critical Care, 2006; 61: 992–994. [Pubmed]
[9].Ghatak S, Ray S, Sanyal S, Sonar PK, Khamrui S, Basu K, Ray S, Das K. An unusual cause of acute abdomen in adults: giant cystic lymphangioma of the pancreatic head. A clinical case and literature review. J Pancreas, 2011; 12: 266–270. [Pubmed]
[10].Koch K. Beiträge zur Pathologie der Bauchspeicheldrüse. Virchows Archiv für pathologische Anatomie und Physiologie und für klinische Medizin. 1913; 214:180-206. [Full text]
[11].Yüceyar S, Kapan M, Ozben V, Ertürk S, Aydin I, Kepil N. Pancreatic cystic lymphangioma: Report of a case. Turk J Gastroenterol 2009; 20 (3): 228-230 [Pubmed]
[12].Schneider G, Seidel R, Altmeyer K, Remberger K, Pistorius G, Kramann B, Uder M. Lymphangioma of the pancreas and the duodenal wall: MR imaging findings. Eur Radiol, 2001; 11: 2232–2235 [Pubmed]
[13].Bhatia V, Rastogi A, Saluja SS, Kumar M, Bihari C, Kalayarasan R, Gupta NL. Cystic pancreatic lymphangioma. The first report of a preoperative pathological diagnosis by endoscopic ultrasound-guided cyst aspiration. J Pancreas, 2011; 12: 473–476.[Pubmed]
[14].Coe AW, Evans J, Conway J. Pancreas cystic lymphangioma diagnosed with EUS-FNA. J Pancreas 2012; 13: 282-284 [Pubmed]
[15].Dalla Bona E1, Beltrsame V, Blandamura S, Liessi F, Sperti C. Huge cystic lymphangioma of the pancreas mimicking pancreatic cystic neoplasm. Case Rep Med. 2012; 2012: 951358. doi: 10.1155/2012/951358 [Pubmed]

