Case Report

Krukenberg Tumor arising from Bilateral Lobular Carcinoma in a Pregnant Lady: A Rare Case Report.
*T Santosh, E S Rao, *B R M Rao, *R V Kumar,
- *Pathology, KIMS &RF, Amalapuram AP, India
- Submitted: Friday, July 18, 2014
- Accepted: Sunday, August 17, 2014
- Published:Sunday, November 16, 2014
This is an Open Access article distributed under the terms of the Creative Commons Attribution License ((http://creativecommons.org/licenses/by/3.0)which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited
Abstract
Metastatic ovarian tumors are thought to account for approximately 10–30% of malignant ovarian tumors. Krukenberg tumor refers to a malignancy in the ovary that metastasized from a primary site, classically the gastrointestinal tract, although it can arise in other tissues such as the breast (approx. 04%). Krukenberg tumor during pregnancy arising from breast is even rarer (0.1 - 0.2%).The presence of adnexal masses during pregnancy ranges from 1:81 to 1:2,500 pregnancies, but only 3% of these masses are malignant. Management of such cases can present as diagnostic & treatment dilemma. We report a case of 25 year primiparous female with Krukenberg tumor of breast origin.
Keywords
Krukenberg tumor, Pregnancy, Breast, Invasive Lobular carcinoma, IHC.
Introduction
Krukenberg tumors are defined as tumors characterized entirely or prominently by the presence of mucin-filled signet ring cells, typically lying within a cellular stroma derived from the ovarian stroma & metastasized from a primary site, classically the gastrointestinal tract, although it can arise in other tissues such as the breast [1]. Krukenberg tumors are often (over 80%) found in both ovaries, consistent with its metastatic nature [2]. They account for about 1-6% of ovarian tumors and 10-30% of malignant ovarian tumors.In both Asia and the West, most metastatic ovarian tumors originate from the gastrointestinal tract but is relatively less common from breast primary [3, 4]. Krukenberg tumor during pregnancy arising from breast is even rarer (<0.2%). Their diagnosis & management can present a dilemma for the pathologists & obstetrician [5].
Case Presentation
A 25 year female G1 P0 (28 weeks) was admitted to the labor room with complaints of severe abdominal pain. Clinical examination revealed abdominal fullness & tenderness. Routine investigations were all normal, except CA-125-- 230 U/ml, mild anemia. USG abdomen pelvis showed a single live fetus of mean gestational age 28 weeks +/- 1 week with an isoechoiec lesion (11 x 10 x 4cms) in maternal POD. Laparotomy was done showing B/L ovarian tumors (Figure 1). We received the specimens in the histopathology department with a clinical diagnosis of B/L ovarian carcinoma. On gross examination (Figure 2) both ovaries were seen to have maintained normal contours, measuring 11x18x7 cm (right) & 8x7x4 cm (left), cut surface was solid & grey white in color with areas of hemorrhage. Histology of both ovaries showed groups & sheets of signet ring cells in a fibrous background with focal pseudo lobule formation in both ovaries, signet ring cells were PAS positive (Figure 3). A diagnosis of B/L ovarian Krukenberg tumor was made & advised to search for primary.

Figure 1: Laparotomy with B/L ovarian masses

Figure 2: Gross Of Right Ovary [11x8x7 cms] showing maintenance of normal contour with solid, grey white c/s with Left Ovary (inset).
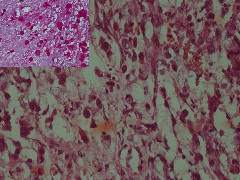
Figure 3: Groups & sheets of signet ring cells in a fibrous background (H&E 40X) with PAS positive signet ring cells (inset).
During re-evaluation of the patient, Esophagogastroduodenoscopy and colonoscopy revealed no significant abnormal lesions. Through clinical examination of the patient revealed ill-defined lumps in both breasts. The masses were located symmetrically in the upper quadrant with irregular outline; with size of 3 cm in the right and 4 cm in the left breast. FNA & Biopsy from both breasts show features of invasive lobular carcinoma (Figure 4&5). IHC of ovarian tumor shows strong nuclear positivity for ER (6/8), negative for PR (2/8) on the basis of Allred scoring system, negative for HER-2/neu , positive for CK & PAS (Figure 6).. A final diagnosis of B/L Krukenberg tumor of ovaries with primary of breast carcinoma (B/L) - lobular variant was given. The patient was given 1st dose of Paclitaxel and carboplatin chemotherapy then she underwent caesarean section at 34 weeks of gestation. She is then under follow up for remaining 5 cycles of chemotherapy.
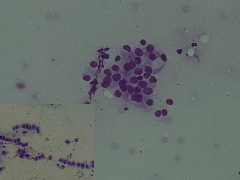
Figure 4:Cytosmear shows low cellularity, small groups of epithelial cells with hyperchromatic nucleus occasional signet ring cells, indian file pattern( inset) Diff Quik(40X).
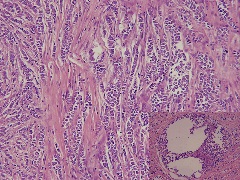
Figure 5: Classic indian file pattern of tumor cells with foci of LCIS (inset). (H&E 40X)
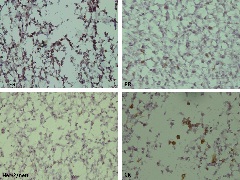
Figure 6: ER strong nuclear positivity, PR & Her-2neu negative , CK positive (IHC 40X)
Discussion
Krukenberg-type tumors are rare among ovarian metastases. They are responsible for the most frequent diagnostic confusions with primary ovarian cancer. The eponym of this condition was given by Krukenberg initially described in 1896 and the criteria given were (1) the presence of a tumor in the ovary, (2) evidence of intracellular mucin secretion by the formation of signet cells, & (3) diffuse infiltration of stroma giving a sarcoma-like appearance [6].They are peculiar tumors with uncertain pathogenesis, challenging etiological diagnosis and poorer prognosis for the primary. Krukenberg tumor is a metastatic signet ring cell adenocarcinoma of the ovary, accounting for 1% to 2% of all ovarian tumors. Stomach is the primary site in most Krukenberg tumors (70%). Carcinomas of colon, appendix, and breast (mainly invasive lobular carcinoma) are the next most common primary sites [2]. Although, ovarian metastasis is frequently seen in connection with breast cancer, the Krukenberg tumor of breast origin is a rare condition. In a study by Gagnon et al., 64 (38%) of 165 cases of ovarian metastasis were found to stem from breast cancer &none had features of Krukenberg tumor
[7]. In a review by Yada-Hashimoto et al., 64 cases of ovarian metastasis were evaluated, 11 cases of Krukenberg tumor were found of which 8 cases originated in the stomach & none originated in breast [3]. In a comprehensive review of the literature by Kiyokawaet al., only 6% of 530 Krukenberg tumors were of breast origin [8]. Apart from the rarity of Krukenberg tumor from breast primary, our case had the further complication of being associated with pregnancy because pregnancy and lactational changes can present a diagnostic challenge to the cytological interpretation of breast aspirates.
The development of ovarian metastasis during the course of any type of cancer is a negative prognostic factor. Most patients die within 1 year of diagnosis of ovarian metastasis. It was reported that the 5-year survival rate after resection of metastatic ovarian tumors from gynecological and non-gynecological organs were 47 and 19%, respectively, which is a significant difference [3].
Conclusion
The metastatic ovarian carcinoma of Krukenberg represents an advanced terminal phase of a neoplastic disease. Stomach is the primary site in most Krukenberg tumors with breast being an uncommon site. There are only very few reported cases of Krukenberg tumor in pregnancy. Our case of a primiparous young female having bilateral breast carcinoma with ovarian metastasis (B/L) is very rare. This rarity prompted us to report it.
Abbreviations
B/L: Bilateral; ER: Estrogen receptor; FNA: Fine needle aspiration; HER-2/neu: Human epidermal; IHC: Immunohistochemistry; PAS: Periodic acid Schiff; POD: Pouch of Douglas; PR: Progesterone receptor
Authors' Contribution
TS: Concept and design, literature search and preparation of manuscript.
ESR: Concept and design, literature search and preparation of manuscript.
BRMR: Concept and design, preparation review and editing of the manuscript.
RVK: Concept and design, preparation review and editing of the manuscript.
All authors read and approved the manuscript.
Conflict of Interests
The authors declare that there are no conflicts of interests
Ethical Considerations
Written informed consent was obtained from patient for publication of this case report. Copy of the consent is available with authors.
Funding
None declared
Acknowledgements
None
References
[1].Lerwill MF, Young RH. Metastatic Tumors of the Ovary. In: KurmanRJ, editor. Blaustein’s pathology of female genital tract, 6th ed. New York: Springer; 2011: 949-60.
[2].Al-Agha OM, Nicastri AD. An in-depth look at Krukenberg tumor: an overview. Arch Pathol Lab Med. 2006 Nov;130(11):1725-30. [PMID 17076540]
[3].Yada-Hashimoto N, Yamamoto T, Kamiura S, Seino H, Ohira H, Sawai K, Kimura T, Saji F. Metastatic ovarian tumors: a review of 64 cases. GynecolOncol 2003;89:314-317
[Pubmed]
[4].KwonHY, NamE, KimSW,KimYT. A young patient in Korea with Krukenberg tumors arising from breast cancer: A case report. Korean J ObstetGynecol 2011;54(10):643-646.http://www.ogscience.org/Synapse/Data/PDFData/2021KJOG/kjog-54-643.pdf
[5].Dueñas-García OF1, Diaz-Sotomayor M, Chanana C. Bilateral ovarian krukenberg tumor in a full-term pregnancy. ISRN Obstet Gynecol. 2011; 2011:620380. doi: 10.5402/2011/620380. Epub 2010 Oct 28. [PMID: 21637363].[Pubmed]
[6].KrukenbergF. “Uber das fibrosarcomaovariimucocellulase (carcinomatoses),” Archives of Gynecology Obstetrics1896; 50: 287–321.
[7].Gagnon Y, Tetu B. Ovarian metastases of breast carcinoma. A clinicopathologic study of 59 cases. Cancer 1989; 64: 892–98
[Pubmed]
[8].Kiyokawa T, Young RH, Scully RE. Krukenberg tumors of the ovary: a clinicopathologic analysis of 120 cases with emphasis on their variable pathologic manifestations. Am J SurgPathol 2006;30: 277–99.[Pubmed]

