Case Report

Multinodular Pulmonary Amyloidosis: a Rare and Challenging Diagnosis
(*)Mona Mlika , (*) Emna Braham,
(*)Linda BelHadjKacem, (*) FaouziMezni ,
- (*)Department of Pathology. AbderrahmanMami Hospital. Ariana
- Submitted: January 15, 2015
- Accepted: February 17, 2015
- Published: February 22, 2015
This is an Open Access article distributed under the terms of
the Creative Commons Attribution License
(http://creativecommons.org/licenses/by/3.0) which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited
Abstract
Background
Pulmonary amyloidosis is a very rare form of localized amyloidosis. Microscopic examination plays a key role in the diagnosis because of the non specificity of clinical and radiological findings. Even PET scan is not helpful to make the diagnosis.
Observation
We present the case of a 66-year-old man with a smoking history and an occupational exposure to dust. He presented with asymptomatic multiple pulmonary masses evoking the diagnosis of pulmonary metastasis. Surgical resection was performed and microscopic examination confirmed the diagnosis of multinodular amyloidosis.
Conclusion
This case highlights the fact that pulmonary amyloidosis may cause multiple nodules.
Introduction
Amyloidosis is due to the depositof a complex protein, which has the ability to form beta-pleated sheet. Amyloidosis can involve the lung as a local or part of a systemic disease
[1]. We report a case of multinodular pulmonary amyloidosis in order to highlight the key-role played by the microscopic examination.
Case Presentation
A 66-year-old patientpresented in March 2014 an asymptomatic mediastinal mass discovered incidentally. He had 10 years of smoking history of one pack/day. His past medical history was consistent for occupational exposure to dust and a hydatid cyst of the liver resected in 2000.
There was no clubbing. Bronchial endoscopy was normal. Chest X-ray showed a right para-cardiac mass (Figure
1A). The CT-scan showed bilateral pulmonary nodules and micronodules with the largest one measuring 12 mm
(Figure 1B).
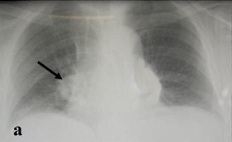
Figure 1(A): Chest-x-ray showing a right para-cardiac mass (arrow),

Figure 1(B): CT-scan showing bilateral pulmonary nodules and micronodules with the largest one measuring 12 mm.
After 6 months, a second CT-scan was performed and showed a suspect nodule of the inferior left lobe which didn’t increase in size but presented irregular margins. A cerebral scan was performed and was normal. A peripheral blood count baseline serum chemistry screening and urinalysis were normal on admission, as were tumor biomarker tests and a purified protein derivative test for tuberculosis. Surgical resection was performed and consisted in a wedge resection including the left inferior nodule. Extemporaneous exam was performed and concluded to an eosinophilic material corresponding probably to an amyloid deposit. Definitive examination showed an amorphous acellulareosinophilic material. Under polarized light microscopy, Congo-red stained material showed the characteristic apple green birefringence of amyloid material (Figure 2a, b). To investigate the possibility of primary systemic amyloidosis, urine and serum protein electrophoresis were performed without evidence of monoclonal protein. Bone marrow biopsy was performed without evidence of clonal plasma cell and amyloid deposit.The diagnosis of multinodular pulmonary amyloidosis was retained. The patient was discharged without complications. He showed no signs of local recurrence or distal disease at two-month follow-up visit.
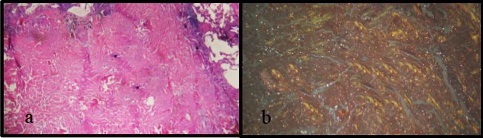
Figure 2: (a)Microscopic examination showing a pulmonary parenchyma with an amorphous acellulareosinophilic material (HEx400).
(b) Under polarized light microscopy, Congo-red stained material showed the characteristic apple green birefringence of amyloid material (HEx400).
Discussion
In this case, we report a rare form of multinodular pulmonary
amyloidosis. Formerly grouped by etiology (primary versus secondary), it is now
classified as either systemic or limited. Systemic disease typically is seen in
patients suffering from chronic inflammation, myeloma or tuberculosis and may
affect multiple organs expected the brain and is less apt to involve the lungs.
The respiratory tract is commonly affected in localized disease [2].
Pulmonary amyloidosis is very rare with 4 major types of involvement:
tracheobronchial form (local or diffuse) and 2 parenchymal forms including
nodular and alveolar septal parenchymal involvement. Rare forms of
tracheobronchial forms have been described [1]. Parenchymal
involvement was described in association to WG [3], plasmocytoma, myeloma, epithelioid hemangioendothelioma
[3 4 5 6 and 7].
Patients are typically asymptomatic; however, a solitary nodule is a more common
finding than multiple nodules. Such nodules were reported in association with
lymphoma or Sjogren’s syndrome [8 9]. On CT scan, pulmonary nodules have sharp and lobulated margins and are found in sub-pleural or peripheral location, more frequently in the lower lobes. Size may vary from micro-nodules to 15 cm in diameter [6 9].
Over time, nodules may grow slowly, cavitate, calcify or resolve spontaneously [9 10].
Calcifications are observed in 20 to 50% of nodules on CT images [6].
In our case, nodules were bilateral and the suspected nodule was located in the
left lung. During follow up, the nodules haven’t increased in size but the
irregular margins of 1 nodule made its microscopic exploration mandatory. In our
case, metastatic disease or primary lung cancer has to be ruled out. Besides,
because of the professional exposure of our patient to dust, the possibility of
pneumoconiosis had to be excluded. Positron emission tomography (PET)-scan may
be helpful when showing non fluorodeoxyglucose-avid nodule, however, negative
results would not necessary secure the diagnosis and PET-scans are costly [2].
CT-guided percutaneous lung biopsy or trans-bronchial biopsy is helpful to make
the diagnosis and many authors reported their efficiency to make the diagnosis [11].
In our case, the need to surgical resection was justified by the thought of the
clinicians that the nodule was malignant. Characteristic microscopic features of
amyloid deposit consist in an amorphous acellular eosinophilic material with an
apple green birefringence under polarized light microscopy. This birefringence
isn’t observed in case of pneumoconiosis and helps to rule out the diagnosis. By
consensus, asymptomatic patients with the diagnosis of pulmonary amyloidosis
performed on trans-thoracic biopsy or surgical biopsy may not require surgical
intervention. Periodic follow-up with careful monitoring may be sufficient. For
symptomatic patients, carbon dioxide laser ablation or surgery may be used [12].
The prognosis of pulmonary amyloidosis is generally poor with a median survival
time of diffuse parenchymal amyloidosis less than 2 years [13 14]
but nodule amyloidosis carries the most favorite prognosis and long-term
survival is expected even without treatment [9].
Authors' Contribution
MM carried out the literature search and prepared the draft manuscript, MM and EB interpreted the results, HZ, LBK and FM participated in design and edited the final manuscript. All authors read and approved the final manuscript for submission.
Conflict of Interests
The authors declare that there are no conflicts of interests.
Ethical Considerations
Written informed consent was obtained from patient for
publication of this case report
Funding
None declared
Acknowledgement
None
References
[1]Raiyani PD, Vyas SS. Tracheobronchial amyloidosis-a series of two cases.J ClinDiagn Res. 2014; 8(9):FD09-10. [Pubmed]
[2]Liu M, Wei S, Li X, Liu H, Zhou Q, Chen J1. Pulmonary nodular amyloidosis in a patient undergoing lobectomy: a case report.J Med Case Rep. 2013; 7:248
[Pubmed]
[3]Ishiguro T1, Takayanagi N, Katoh N, Shimizu Y, Hoshi T, Yanagisawa T, Sugita Y. Waldenström'sMacroglobulinemia Accompanying Systemic Amyloidosis: The Usefulness of Endobronchial Ultrasound-guided Transbronchial Needle Aspiration for Detecting Amyloid Deposits.Intern Med. 2014; 53(24):2789-93.
[4]Piard F, Yaziji N, Jarry O, et al. Solitary plasmacytoma of the lung with light chain extracellular deposits: a case report and review of the literature. Histopathology. 1998; 32:356-61. [Pubmed]
[5]- Morinaga S, Watanabe H, Gemma A, et al. Plasmacytoma of the lung associated with nodular deposits of immunoglobulin. Am J SurgPathol. 1987; 11:989-95. [Pubmed]
[6].Higo H1, Fujiwara K, Watanabe H, Makimoto G, Kameyama N, Matsushita M, Rai K, Sato K, Inomata T, Sunami K, Shibayama T. Diffuse parenchymal pulmonary amyloidosis showing an objective response to bortezomib-based chemotherapy.Intern Med. 2014; 53(16):1809-12 [Pubmed]
[7].Cheng D, Shi H, Zhang K, Liao Y, Zhen G. Pulmonaryepithelioidhemangioendotheliomacoexisting with pulmonary nodular amyloidosis: case discussion and review of the literature.Int J ClinExp Med. 2014 15; 7(7):1891-7. [Pubmed]
[8]Zhang LN1, Xue XY, Wang N, Wang JX. Mimicking pulmonary multiple metastatic tumors: A case of primary nodular parenchymal pulmonary amyloidosis with review of the literature.OncolLett. 2012; 4(6):1366-1370.[Pubmed]
[9].Chew KM, Clarke MJ, Dubey N, Seet JE. Nodular pulmonary amyloidosis with unusual, widespread lung cysts.Singapore Med J. 2013; 54(5):e97-9 [Pubmed]
[10].OzerSimsek Z1, Oymak FS, Tutar N, Canoz O, Demir R. A Rare Cause of Diffuse Parenchymal Lung Disease together with Granulomatous Reaction: Pulmonary Amyloidosis.Case Rep Pulmonol. 2013; 2013:837190.[Pubmed]
[11].Kitamura H, Kobayashi T, Kaneko M, Kusumoto M, Kodama T, Matsuno Y,Niki T: Pulmonary amyloidosis diagnosed by CT-guided transbronchial biopsy: a case report. Jpn J ClinOncol2001, 31:209–211.[Pubmed]
[12].Nugent AM, Elliott H, McGuigan JA, Varghese G: Pulmonary amyloidosis: treatment with laser therapy and systemic steroids. Respir Med 1996, 90:433–435 [Pubmed]
[13].Utz JP, Swensen SJ, Gertz MA. Pulmonary amyloidosis: the Mayo Clinic experience from 1980-1993. Ann Intern Med 124: 407-413, 1996.[Pubmed]

