
Giant Cells in Giant Cell Reparative Granuloma: Physiognomic or Pathognomic Relevance?
*Bacem AE Ottoman,
- *Maxillofacial Surgery and Diagnosis, Ministry of Health, Cairo, Egypt
- Submitted: Tuesday, May 19, 2015
- Accepted: Thursday, July 02, 2015
- Published: Tuesday, July 07, 2015
This is an Open Access article distributed under the terms of the Creative Commons Attribution License ((http://creativecommons.org/licenses/by/3.0)which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited
Abstract
Giant cell reparative granuloma is a tumor-like lesion, which is characterized by the typical appearance of dotted granulation tissue. Such dotting is attained by the giant cell populations. Histogenesis and pathogenesis of such multinucleated giant cells are, hitherto, controversial. Some attributed the origin of multinucleated giant cells to an osteoclastic lineage from differentiated mononuclear cells. This paper, however, suggests another origin with a newly introduced mechanism of action.
Introduction
For so many years, the nature of giant cell lesions of oral cavity has been controversial. Some substantial histological, immunohistological, ultrastructural and enzymatic studies have been carried out to determine the origin and role of multinucleated giant cells (MGCs) in giant cell granulomas. Yet, the exact mechanism and nature are, statically, idiopathic [1]. Some investigators believed that MGCs emanate from phagocytic, foreign body MGC, or osteoclastic lineage [2-4]. Other studies considered myofibrolastic [5] an endothelial cell origin [6]. Moreover, some investigations suggested that giant cells were formed by fusion and adhesion of stromal mononuclear cells with an unknown mechanism [7].
In the same vein, Odell et al., [8] have suggested a fibroblastic origin of the giant cell, due to the vimentin positivity which was observed in his study, analogous to the positive reactivity of vimentin in giant cell glioblastoma [9]. Desmin has shown, however, a negative reactivity for giant cells; eliminating the prospect of a myofibroblastic origin, in a single case [10]. Moreover, positivity of benign giant cells for CD68, in pathognomic giant cell tumors was reported [11].
Material and Method
Besides the systematic review of literature, twelve archival cases of reparative granulomas were histologically contrasted to ten cases of normal mucosa. All were stained with three mesenchymal immunohistochemical markers: CD34 (1:200, citrate 30 min, Dako) vimentin (D33, 1:600, citrate 30 min, Dako), and desmin (V9, 1:200, citrate 30 min, Dako).
From the block of the represented case, serial sections from formalin-fixed, paraffin-embedded specimen block of 4 μm thickness were deparaffinized in xylene and rehydrated in decreasing concentrations of ethanol. Endogenous peroxidase activity was blocked by immersing the sections in 3% H2O2 with methanol for 30 minutes. For antigen retrieval, sections were boiled in 10 mmol/L citrate buffer (pH 6.0) for fifteen minutes in a pressure cooker. After treatment with protein block serum at room temperature, sections were covered with primary antibodies. Immunoreaction was performed using the labeled streptavidin-biotin method and overnight incubation. For all antibodies, negativity or positivity was evaluated.
Results
Reparative giant cell granulomas (RGCGs) typically appear as red to blue, broad-based masses. Secondary ulceration caused by trauma may result in the formation of a fibrin clot over the ulcer (Figure 1a). RGCGs mostly exceed 1 cm in diameter, and hit any age with a female predilection. All submitted cases were treated via conservative surgical excision, with no evidence of recurrence for 18 months (Figure 1b). Histologically a confluence of multinucleated giant cells in a granulation tissue was remarkable. Metaplastic bone and chronic inflammatory cells were present (Figure 2).

Figure 1: (a) A clinical picture of a reparative giant cell granuloma before excision

Figure 1(b) the same case 2 week after excision.
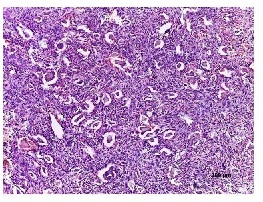
Figure 2: Photomicrograph showing reparative giant cell granuloma whose fibroblastic matrix and abundant multinucleated giant cells are obvious. (H&E stained, Original magnifications: 40x, 100x)
All case of normal mucosa, on the one hand, showed no giant cell population. They were negative for any significant expression of CD34, vimentin, or desmin. On the other hand, all submitted cases showed strong positive immunoreaction for vimentin (Figure.3, 4& 5) and positive, but weaker, immunoreaction for desmin.(Figure.6 & 7)
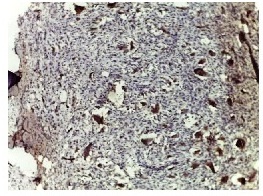
Figure 3: photomicrograph showing positive vimentin expression by multinucleated giant cells (Original magnifications: 10x).
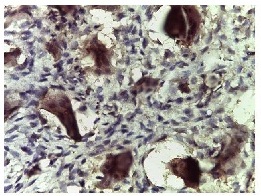
Figure 4: photomicrographs showing positive vimentin expression by multinucleated giant cells (Original magnifications: 40x).
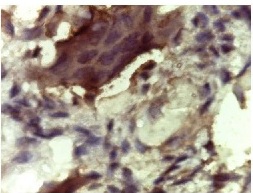
Figure 5: Photomicrograph showing positive vimentin expression by multinucleated giant cells (original magnifications: 100x).
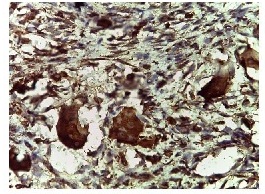
Figure 6: photomicrograph showing desmin positivity by multinucleated giant cells (original magnifications: 40x).
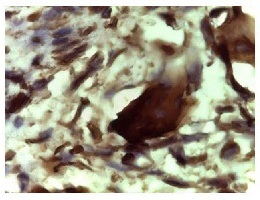
Figure 7: photomicrograph showing desmin positivity by multinucleated giant cells (original magnifications: 100x).
Discussion
Reparative giant cell granuloma (RGCG), either peripheral or central, is a relatively uncommon and unusual hyperplastic connective tissue response to injury of gingival tissues. It is one of the “reactive hyperplasia” commonly seen in oral mucous membranes, representing an exuberant reparative process in association with local trauma, or irritation. The hallmark that typifies this lesion is the appearance of multinucleated giant cells, but the reason for their presence remains idiopathic [12].
Injury of the connective tissue stimulates parenchymal and stromal cells to undergo desmoplastic changes. Given the multiple components of the connective tissue, an exuberant reparative response is characterized by larger stromal cells with increased extracellular fibers by transformation of fibroblastic-type cells to a myofibroblastic phenotype. Irritation and injury of CT induce a remarkable proliferation of fibroblasts with subsequent secretion of collagen. The newly secreted collagen acts as a scaffold for infiltration of cells to the site of injury. Moreover, some degradation occurs providing some space for new vasculature to start an angiogenesis [13].
Given the considerable confusion which surrounded giant cell lesions and giant cell tumors, cytogenetic studies in giant cell tumors (GCT) reveal telomeric associations (TAS) as the most frequent chromosomal aberration [14]. Some GCTs show rearrangements in 16q22 or17p13, similar to aneurysmal bone cyst, which is often associated with GCT [15], unlike the X-chromosome and chromosome 4 [t(X;4)(q22;q31.3)] cytogenetic findings in central reparative giant cell granulomas.
ligament or periosteum, and they sporadically induce alveolar bone resorption. Peripheral giant cell granulomas typically appear as red to blue, broad-based masses. Secondary ulceration caused by trauma may result in the formation of a fibrin clot over the ulcer. These lesions, most of which are about 1 cm in diameter, may occur at any age and tend to show a female predilection (1.5-2:1) [16]. RGCGs are usually located in the mandible more than the maxilla [17]. Molar and pre-molar areas are more often encountered than the anterior parts, or the ascending ramus. On removal, RGCGs, peripheral or central, are highly vascular [18].
Although some RGCGs are expansive and invasive, they do not usually involve perineural sheets [19]. Despite some cases in literature of metastatic giant cell tumors where have been reported [20], it should be emphasized that giant cell tumor and brown tumor of hyperparathyroidism are way different from RGCG. Their giant cell populations are neoplastic with typical features of malignancy, unlike RGCG. Accordingly, histological scrutinizing and determination of parathormone levels may be indicated, especially in elderly patients or when multifocal lesions are evident [12].
Histologically, scattered throughout the fibroblasts are abundant multinucleated giant cells, which appear to be nonfunctional in the usual sense of phagocytosis and bone resorption. Islands of metaplastic bone occasionally may be seen in these lesions. Chronic inflammatory cells are present, and neutrophils are found in ulcer bases. Microscopically, a peripheral giant cell granuloma is identical to its central or intraosseous counterpart, the central giant cell granuloma [12].
For the sister lesion, the so-called pyogenic granuloma, the remodeling of resynthesized collagen, was blamed for adding up to the swollen nature in order to accommodate the stromal changes [21]. In a similar vein, this study suggests that the MGCs, which were positive for vimentin, belong to the fibroblastic-type cells. Moreover, a myofibroblastic phenotype is suggested owing to the positive immunoreactivity with desmin. All supports the physiognomic presence of such MGCs, which induce no conspicuous damage to the surrounding structures. Ultrastructurally, El-labban [10] has supported the presence of myofibroblast in RGCG . This finding , which was upported by the current positive immunoreactivity, was denied by Mighell
et al., [10]. Given that Mighell
et al., [10] have reported a solitary case with a negative expresion for desmin, this appears to relate to either an isolated case or unrepresentative stained section. The stained section , had it had been representative, could have been passively affected by improper preparation or retrieval. For not underestimating the valuability of that reported case, further studies are recommended to quash a claim and field a strong side.
Surgery is the most accepted and traditional form of treatment. However, tissue removal ranges from simple curettage to bloc resection [22]. Nonsurgical approaches to avoid disfigurement have been also used, including daily systemic doses of calcitonin and intralesional injection with corticosteroids. Some giant cell granulomas can be sterilized thermally using laser or cryoprobe [23]. More recently, antiangiogenic therapy with interferon alpha has been successfully applied [24].
Conclusion
This study suggests that the MGCs, which were positive for vimentin, belong to the fibroblastic-type cells. Moreover, a myofibroblastic phenotype is suggested owing to the positive immunoreactivity with desmin. The physiognomic presence of such MGCs, which induce no conspicuous damage to the surrounding structures, is highly suggested.
This should prompt new speculations about the claims of malignant transformation of such self-reparative lesion. Moreover, it accounts for the high clinical vascularity of such lesion since the newly secreted collagen acts as a scaffold for infiltration of cells with some degradation which should provide some space for new vasculature to start a remarkable angiogenesis.
Authors’ Contribution
The author conducted the study, prepared and edited the manuscript and approved for publication.
Conflict of Interests
The author declares that there is no conflict of interest.
Ethical Considerations
The authors declare that the study was approved by the Institute Ethics committee and consent was obtained from the patients.
Funding
None
References
[1].Liu B, Yu SF, Li TJ. Multinucleated giant cells in various forms of giant cell containing lesions of the jaws express features of osteoclasts. J Oral Pathol Med. 2003;32:367–75 [Pubmed]
[2].Hlleen JM, Tiitinen SL, Ylipahkala H, Fagerlund KM, Vaananen HK. Tartrate-resistant acid phosphatase 5b (TRACP 5b) as a marker of bone resorption. Clin Lab. 2006;52:499–509 [Pubmed]
[3].Bonetti F, Pelosi G, Martignoni G, Mombello A, Zamboni G, Pea M, et al. Peripheral giant cell granuloma: Evidence for osteoclastic differentiation. Oral Surg Oral Med Oral Pathol. 1990;70:471–5 [Pubmed]
[4].Flanagan AM, Nui B, Tinkler SM, Horton MA, Williams DM, Chambers TJ. The multinucleate cells in giant cell granulomas of the jaw are osteoclasts. Cancer. 1988;62:1139–45 [Pubmed]
[5]El-labban NG, Lee KW. Myofibroblast in central giant cell granuloma of the jaws: An ultrastuctural study. Histopathology. 1983;7:907–18 [Pubmed]
[6].Thompson SH, Bischoff P, Bender S: Central giant cell granuloma of the mandible. J Oral Maxillofac Surg. 1983;41:743–6 [Pubmed]
[7].Adkins KF, Martinez MG, Robison LH: Cellular morphology and relationships in giant-cell lesions of the jaws. Oral Surg Oral Med Oral Pathol. 1969;28:216–22 [Pubmed]
[8].Odell EW, Lock C, Lombardi T: Phenotypic characterisation of stellate and giant cells in giant cell fibroma by immunocytochemistry. Journal of Oral Pathol Med. 1994;23:284–7.[Pubmed]
[9].Miller DC. Modern surgical neuropathology. Cambridge: Cambridge University Press; 2009.
[10].Mighell AJ, Robinson PA, Hume WJ: PCNA and Ki-67 immunoreactivity in multinucleated cells of giant cell fibroma and peripheral giant cell granuloma. J Oral Pathol Med. 1996;25:193–9 [Pubmed]
[11].Chu PG, Weiss LM. Modern immunohistochemistry. New York, NY: Cambridge University Press; 2009.
[12].Regezi J, Sciubba J, Jordan R: Oral Pathology. Clinical Pathologic Correlations, Saunders, Philadelphia, Pa, USA, 5th edition, 2007.
[13].Ross M, Pawlina W: Histology: A Text and Atlas: With Correlated Cell and Molecular Biology. Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins Health, 201:158-78.
[14].Bridge JA, Neff JR, Bhatia PS, Sanger WG, Murphey MD (1990). Cytogenetic find- ings and biologic behavior of giant cell tumors of bone. Cancer 65: 2697-703 [Pubmed]
[15.Fletcher CDM, Unni K, Mertens F . WHO Classification of Tumours. Pathology and Genetics of Tumours of Soft Tissue and Bone. IARC Press: Lyon. 2002
[16].Kaffe I, Ardekian L, Taicher S, Littner MM, Buchner A (1996). Radiologic features of central giant cell granuloma of the jaws. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 81: 720-726.[Pubmed]
[17].Whitaker SB, Waldron CA. Central giant cell lesions of the jaws. A clinical, radiologic, and histopathologic study. Oral Surg Oral Med Oral Pathol 1993;75: 199-208.[Pubmed]
[18].tavropoulos F, Katz J . Central giant cell granulomas: a systematic review of the radiographic characteristics with the addition of 20 new cases. Dentomaxillofac Radiol 2002; 31: 213-7.
[19].Fechner RE, Stacey EM, editors. Atlas of Tumor Pathology: Tumors of bones and joints. Armed Forces Institute of Pathology. 1993:181–2
[20].Small GS, Rowe NH: A true giant cell tumor in the mandible. J Oral Surg. 1975;33:296–301 [Pubmed]
[21].Al-shiaty R, Ottoman B: Recurrent pyogenic granuloma: an update. Int J Sci Rep, 2015; 1(1), 22-31.
[Full text]
[22].Bataineh AB, Al-Khateeb T, Rawashdeh MA. The surgical treatment of central giant cell granuloma of the mandible. J Oral Maxillofac Surg. 2002;60:756–61 [Pubmed]
[23].Whitaker SB, Waldron CA. Central giant cell lesions of the jaws: A clinical, radiologic and histopathologic study. Oral Surg Oral Med Oral Pathol. 1993;75:199–208.[Pubmed]
[24].Kaban LB, Troulis MJ, Ebb D, August M, Hornicek FJ, Dodson TB . Antiangiogenic therapy with interferon alpha for giant cell lesions of the jaws. J Oral Maxillofac Surg 2002; 60: 1103-11.[Pubmed]

