Case Report

Cytodiagnosis of Sinonasal Aspergillosis - A Case Report with Brief Review of Literature
*Dhiraj B Nikumbh, *Shivraj N Kanthikar, *Sneha S Desale, *Rajeshwari K,
- *Department of Pathology, JMF’s ACPM Medical College, Dhule, Maharashtra, India.
- Submitted: Monday, May 18, 2015
- Accepted: Tuesday, June 23, 2015
- Published: Wednesday, July 22, 2015
This is an Open Access article distributed under the terms of
the Creative Commons Attribution License
(http://creativecommons.org/licenses/by/3.0) which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited
Abstract
Background
Aspergillosis of head and neck region primarily affect nose and paranasal sinuses. Mycotic infections are raising globally both in immunocompetent and immunocompromised individuals. These infections mimic malignancy clinically and radiologically. They pose a diagnostic and therapeutic challenge to the physician. In such cases, aspiration cytology plays a crucial role in early and definitive diagnosis of mycotic infections.
Case Presentation
We herein present a case of 75-year-old male presented to the surgical department of our hospital with right maxillary region swelling with a discharging sinus since 2 months. Clinically suspected as sebaceous cyst/malignancy. Fine needle aspiration cytology (FNAC) was advised and showed giant cell lesion with fungal hyphae, morphologically suggestive of
Aspergillosis.
Conclusions
Early diagnosis with aspiration cytology will help the clinician for prompt and appropriate management and follow up in order to reduce the morbidity and mortality associated with its destructive nature. The goal of this case report was to highlight the importance of FNAC in diagnosing subcutaneous mycotic infections promptly and to avoid further complications of the disease.
Key words
Aspiration cytology, aspergillosis, mycotic infections.
Introduction
Fungal sinonasal sinusitis constitutes 6-9% of all the rhinosinusitis [1, 2]. Fungal infections of the sinonasal areas are increasingly recognised entity in immunocompetent and immunocompromised individuals [3]. Aspergillosis and Mucormycosis being commonest of all the fungal infections involving maxillary sinus manifests as two different entities, a non-invasive and an invasive infection respectively. These lesions presents a diagnostic and therapeutic challenge to the physician as they mimics malignancy clinically and radiologically [4].
Hence it is important to distinguish the invasive and non invasive fungal infections as the treatment and prognosis are different in each. Early diagnosis by cytological examination is always essential in order to avoid high morbidity and mortality associated with the destructive diseases [3].
Herein, we discuss a case of 75-year-old male presented to the surgical OPD with right maxillary region swelling with discharging sinus since 1 month. Fine needle aspiration cytology morphology was suggestive of
Aspergillosis. The culture and the histopathological examination were advised to the patient.
Cytology is the reliable, safe, simple and quick technique for diagnosis of aspergillosis. Preoperative cytodiagnosis obviates the need of diagnostic biopsy, allow rapid diagnosis to plan the proper management as culture take time. In this case report, we highlight the role of fine needle aspiration cytology in such lesions.
Case Report
A 75-year-old-male presented to the surgical department of our hospital with chief complains of right maxillary painful swelling since 2 months. The swelling has gradually increased to the present size and with serous discharge. There was history of recurrent nasal obstruction and recurrent rhinitis. On local examination, the tender swelling in the right maxillary region was noted measuring 3x2 cms with sinus opening (Figure 1).

Figure 1 - Gross appearance of swelling over right maxillary region with discharging sinus.
There was no history of diabetes, hypertension or tuberculosis to the patient and also in the family. Haematological, biochemistry, serological and urinary analysis were within normal limits. X-ray of the maxillary region showed soft tissue lesion with no bone involvements. Clinical differential diagnosis was sebaceous cyst or malignancy. Fine needle aspiration cytology of right maxillary region was advised. Fine needle aspiration cytology was performed with 22 gauge needle attached to the 10cc syringe mounted on Comeco’s handle under all aseptic precautions. The gross aspirate was haemorrhagic with greyish whitish material. Air dried and wet fixed smear were prepared and stained with Leishman stain and pap stain respectively. Microscopic picture of fine needle aspiration cytology showed predominantly clusters and sheets of histiocytes with multinucleated giant cells and epithelioid cell clusterson a hemorregic background (Figure 2). The cytoplasm of multinucleated giant cells and histiocytes showed branching septate hyphae of fungus-morphology suggestive of aspergillosis (Figure 3).
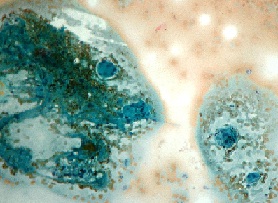
Figure 2- Cytology showed clusters and sheets of histiocytes with multinucleated giant cells and epithelioid cell clusters (Pap stain, x100).

Figure 3-The cytoplasm of multinucleated giant cells and histiocytes showed branched septate hyphae of fungus-morphology suggestive of aspergillosis (Pap stain, x400).
Many fruiting bodies and conidia were also evident inside the giant cells. Many multinucleated giant cells with intracytoplasmic negative staining hyphae were evident (Figure 4). The hyphae was thin septate and branched at acute angles. With above cytological features, morphology was suggestive of aspergillosis. The final diagnosis of sinonasal region aspergillosis was rendered and further culture and histopathological examination study were advised to the patient. The patient was prescribed oral antifungal drugs and ointments.
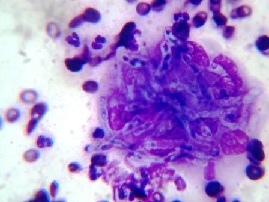
Figure 4–Microphotograph showing multi-nucleated giant cells with intracytoplasmic negative staining hyphae of aspergillus (Leishman stain x400).
Discussion
Aspergillosis belongs to the category of systemic mycosis. Though not seen in immunocompetent individual, there is an increased incidence in immunocompromised patients over the past two decades. Fungal sinusitis constitutes 6-9% of all the rhinosinusitis [1, 2]. Clinically it present as an acute fulminant sinusitis or chronic invasive sinusitis [3].
Aspergillus species are ubiquitous, commonly found in the soil and decaying vegetation. The spores are typically inhaled or ingested without any consequence in the normal host and exposure to this fungus is frequent. However, disease due to tissue invasion is uncommon in the immunocompetent host [5]. The modes of entry of aspergillus include the respiratory tract, damaged skin or operated wounds, cornea and ear [6].
Aspergillosis of head and neck region primarily affects the nasal cavity and paranasal sinuses [7]. It is seen in warm and dry climatic conditions with young men from rural background in north India [8]. Aspergillus as a pathogen cannot actively penetrate the undamaged and intact mucus areas or skin as it lacks keratolytic enzymes. On the basis of this finding, paranasal sinus
aspergillosis is now classified into invasive (acute fulminant, chronic invasive and granulomatous invasive) and non-invasive (allergic rhinosinusitis and fungal ball) forms with their pathophysiology and clinical presentation [9]. Any type of sinonasal aspergillosis may progress to more aggressive disease. Hence the importance of early recognition of this increasingly encountered disease is always warranted by FNAC [7].
In our case, the patient was immunocompetent presented with sinonasal mass and cytomorphologically diagnosis was suggestive of aspergillosis, probably non-invasive-allergic rhinosinusitis.
Clinically these patients presents with rhinorrhoea, headache, nasal obstruction, proptosis, facial and periorbitalpain mimicking infections, inflammatory lesion and malignant tumour of the nose and paranasal sinuses. In our case, the patient presented with recurrent rhinitis and sinonasal swelling without any symptom of invasive disease.
Imaging modalities such as X-ray, MRI and CT can help to establish a diagnosis of invasive fungal sinusitis. However they are not definitive and often fail to differentiate an infectious from a neoplastic one [10]. Fungal culture is complementary to morphology and required for species identification, but samples submitted for the cultures may not be representative, and not all the cultures grow on the media, hence cytomorphology remains the mainstay of diagnosis in most of the cases [10]. Sinonasal swelling when present are easily amenable to FNAC. Adequate and representative cytological material when obtained can reliably give a confident diagnosis [10].
Regarding differential diagnosis, aspergillosis can be easily differentiated from mucor on morphology, as the latter is characterised by broad non-septate hyphae with branching at right angles.
Aspergillus shows filamentous structure with a diameter of 3-6 micron and with septate hyphae with branching at acute angles [10]. Due to the presence of many foreign body giant cells, other differentials include the giant cells rich lesions such as tuberculosis, leprosy, rhinoscleroma, actinomycosis, rhinosporidiosis, sarcoidosis and Wegner granulomatosis to giant cell reperative granuloma, giant cell tumour, Langharhan’s cell histiocytosis and anuerysmal bone cyst [4]. Cytologically and on subsequent biopsy we can easily differentiate above diagnosis.
In our case, cytomorphological finding were suggestive of aspergillosis. Fine needle aspiration cytology provides specific fungal diagnosis when fungal profiles are identified. Special stain such as PAS and GMS may be helpful to find fungal hyphae.
FNAC provides the reliable generic diagnosis of inflammation and inflammatory infiltrate with foreign body giant cells with or without necrosis. Fungi may be seen intracellular or extracellulary [4]. Demonstration of inflammatory reaction determines that the organism represent the infection and not the contamination [4].
In our case, the patient was old age, immunocompetent with clinical suspicion of cyst/ malignancy, however, the diagnosis on fine needle aspiration cytology as aspergillosis (allergic, non-invasive fungal infection). FNAC prevents undue surgery in our case.
Species identification is of importance in case of aspergillosis, in view of
Aspergillus flavus is the commonest type reported in India [10]. Unfortunately culture and histopathological examination may not be performed in our case, in view of lost the follow up of patient after the medical treatment which was given after cytodiagnosis.
Conclusions
The goal of this case report is to emphasize on the early diagnosis of subcutaneous and sinonasal fungal infections which can be managed conservatively, preventing morbidity and mortality in these patients. Fungal infection with subcutaneous mass closely mimics malignancy on clinical examination. Cytology being an easily available procedure can be used as initial diagnostic modality in subcutaneous and sinonasal fungal infections. It obviates the need of diagnostic biopsy; allow rapid diagnosis as culture takes time. Early diagnosis by fine needle aspiration cytology is mandatory to prevent undue surgery.
Authors’ Contribution
DBN: Concept and design, preparation review and final editing of the manuscript.
SNK: Concept and design, literature search and draft of manuscript.
SSD: Concept and design, literature search and preparation of manuscript.
RK: Concept and design, preparation review and editing of the manuscript.
Conflict of Interest
The authors declare that there are no conflicts of interest.
Ethical Considerations
Written informed consent was taken from patient for publication of this case report.
Funding
None declared
References
[1]Schubert MS. Allergic fungal siunusitis: Pathophysiology,diagnosis and management.Med Mycol.2009;47(supp.):S324-30 [Pubmed]
[2].Parikh SL, Venkatraman G, DelGaudio JM.Invasive fungal sinusitis:A 15 year review from a single institution. Am J Rhinol.2004; 18:75-81 [Pubmed]
[3]Taneja T,Saxena S,Aggrawal P,Reddy V.Fungal infection involving maxillary sinus a difficultdiagnostic task. JClinical Exp Dent.2011; 3(2):e172-6.http://www.medicinaoral.com/odo/volumenes/v3i2/jcedv3i2p172.pdf
[4]Singhal N, Raghubanshi G, Handa U, Punia RP, Singhal S.Fine needle aspiration cytology: A useful technique for diagnosis of invasive fungal rhinosinusitis. Head and Neck Pathology.2013; 7:236-40.[Pubmed]
[5]Furgue TH Jr, Sittitavornwong S, Kroll M,Said-Al-HaiefN.Primary invasive oral
aspergillosis: An updated literature review. J Oral Maxillofacial Surg.2010; 68:2557-63 [Pubmed]
[6]Sivak-Callcott JA, Livesley N, Nugent RA, Rasmussen SL, Saeed P, Rootman J. Localised invasive sino-orbital
aspergillosis: Characteristic feature. Br J Ophthalmol. 2004 May;88(5):681-7. [Pubmed]
[7]Rowe-Jones J.Paranasal aspergillosis - a spectrum of disease. J Laryngol Otol. 1993 Sep;107(9):773-4 [Pubmed]
[8]ChakrabartiA, Sharma SC.Paranasal sinus mycoses. Indian J Chest Dis Allied Sci. 2000 Oct-Dec;42(4):293-304 [Pubmed]
[9]Lin SJ, Schranz J, TeutschSM..Aspergillosis- Case fatality rate: Systemic review of literature. Clin Infect Dis. 2001 Feb 1; 32(3):358-66. Epub 2001 Jan 26. [Pubmed]
[10].Kumar Behera S,Patro M, Mishra D,Bal A, Behera B, Sahoo S. Fine needle aspiration cytology in aspergilloma of frontal sinus: A case report. ActaCytol.2008; 52:500-04 [Pubmed]

