Case Report

Melanotic Neuroectodermal Tumour of Infancy - A Case Report of a Rapidly Enlarging Maxillary Mass
1Olugbemi B Akintububo 2Olufemi K Ogundipe2Olujide O Soyele3Umaru H Pindiga3Yusuf M Abdullahi
- 1Department of Oral and Maxillofacial Surgery, Federal Teaching Hospital, Gombe, Nigeria
- 2Departmen of Oral Maxillofacial Surgery and Oral Pathology, OAU Ife, Nigeria
- 3Department of Pathology, Federal Teaching Hospital, Gombe, Nigeria.
- Submitted: Tuesday, October 18 2016
- Accepted: Thursday, November 24, 2016
- Published: Tuesday, December 27, 2016
This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/3.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited
Abstract
Introduction
The melanotic neuroectodermal tumor of infancy (MNTI) is a rare benign neoplasm that primarily affects the maxilla of infants during their first year of life. It is a rapidly growing lesion, clinically aggressive and surgery is the mainstay of treatment with proven efficacy.
Case Presentation
A case of maxillary MNTI in a 5-month-old male infant treated by radical surgery is reported here. Both extraoral and intraoral findings showed a massive swelling with multiple ulcerations of the overlying mucoas. Radiographs showed an ill defined mixed radiolucent radiopaque lesion. Histopathological examination showed biphasic microscopical presentation consisting of aggregates of small neuroblastic cells surrounded by the larger pigmented cells.
Conclusions
MNTI is a rare, rapidly progressive pigmented lesion that commonly affects the anterior maxilla. Other differentials should be carefully considered in arriving at a diagnosis. Wide surgical excision with margin of normal tissue is the mainstay of treatment.
Key Words
Melanotic neuroectodermal tumor of infancy, Surgery
Introduction
Melanotic neuroectodermal tumour of infancy (MNTI) is a rare connective tissue neoplasm of neural crest origin, comprising pigment producing large polygonal cells and small neuroblastic cells [1- 5].
The origin of MNTI is uncertain, it is believed to arise from the retinal anlage, odontogenic origin, melanocarcinoma from epithelial rests or Jacobson vomeronasal organ [1 - 5]. Since the time MNTI was first reported in 1918, five major systematic reviews of English literature have identified more than 476 cases with no clear gender predilection [1 - 5]. It predominantly occurs in infants, involving the craniofacial site specifically the premaxilla/maxilla area although other sites have been reported [2, 3]. Cases involving the mandible and skull have been reported [4, 5].
It is characterized by rapid growth, bluish-black discoloration, displacement of the involved tooth buds, and high recurrence rate with a propensity for malignant transformation [1 - 5]. MNTI could pose diagnostic and treatment challenges to clinicians. Complete surgical excision is generally considered as the primary treatment option [6], but protocols combining local surgery and adjuvant chemotherapy have also been proposed for recurrent tumours [7,8]. The severe adverse effects associated with chemotherapy in young children remain a matter of debate. A recent investigation showed BRAFV600E mutation in a case of MNTI, which might give rise to the use of targeted therapy in the management of MNTI [10].
The purpose of this report is to present a case of MNTI in a five-month-old boy who was treated by complete surgical excision. The clinical, imaging, and histological characteristics of this case are also discussed. To the best of our knowledge, no previous Nigerian case has been documented.
Case Report
A five-month-old boy was referred to the Oral and Maxillofacial Surgery Department of Federal Teaching Hospital, Gombe, Nigeria, with a 5- month history of upper left jaw swelling. The swelling, noticed at birth was painless, rapidly increasing in size with associated difficulty in feeding and weight loss. There was no associated epistaxis or spontaneous bleeding from the lesion. He otherwise appeared healthy with remarkable medical or family history. On extra-oral examination, the baby was emaciated with grossly enlarged mass of the left maxilla with extension out of the mouth. The swelling measured 8cm by 6cm in diameter, oval, firm, non-tender, with blackish colouration of the overlying mucosa. The nose was deviated to the right side (Figure 1). Extra-oral plain radiographs revealed ill defined mixed radiolucent radiopaque presentation.

Figure 1: Clinical photograph showing intraoral tumor
Intra- oral examinations revealed a large expansile mass with well demarcated margins. There are multiple areas of ulceration of the alveolar mucosa labially and palatally. The two mandibular central incisors were the only teeth present. Excisional biopsy under general anesthesia was decided upon based on the age of the patient and the size of the lesion. The patient was worked up for surgery. The tumour was surgically excised with wide margin of normal tissue via bucco-gingival incision. Local buccal flap was used for closure of the defect. Grossly the tumor appeared pigmented (Figure 2). Microscopically, lesion consisted of small neuroblastic cells and larger polygonal cells which were pigmented with melanin granules. The small neuroblastic cells were arranged in nest surrounded by the larger pigmented cells (Figure 3 & 4) His postoperative recovery was uneventful (Figure 5) and patient was considered fit to go home a week later. The patient was subsequently lost to follow-up.

Figure 2: Resected specimen
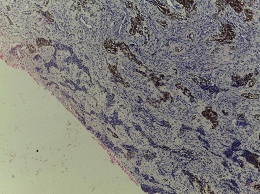
Figure 3: Photomicrograph showing tumor composed of small neuroblastic cells
and larger polygonal cells (H & E x40)
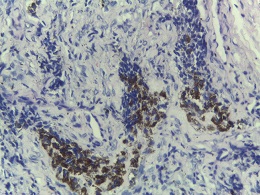
Figure 4: Photomicrograph showing tumor cells laden with intracellular
melanin. The small neuroblastic cells were arranged in nest surrounded by the
larger pigmented cells

Figure 5: Postoperative photograph showing recovery.
Discussion
MNTI is a rare tumor; we report the first Nigerian case in a 5-month old infant. Camevale et al., [9] earlier reported a case in West Africa. The clinical presentation of a rapidly enlarging nonulcerative pseudoencapsulated and solitary discolored maxillary mass in an infant is highly suggestive of MNTI as majority of cases previously reported have similar presentations. The peak age of occurrence has been reported to be 4 months [2]. Clinical differential diagnosis of a rapidly enlarging mass of the upper jaw includes rhabdomyosarcoma (RMS), Ewing family of tumours (EFT) and Burkitt lymphoma (BL) were considered but were excluded based on clinical and histologic grounds.
African endemic BL may present with other abdominal symptoms which were absent in this present case. Also, BL is not known to present with this typical discoloration. Histologically, BL does not present with a biphasic cellular pattern of small neuroblastic cells and large polygonal melanin producing cells. The typical morphologic starry-sky appearance in dense lymphoid cells caused by tingible body macrophages seen in BL was not present in our case. Phenotypically and genetically, BL should be positive for CD45 (leucocyte common antigen) and isolated MYC/8q24 rearrangement.[11].
RMS is also not known to present with this typical discoloration. Histologically, the morphologic presentation of RMS depends on the particular subtype: alveolar, embryonal, spindle-sclerosing and pleomorphic. RMS should be positive for desmin phenotypically [11].
EFT, when it presents in the jaw does not present with discoloration. Histologically, the morphologic presentation of EFT is that of small round blue cells. EFT is positive for CD99 and EWSR1 rearrangement[11]. In MNTI, the small neuroblastic cells are positive for neuroendocrine markers such as Chromogranin, synaptophysin, and neuron-specific enolase. The large polygonal cells which are usually pigmented with granules of melanin pigment are positive for Human melanoma black-45 and cytokeratin [11]. Furthermore, patients with MNTI, although not all, show positivity to urinary3-methoxy 4-hydromandelic acid (VMA) [2].
Computerized tomography (CT) scan and magnetic resonance imaging (MRI) are of benefit in preoperative assessment and treatment planning. However, only extraoral plain radiographs were used in this case because the patient could not afford the cost of these advanced imaging techniques. This is a common challenge seen in the management of this tumour in a resource poor setting.
Treatment is by wide surgical excision although recurrences have been reported usually within the first few months of surgery. Since the patient did not return after surgical excision, we could not ascertain the possibility of recurrence. Long term follow up is mandatory because the course of the disease cannot be predicted by morphological findings alone. However, the age at presentation is an important prognostic predictive marker of recurrence with younger patients more likely to develop such [12]. Previous studies have reported positive results following surgical treatment [7,8]. Wide surgical excision with margin of normal tissue provides the best efficacy for local tumour clearance and cure [13]. Radiotherapy and chemotherapy have been found to be ineffective in the treatment of MNTI [2].
Conclusions
MNTI is a rare, rapidly progressive pigmented lesion that commonly affects the anterior maxilla. Other differentials should be carefully considered in arriving at a diagnosis. Wide surgical excision with margin of normal tissue is the mainstay of treatment.
Conflict of interest
The authors declare that there are no conflicts of interests
Authors’ contribution
AOB was responsible for conception, design, data acquisition, drafting/revision of the article and final approval.
OOK was responsible for design, data acquisition/analysis/interpretation, drafting/revision of the article and final approval.
SOO made substantial contribution to design, drafting/revision of the article and final approval.
PUH made substantial contribution to design, drafting/revision of the article and final approval.
AYM made substantial contribution to design, drafting/revision of the article and final approval.
Ethical consideration
The written informed consent was taken from the next of kin of the patient and is available with the authors.
Funding source
None
References
-
Rustagi A, Roychoudhury A, Karak AK. Melanotic neuroectodermal tumour of infancy of the maxilla: a case report with review of literature. L Oral Maxillofac Surg 2011:69(4):1120-1124
[Pubmed]
-
Rachidi S, Sood AJ, Patel KG, Nguyen SA, Hamilton H, Neville BW, Day TA. Melanotic Neuroectodermal Tumor of Infancy: A Systematic Review. J Oral Maxillofac Surg. 2015 Oct;73(10):1946-56. doi: 10.1016/j.joms.2015.03.061. Epub 2015 Apr 7. PMID: 25936939
[Pubmed]
-
Cutler LS, Chaudhry AP, Topazian R. Melanotic neuroectodermal tumour of infancy: an ultrastructural study, literature review, and reevaluation. Cancer. 1981;48(2):257-70
[Pubmed]
-
Mosby EL, Lowe MW, Cobb CM, Ennis RL. Melanotic neuroectodermal tumor of infancy: review of the literature and report of a case. J Oral Maxillofac Surg. 1992 Aug;50(8):886-94. PMID: 1321897
[Pubmed]
-
Kruse-Lösler B, Gaertner C, Bürger H, Seper L, Joos U, Kleinheinz J. Melanotic neuroectodermal tumor of infancy: systematic review of the literature and presentation of a case. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006 Aug;102(2):204-16. Epub 2006 Jun 8. PMID: 16876064
[Pubmed]
-
Piperi EP, Rake SA, Tosios KI, Vasilopoulou EE, Rake AP, Sandler NA, Issacson T, Sklavounou A, Koutlas IG. Mandibular melanotic neuroectodermal tumor of infancy treated conservatively with enucleation. J Craniofac Surg. 2010 May;21(3):685-8. doi: 10.1097/SCS.0b013e3181d7f0c5. PMID: 20485029
[Pubmed]
-
Maroun C, Khalifeh I, Alam E, Akl PA, Saab R, Moukarbel RV. Mandibular melanotic neuroectodermal tumour of infancy: a role for neoadvuvant chemotherapy. Eur Arch Otorhinolaryngol. 2016 Dec;273(12):4629-4635. Epub 2016 Apr 23
[Pubmed]
-
Kumari TP, Venugopal M, Mathews A, Kusumakumary P. Effectiveness of chemotherapy in melanotic neurectodermal tumor of infancy. Pediatr Hematol Oncol. 2005 Apr-May;22(3):199-206
[Pubmed]
-
Camevale GG, Mortelliti AJ. The operating microscope in the management of melanotic neuroectodermal tumour of infancy. Am J Otolaryngol. 2001, 22: 76-79
[Pubmed]
-
Gomes CC, Diniz MG, Menezes GH, Castro WH and Gomez RS. BRAFV600E Mutation in Melanotic Neuroectodermal Tumour of Infancy: Toward Personalized Medicine? Pediatrics.2015; 136(1):e267-269.
[Pubmed]
-
Owosho AA, Ko E, Rosenberg HI, Yom SK, Antonescu CR, Huryn JM and Estilo CL. Primary Ewing Family of Tumors of the Jaw Has a Better Prognosis Compared to Tumors of Extragnathic Sites. J Oral Maxillofac Surg. 2016.74:973-981.[Pubmed]
-
Yoo IH, Yum SK, Oh SJ, Kim MK and Jeong CD. Melanotic neuroectodermal tumour of infancy disseminated by a ventriculoperitoneal shunt and diagnosed from the inguinal sac. J Pediatr Hematol Oncol 2014. 36: e61-64.[Pubmed]
-
Rasmane B, Zakari N, Sa T, Pierre B. Maxillarty Melanotic Neuroectodermal Tumour of Infancy Management: Is Conservative Surgery the Best Approach? J Craniofac Surg. 2013 Jul;24(4):e338-40. doi: 10.1097/SCS.0b013e31828a7c4c
[Pubmed]

