Research

Acellular Collagen Matrix versus Autologous Breast Reconstruction:
Patient-reported Outcome.
*, Lay In Lim, ** Amar Deshpande
- * Core Surgical Trainee, West Midlands, UK
- ** Consultant Breast Surgeon Wrightington Wigan and Leigh NHS Foundation Trust, Wigan, UK
- Submitted Saturday, June 28, 2014
- Accepted:Thursday, September 04, 2014
- Published Sunday, September 07, 2014
This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/3.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited
Abstract
Background: Acellular collagenl matrix (ACM) is getting more popular and well established in recent years in breast reconstruction where it is used to achieve implant cover and produce a better outcome. There are different types of tissue matrix which are made from different materials such as porcine dermis (Strattice tm), foetal bovine dermis (Surgimend tm), etc. Another well-known method of breast reconstruction is using autologous tissue such as Lattisimus Dorsi flap or Transverse Rectus Abdominis Myocutaneous flap.
Aims
We are looking into the outcome of breast reconstruction using ACM versus breast reconstruction with autologous tissue. The outcomes include patient satisfaction, post¬operative psychosocial, sexual and physical well-being, complications after breast reconstruction, information given and evaluation from patients on surgeons and medical team's care towards patients.
Methods
This study is carried out as a retrospective study on a single institution. Patients who have had breast reconstruction using ACM and autologous tissue were randomly identified from the electronic patient records from year 2009 to 2013. Questionnaires were posted to patients and data were analysed. Breast Q questionnaire was used for this study.
Breast Qª is a validated and copyrighted questionnaire designed for researchers to assess a patient's perspective before and after their breast reconstruction. The Breast Qª scoring system was used to analyse our data. Each cohort received 18 responses, therefore the total sample size is 36 patients.
Results
On average, patients have scored more than 60 out of 100 on all the aspects except on sexual well-being where the mean score for patients who has had ACM was 49 and for the patients who had autologous reconstruction was 59. Patients with ACM scored slightly higher score as compared to patients with autologous reconstruction in terms of physical well-being, satisfaction with surgeons and overall care whereas patients with autologous reconstruction scored slightly higher scores as compared to patients with ACM in terms of satisfaction with breasts, outcomes, psychosocial well-being, social well-being and satisfaction with information. In the result analysis, we also looked into median for each categories and used Mann Whitney U test as our statistical analysis. The value for U statistic was 21. For 5% two-tailed level, critical value of U is 13. As calculated U> U critical, and the p value is 0.247996, we accept the null hypothesis that the two groups of data are not different.
Conclusions
There was no significant difference in terms of outcomes in between the 2 groups of patients. Through this study, it is suggested that breast reconstructions using both ACM and autologous tissue are safe to be used and both are satisfactory to the patients.
Background
Acellular collagenl matrix (ACM) is a soft tissue matrix graft created by a process that results in decellularization. This process will leave the extracellular matrix intact. This matrix is said to act as a platform where the patients own cell can populate and revascularise the implanted tissue [1]. ACM has been used since 2001 in breast surgery. The use of ACM in breast reconstructions was first reported by Breuing and Warren in year 2005 [2]. The authors had selectively chosen 10 women who underwent bilateral mastectomy using this technique.
ACM is getting more popular and well established in recent years in breast reconstruction where it is used to achieve implant cover and produce a better outcome [3]. There are different types of tissue matrix which are made from different material such as porcine dermis (Strattice tm), foetal bovine dermis (Surgimend tm) etc.
ACM helps to optimize aesthetic results (figure 1)
(figure 2), control the implant position by providing a strong support and cover and help in defining the inframammary and lateral mammary folds in order to create a more natural-looking breast. It may help mask the palpability of the implant in addition to other added benefits [4].
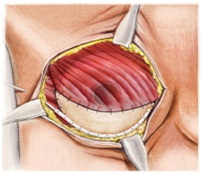
Figure 1: Laterally, ACM is directly secured to serratus to create lateral portion of mammary fold. Disinserted pectoralis major is secured inferiorly to ACM and laterally to serratus to provide complete coverage of tissue expander or implant.
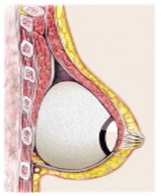
Figure 2: Lateral view (Pictures adopted from Medscape (1a)
autologous parts; leading to reduced operation and recovery time and lesser morbidity. However, these types of products are fairly new to the market. The use of ACM in breast reconstructive surgery is well described in the North American literature however it is a relatively new technique in the UK [5]. We are still in the phase of establishing the definite benefit of using ACM therefore more research needs to be done to prove and validate that it is worth using these types of materials for breast reconstruction bearing in mind the cost of the acellular collagen matrix before using it in a large volume.
In recent years, due to the popularity of usage of ACM, L Martin et al., had produced a guideline with participation of the association of breast surgery and the British association of plastic, reconstruction and aesthetic surgeons. Recommendations were produced after reviewing the current published data for using ACM as part of breast reconstruction. One of the areas that the authors looked into was to derive indications for ACM assisted breast reconstruction [5]. Clinical indications for ACM include sufficient skin envelope, planned immediate breast reconstruction procedure after discussion at the MDT meeting, as a potential alternative to 2 stage breast reconstructions using expander and implant based reconstruction, estimated mastectomy weight of less than 600grams ;this is because it has been reported that breast sizes>600 grams are associated with higher infection rate
[5]. Relative indications and cautions were discussed in the article as well [5].
According to Zhong T et al where the team did a multi-centre
Canadian randomised controlled trial to evaluate the impact on patient
satisfaction and quality of life using the Breast Q questionnaire comparing
ADM-facilitated one stage implant reconstruction to two- stage tissue expander /
implant reconstruction, it was suggested that there was a huge interest in using
ADM assisted implant reconstruction due to the unique benefit of having surgery
through one stage instead of going through two stages [6]. However, this
technique needs to be evaluated further scientifically before it is promoted as
the gold standard in implant-based breast reconstruction [6].
Goyal et al., carried out a study assessing safety, efficacy, patient satisfaction and also the complications after dermal sling-assisted breast reconstruction. In their study, they have selected 21 patients who underwent 28 dermal sling assisted breast reconstruction procedures. It was found that dermal sling for breast reconstruction has a low serious complication rate, providing stable tissue cover and has high patient satisfaction [7].
While there is a wide spread use of ACM, Reitsamer R et al., had conducted a research to look into the technical result and complication rates after mastectomy and immediate implant based reconstruction using ACM [8]. In this study the sample size was 27 cases of skin-sparing or nipple-sparing mastectomy with immediate implant based reconstruction using ACM for implant coverage. The complications include skin breakdown with implant loss in 7.4%, secondary haemorrhage in 3.7%, complete nipple necrosis in 3.7%, minimal nipple necrosis in14.8% and inflammation requiring antibiotics in 3.7% [8]. It was concluded through this study that using ADM such as strattice is an innovative approach resulting in an excellent cosmetic result, it is also technically feasible and the complication rates are low [8].
Alternative method of breast reconstruction is using autologous tissue such as lattisiumus dorsi flap, transverse rectus adbominus myocutaneous flap , deep inferior epigastric perforator flap, superior gluteal artery perforator flap, superficial inferior epifascial artery flap and so on.
The LD flap was initially described in 1906 by Iginio Tansini [9], subsequently in 1976 it was reinforced by Olivari [10] . Mühlbauer and Olbrich utilised and applied this LD flap in breast reconstruction [11]. Holmström reconstructed breasts in 1979 using the free TRAM flap [12]. Both LD flap and TRAM flap has good blood supply from the donor sites.
LD flap obtained the blood supply from thoracodorsal artery which is the terminal branch of the subscapular artery. It also received a secondary blood supply which arises from segmental perforating branches off of the lumbar and intercostal arteries [13]. TRAM flap has dual blood supply as well which are superior and inferior epigastric arteries. However for the operation using TRAM flap, it relies only on the inferior epigastric arterial system [14]
In our institute, most of the surgeons utilise either Lattisimus Dorsi (LD) flap or Transverse Rectus Abdominus Myocutaneous (TRAM) flap. Use of autologous tissue such as (LD) flap and (TRAM) in breast reconstruction accounts for a flexible and more natural looking breast after reconstruction. There are risks associated in using autologous tissue for breast reconstruction such as seroma, flap necrosis, back pain for LD flap and abdominal shaped distortion for TRAM flap.
Fakhry H. et al carried out a study to look into the results and complications of autologous LD flap for breast reconstruction. In this study, 40 patients underwent breast reconstruction using LD flap were assessed. The complications were partial flap necrosis in 10%, wound breakdown in 5%, lymphorrhea in 5%, seroma in 15 %. It was concluded through this study that LD flap breast reconstruction is a versatile, safe and satisfactory technique with a success rate of over 99 % and it is also applicable to the high risks patients [15]. In this study, it was proven that seroma is the most common complication which can be dealt with in the clinic by aspiration [15].
Lattisimus Dorsi(LD) flap reconstruction is a good option for patients who had failure with breast conservation therapy(BCT): lumpectomy and postoperative radiation. According to Freeman M. E. et al who had conducted a study to look into the outcomes of 12 patients who underwent LD flap reconstruction after the development of recurrent breast cancer after BCT. [16]. Despite prior radiation, it is shown that LD flap is still a good options for breast reconstruction. It was also discovered that all of the patients had a satisfactory aesthetic result, therefore LD flap remains a good option for breast reconstruction after failure of BCT. [16]. In this study, they have the similar finding as compared to the finding from Fakhry et al.’s study in terms of post- operative complication which is seroma. However the sample size used by Freeman M. E. et al is relatively small, therefore larger sample size would have been more valuable in data interpretation.
Aims
Aim of this study was to assess the outcome of breast reconstruction using ACM, produces an outcome which is as good as using autologous tissue in breast reconstruction form the patients’ perspective. The outcomes include patient satisfaction, post-operative psychosocial , sexual and physical well-being, complications after breast reconstruction, information given and evaluation from patients on surgeons and medical team’s care towards patients. We also aim to highlight any technical problems encountered using the ACM. The authors are reviewing the cumulative experience with this technique.
Patients and Methods
This is a retrospective study and the samples were selected randomly from a single institution. Patients who have had breast reconstruction using ACM and autologous tissue were identified from the electronic patient records and also theatre lists from year 2009 to 2013.
Questionnaires were posted to patients and postage paid envelops were enclosed with the for the patients to send back the questionnaire to us.
We used Breast Q questionnaire for this study [17
18]. Breast Q is a validated and copyrighted questionnaire designed for researchers to assess a patients perspective before and after their breast reconstruction [19]. Breast Q has several different modules and we used the reconstruction module (post-operative) 1.0 version. We have gained permission and obtained a license to use this questionnaire for our research purposes.
Besides that we have liaised with the local hospital patient and public engagement department and went through the legal procedure to get permission to get in touch with the patients prior to sending out of the questionnaires to the patients.
We produced 2 separate cover letters as shown in Figure.1,2, in appendices and sent to these 2 groups of patients. Group 1 patients are the patients who have had breast reconstructions using ACM + implant, whereas Group 2 are the patients who had autologous tissue +/- implant as breast reconstruction method.
Breast Q
There are 3 separate domains in interpretation of Breast Q result. The first domain is quality of life, the second domain is satisfactions and the third one is expectations domain [21]
In quality of life domains, it is subdivided into psychosocial wellbeing, sexual well-being and physical well-being. In satisfaction domains, it is split up into satisfaction with breast, satisfaction with nipple, satisfaction with abdomen, satisfaction with outcome and satisfaction with care. The last domain is expectations domain which includes expectations for support from medical staff, expectations for pain, expectations for recovery, expectations for coping, expectations for breast appearance &outcome, expectations for psychosocial well-being and expectations for sexual well-being [21].
The breast reconstruction module consists of 13 questions.
Each question is subdivided to many other questions as shown in appendices.
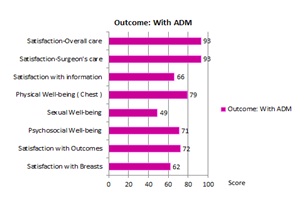
Figure 3: Mean scores for each domain
In the questionnaire, questions 1 and 2 are asking about satisfaction with breast, question 3 is asking about satisfaction with outcome which means the womans overall appraisal of the outcome of the breast surgery. Question 4 covers psychosocial well-being. Question 5 asks about sexual well-being. Questions 6, 7, 8, 9 and 10 cover physical well-being. Question 11 is about satisfaction with information, question 12 is about patients satisfaction with surgeons care and question 13 is about patients satisfaction with overall care.
Each question has numbers ranging from 1 to 5. Data collected from patient need to be key in into an excel sheet, after key in all the data, the data is then exported to Q score programme where Q score software will convert the data to numbers ranging from 0 to 100 which is similar to conversion into a percentage. The sum of the scores is then calculated to produce a mean score. A higher score means high satisfaction or better health related quality of life [21]. The lower score indicates the opposite.
Appendices are the example of the structure of the Breast Q for breast reconstruction module. (Courtesy Memorial Sloan-Kettering Cancer and the University of British Columbia who hold the copyright of the BREAST-Q) Copyright © 2012 Memorial Sloan Kettering Cancer Center.
Results
Overall the questionnaire return rate was 67%. In the patient Group 1 the return rate was 64%, whereas for Group 2 the response rate was 69%. Each cohort received 18 responses; therefore the total sample size is 36 patients.
The mean age for patients in Group 1 was 52, ranging from 28 to 67 years of age whereas the mean age for patients in Group 2 was 53, ranging from 32 to 68 years of age. The mean ages for these 2 groups are very similar. All the women had breast reconstruction following breast cancer surgery.
In Group 1, there was 62% for satisfaction with breast, 72% for satisfaction with outcomes, 71% for psychosocial well-being, 49% for sexual well-being, 79% for physical well-being, 66% for satisfaction with the information, 93% for satisfaction with surgeon’s care, 93% for satisfaction for overall care.
In group 2, on average, there was 74% for satisfaction with breast, 83% for satisfaction with outcomes, 77% for psychosocial well-being, 59% for sexual well-being, 72% for physical well-being, 75% for satisfaction with the information, 88% for satisfaction with surgeon’s care, 90% for satisfaction for overall care.
In summary, as shown in [Figure.3, 4, 5]on average patients have scored more than 60 out of 100 on all the aspects except on sexual well-being where the mean score for patients in Group 1 was 49 and Group 2 was 59. Patients in Group 1 scored slightly higher score as compared to patients in Group 2 in terms of physical well-being on chest, satisfaction with surgeons and overall care whereas patients in Group 2 scored slightly higher scores as compared to patients in Group 1 in terms of satisfaction with breasts, outcomes, psychosocial well-being, social well-being and satisfaction with information. In our study , our null hypothesis is there is no difference in breast reconstrauction outcome in terms of patient satisfaction btween patient using ADM versus patient using autologous tissue.
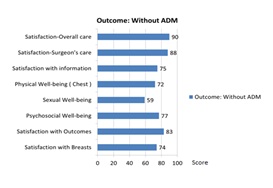
Figure 4: Mean scores for each domain
Figure 5: Mean scores for 2 groups
In the result analysis, we also looked into the median manually without the software for each categories as shown in [Figure 6] in order to use Mann Whitney U test as our statistical analysis. After analysing, the value for U statistic was 21. For 5% two-tailed level, critical value of U is 13. As calculated U> U critical, and the p value is 0.247996, we accept the null hypothesis that the two groups of data are not different.
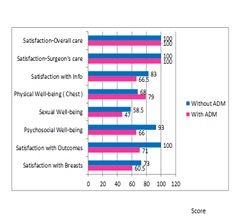
Figure 6: Median scores for 2 groups
Discussion
Our result shows that there are similarities as compared to studies carried out by other authors. For example, In May 2013, Elgammal S et al., published about patient reported outcomes in immediate breast reconstruction [22]. Validated patient questionnaire were used which covered cosmetic, emotional and functional outcomes. The sample size is 158 patients who responded to the survey. For the question how natural the breast looked unclothed â€which is a sensitive marker, 83% of woman who had LD flap as breast reconstruction had high satisfaction (excellent/ very good), 82% for DIEP flap, 82% of women underwent ADM assisted breast reconstruction reported high satisfaction. However, 39% of patients who has had tissue expander as part of breast reconstruction rated poorly for satisfaction. It was concluded that in breast reconstruction, the ADM compares more closely to autologous tissue in terms of patient perceptions of cosmesis, and scores considerably better than implant based with tissue expander [22].
Another study was conducted by Theodorakopoulou E et al., where breast QTM Questionnaire was used to determine the patient satisfaction following oncoplastic breast surgery. Responses were analysed using breast QTM scoring software which is the same as our study method [23]. The study assessed the perceived success of breast cancer surgery using the patients own views. Overall satisfaction with surgical outcome is closely related to patients physical and psychoemotional well-being after the operations [23].
There are a few similar studies to date. However, because ADM is a fairly new product to the surgical field, carrying out more research and surveys will help to compare with the existing studies and will be fruitful for future research references
The centre is very keen to establish the evidence that is worth using ADM for breast reconstruction and the patient satisfaction to this procedure is high.
A review of the current English literature was carried out using Cochrane, Embase, Medline and Pubmed databases with a few key words such as Breast Q, acellular dermal matrix, autologous tissue, lattisimus dorsi flap, transverse rectus abdominus myocutaneous flap, breast cancer and breast reconstruction.
We narrowed down the number of papers by selecting the papers that have similar topics to our study and review the results of the papers. Through the literature review, most of the papers suggest that ACM and autologous tissue generate high patients satisfactions.
EltharY et al., carried out a cross sectional study on quality-of-life outcomes between mastectomy alone and breast reconstruction using breast Q. The total patients in mastectomy plus breast reconstruction were 92 patients, whereas there were 45 patients for mastectomy alone. The authors used multiple regression analysis to evaluate the statistical significance in this study. It was suggested that women with successful breast reconstruction were significantly more satisfied with different aspects of the patients life compared to women who do not undergo reconstructive surgery [24]
Seroma is one of the most common complications following mastectomy and breast reconstruction. We reviewed a research which was conducted by Tong RT et al., on clinical outcomes of percutaneous drainage of breast fluid collections after mastectomy with expander-based breast reconstruction. It was found that 28 patients (5%) developed seroma which led to 30 imaging guided percutaneous drainage procedures. It was established that percutaneous drainage is an effective means of treating postoperative seroma [25]. Another issue that we should consider is the cost of the different types of breast reconstruction. In patients who had breast implants and ACM, the cost of the prosthesis is higher whereas in patients who have had autologous tissue as part of the breast reconstruction the duration of the operating time is longer and therefore the cost of theatre time, surgeons and staff time need to be taken into consideration.
Johnson RK et al conducted a study to analyze the cost of using ACM for breast reconstruction as compared to standard alternative techniques which are tissue expander/implant as a 2 stage procedure and LD flap breast reconstruction. Clinical report such as operative time, length of stay, outpatient procedures and number of admissions were collected. The cost analysis shows that there is a financial advantage in using ACM in unilateral breast reconstruction as compared to the alternative techniques [26]. Bilateral breast reconstruction using ACM is more expensive than conventional bilateral breast reconstruction.
Breast reconstruction using ACM is technically more demanding as there is a learning curve. Besides that, specific post-operative care is needed in the form of leaving the drains in-situ for up to 2 weeks; depending upon the amount of fluid draining. Patients also need to go home with 2 weeks of antibiotics with early and frequent reviews.
Limitations
A larger sample size and multi-centred study will definitely be beneficial towards reinforcing the findings of this study. In view of small sample size, our study might have type 2 error by accepting the null hypothesis because the power of the study is low.
Summary
From our study, we discovered that there was no significant difference in terms of outcomes in between the 2 groups of patients. ADM is comparable to autologous tissue in breast reconstruction context. This finding coincides with the finding of Elgammal S et al’s study where they have concluded that ADM compares closely with flap based reconstruction in terms of patient perception of cosmesis [22]. Through this study, it is suggested that ADM is safe to be used and patients satisfaction is good. In the patient cohort with ADM, breast implant was used whereas in patient cohort without ADM, autologous tissue (such as Lattisimus Dorsi flap or Transverse Rectus Abdominis Myocutaneous flap) +/-implants were used for breast reconstruction. ADM is a suitable material to be used when the patients do not have suitable autologous tissue to be used for breast reconstruction.
Conclusions
There was no significant difference in terms of outcomes in between the 2 groups of patients. Through this study, it is suggested that ACM is safe to be used and patients satisfaction is good.
Authors Contributions
LIL: Compiling and analysing the data, writing the manuscript
AD: Original idea and provision of the data, checking and editing the manuscript
Ethical Considerations
The study was approved by the Institute Ethics committee.
Conflict of Interests
We thank the authors who produced Breast Q and allowing me to use their validated questionnaire for this study.
We would to express our gratitude to all the patients that responded to the questionnaire and had participated in this study.
References
[1]. Kim JYS. Breast Reconstruction with Acellular Dermis. Medscape Updated: Oct 3, 2013 http://emedicine.medscape.com/article/1851090-overview [Last accessed September 6, 2014].
[2]Breuing KH, Warren SM. Immediate bilateral breast reconstruction with implants and inferolateral AlloDerm slings. Ann Plast Surg. 2005; 55: 232-9.
[3]. Sbitany HH, Langstein N. Acellular dermal matrix in primary breast reconstruction. Aesthetic Surgery Journal 2011; 31(7 suppl): 30S-37S
[Pubmed]
[4] Strattice™ Reconstructive Tissue
Matrix http://www.kci-medical.co.uk/UK-ENG/strattice [Last Accessed on September
6, 2014].
[5] Martina L, O'Donoghue JM, Horganc K, Thrushd S, Johnsone R, Gandhie A. Acellular dermal matrix (ADM) assisted breast reconstruction procedures .Joint Guidelines from the Association of Breast Surgery and the British Association of Plastic, Reconstructive and Aesthetic Surgeons. http://www.bapras.org.uk/downloaddoc.asp?id=848 [Last accessed September 6, 2014].
[6] Zhong T. , Temple-Oberle C, Hofer S, Brett B., Semple J., Brown M., Macadam S., Lennox P., Panzarella T, McCarthy C, Baxter N, Butler C., Causarano N., Choi J., Webb C. The Multi Centre Canadian Acellular Dermal Matrix Trial ( MCCAT): Study protocol for a randomized controlled trial in implant-based breast reconstruction. Trials. 2013; 14: 356.Oct 28, 2013. doi: 10.1186/1745-6215-14-356
[7]. Goyal A,. Wu JM, Chandran VP,. Reed MWR. Outcome after autologous dermal sling-assisted immediate breast reconstruction. Br J Surg. 2011 Sep;98(9):1267-72. doi: 10.1002/bjs.7531. Epub 2011 May 10.[Pubmed]
[8]. Reitsamer R., Farmini A., Gschwandtner E., Fischer T. Technical results and complication rates after skin sparing and nipple-sparing mastectomy and immediate implant based reconstruction using a porcine tissue matrix Strattice® for implant coverage. Geburtshilfe Frauenheilkd April 2012; 72 - A21 DOI: 10.1055/s-0032-1309214
[9] Maxwell GP: Iginio Tansini and the origin of the latissimus dorsi musculocutaneous flap. Plast Reconstr Surg 1980, 65, 686–692
[Pubmed]
[10]. Olivari N: The latissimus flap. Br J Plast Surg 1976, 29, 126-128
[Pubmed]
[11]. Mühlbauer W, Olbrisch R: The
latissimus dorsi myocutaneous flap for breast reconstruction. Chirurgica
Plastica 1977, 4, 27.
[12] Holmstrom H. The free abdominoplasty flap and its use in breast reconstruction. An experimental study and clinical case report. Scand J Plast Reconstr Surg. 1979;13:423-427.
[Pubmed]
[13]. Stewart C Little, Arlen D Meyers. Latissimus Myocutaneous Flap . Nov 2013 http://emedicine.medscape.com/article/880878-overview#aw2aab6b3 [last accessed September 6, 2014]
[14] Michael R Zenn, James Neal Long Free TRAM Breast Reconstruction March 2014. http://emedicine.medscape.com/article/1273997-overview#a04 [last accessed September 6, 2014]
[15] Fakhry H, Hamza H, Ahmed B, Mostafa M, Amira G. Results and complications of autologous lattisimus dorsi flap breast reconstruction . European Journal of Cancer, 2012; 48: S211-S212.
[16] Freeman ME, Perdikis G, Sternberg EG, TerKonda SP, Waldorf JC. Latissimus dorsi reconstruction: a good option for patients with failed breast conservation therapy. Ann Plast Surg. 2006 Aug;57(2):134-7
[Pubmed]
[17] Pusic AL, Chen CM, Cano S, Klassen A, McCarthy C, Collins ED, Cordeiro PG. Measuring quality of life in cosmetic and reconstructive breast surgery: a systematic review of patientreported outcomes instruments. Plast Reconstr Surg. 2007; 120(4):823-37
[18] Pusic AL, Cano S, Klassen AF. Measuring Quality of Life in Breast Surgery: Content Development of a New Modular System to Capture Patient-Reported Outcomes (The MSKCC Breast-Q). ISOQOL Annual Meeting, October 2006, Lisbon, Portugal. http://www.proqolid.org/instruments/breast_q_breast_q
[Pubmed]
[19] Pusic AL, Chen CM, Cano S, Klassen A, McCarthy C, Collins ED, Cordeiro PG. Measuringquality of life in cosmetic and reconstructive breast surgery: a systematic review of patient reported outcomes instruments. Plast Reconstr Surg. 2007 Sep 15;120(4):823-37. Breast-q_useragreement_11.0_feb2013_protected (1).doc © MAPI Research Trust, December 1994. The unauthorized modification and use of any portion of this document is prohibited.
[Pubmed]
[20] RUMMFor analysing assessment and attitude questionnaire data. http://www.rummlab.com.au/ [Last accessed September 6, 2014]
[21] Breast Q™ users manual version 1.0 July 2012. https://webcore.mskcc.org/breastq/qscore/qscore-manual.pdf [Last accessed September 6, 2014]
[22]. Elgammal S, Brindle R, Johnson R. Patient reported outcomes in immediate breast reconstruction : Acellulr dermal matrix is more comparable to autologous rather than implant based reconstruction. Eur J Surg Oncol 2013; 39:518 [Full text]. http://dx.doi.org/10.1016/j.ejso.2013.01.017
[23] Theodorakopoulou E, Rattay T, Krupa J. P86. Patient satisfaction following reconstructive and oncoplastic breast surgery.Eur J Surg Oncol 2012; 38: 1129 [Meeting Abstract]
[24] Eltahir Y, Werners LL, Dreise MM, van Emmichoven I A, Jansen L, Werker PM, de Bock GH. Quality-of-life outcomes between mastectomy alone and breast reconstruction :comparison of patient-reported BREAST-Q and other health-related quality-of-life measures. Plast Reconstr Surg. 2013; 132(2): 201e-209e. doi: 10.1097/PRS.0b013e31829586a7.
[25] Tong RT, Kohi M, Fidelman N, Kuo YC, Foster R, Peled A, Kolli KP, Taylor AG, LaBerge JM, Kerlan RK Jr. Clinical outcomes of percutaneous drainage of breast fluid collections after mastectomy with expander-based breast reconstruction. J Vasc Interv Radiol. 2013; 24(9):1369-74. doi: 10.1016/j.jvir.2013.04.036. Epub 2013 Jun 28.[Pubmed]
[26] Johnson RK, Wright CK, Gandhi A, Charny MC, Barr L. Cost minimisation analysis of using acellular dermal matrix (Stratticeâ„¢) for breast reconstruction compared with standard techniques. Eur J Surg Oncol. 2013; 39(3):242-7. doi: 10.1016/j.ejso.2012.12.002. Epub 2012 Dec 21.[Pubmed]
Cover letter for group 1
Dear Patient,
I am conducting a research and survey on behalf of the Breast Unit at Wigan on our patients who have had breast reconstruction using acellular dermal matrix.
As you have recently had breast reconstruction using one of the materials mentioned above, I would be grateful if you could participate in this study. Your feedback is very important to the unit and will definitely contribute to service improvement.
I would be very grateful if you could kindly fill in the questionnaire attached and post it back in the accompanying stamped envelope, by 31/01/2014. We will keep all the information confidential and your details will not be revealed at all in our research process.
I would like to express our utmost gratitude to you on behalf of the Breast Unit, and we hope to continue to improve our services to the community.
I hope to receive your questionnaire shortly.
Many thanks,
Miss _________
Core surgical trainee
MBChB, MRCS
Appendix 2: Cover letter for group 2
Dear Patient,
I am conducting a research and survey on behalf of the Breast Unit at Wigan on our patients who have had breast reconstruction.
As you have recently had breast reconstruction, I would be grateful if you could participate in this study. Your feedback is very important to the unit and will definitely contribute to service improvement.
I would be very grateful if you could kindly fill in the questionnaire attached and post it back in the accompanying stamped envelope, by 10/02/2014. We will keep all the information confidential and your details will not be revealed at all in our research process.
I would like to express our utmost gratitude to you on behalf of the Breast Unit, and we hope to continue to improve our services to the community.
I hope to receive your questionnaire shortly.
Many thanks,
Miss _______
Core surgical trainee
MBChB, MRCS
Appendix 3: Breast Q (Courtesy Memorial Sloan-Kettering Cancer and the
University of British Columbia who hold the copyright of the BREAST-Q) Copyright
© 2012 Memorial Sloan Kettering Cancer Center. Permission needs to be gained
before using this Breast Q questionnaire.
1. With your breasts in mind, in the past 2 weeks, how satisfied or
dissatisfied have you been with:
|
|
Very
Dissatisfied
|
Somewhat Dissatisfied
|
Somewhat
Satisfied
|
Very
Satisfied
|
|
a.
How you look in the mirror clothed?
|
1
|
2
|
3
|
4
|
|
b.
The shape of your reconstructed breast(s) when you are wearing a bra?
|
1
|
2
|
3
|
4
|
|
c.
How normal you feel in your clothes?
|
1
|
2
|
3
|
4
|
|
d.
The size of your reconstructed breast(s)?
|
1
|
2
|
3
|
4
|
|
e.
Being able to wear clothing that is more
fitted?
|
1
|
2
|
3
|
4
|
|
f.
How your breasts are lined up in relation to each other?
|
1
|
2
|
3
|
4
|
|
g.
How comfortably your bras fit?
|
1
|
2
|
3
|
4
|
|
h.
The softness of your reconstructed breast(s)?
|
1
|
2
|
3
|
4
|
|
i.
How equal in size your breasts are to each
other?
|
1
|
2
|
3
|
4
|
|
j.
How natural your reconstructed breast(s) looks?
|
1
|
2
|
3
|
4
|
|
k.
How naturally your reconstructed breast(s)
sits/hangs?
|
1
|
2
|
3
|
4
|
|
l.
How your reconstructed breast(s) feels to touch?
|
1
|
2
|
3
|
4
|
|
m.
How much your reconstructed breast(s) feels
like a natural part of your body?
|
1
|
2
|
3
|
4
|
|
n.
How closely matched your breasts are to each other?
|
1
|
2
|
3
|
4
|
|
o.
How your reconstructed breast(s) look now
compared to before you had any breast surgery?
|
1
|
2
|
3
|
4
|
|
p.
How you look in the mirror unclothed?
|
1
|
2
|
3
|
4
|
Please check that you have answered all the questions before going on to the next pageThis question is about breast reconstruction using IMPLANTS. If you do not have an implant(s) please skip to question 3. If you do have an implant(s), please answer question 2 below
2. In the past 2 weeks, how satisfied or dissatisfied have you been with:
|
|
Very
Dissatisfied
|
Somewhat
Dissatisfied
|
Somewhat
Satisfied
|
Very
Satisfied
|
|
a.
The amount of
rippling (wrinkling) of your implant(s) that you can see?
|
1
|
2
|
3
|
4
|
|
b.
The amount of rippling (wrinkling) of your implant(s) that you can
feel?
|
1
|
2
|
3
|
4
|
3. We would like to know how you feel about the outcome of your breast reconstruction surgery. Please indicate how much you agree or disagree with each statement:
|
|
Disagree
|
Somewhat
Agree
|
Definitely
Agree
|
|
a.
Having reconstruction is
much better than the alternative of having no breast(s).
|
1
|
2
|
3
|
|
b.
I would encourage other
women in my situation to have breast reconstruction surgery.
|
1
|
2
|
3
|
|
c.
I would do it again.
|
1
|
2
|
3
|
|
d.
I have no regrets about
having the surgery.
|
1
|
2
|
3
|
|
e.
Having this surgery
changed my life for the better.
|
1
|
2
|
3
|
|
f.
The outcome perfectly
matched my expectations.
|
1
|
2
|
3
|
|
g.
It turned out exactly as
I had planned.
|
1
|
2
|
3
|
Please check that you have answered all the questions before going on to the next page
4. With your breasts in mind, in the past 2 weeks, how often have you felt:
|
|
None
of the time
|
A little of the time
|
Some of the time
|
Most of the time
|
All of
the time
|
|
a.
Confident in a social
setting?
|
1
|
2
|
3
|
4
|
5
|
|
b.
Emotionally able to do
the things that you want to do?
|
1
|
2
|
3
|
4
|
5
|
|
c.
Emotionally healthy?
|
1
|
2
|
3
|
4
|
5
|
|
d.
Of equal worth to other women?
|
1
|
2
|
3
|
4
|
5
|
|
e.
Self-confident?
|
1
|
2
|
3
|
4
|
5
|
|
f.
Feminine in your
clothes?
|
1
|
2
|
3
|
4
|
5
|
|
g.
Accepting of your body?
|
1
|
2
|
3
|
4
|
5
|
|
h.
Normal?
|
1
|
2
|
3
|
4
|
5
|
|
i.
Like other women?
|
1
|
2
|
3
|
4
|
5
|
|
j.
Attractive?
|
1
|
2
|
3
|
4
|
5
|
5. Thinking of your sexuality, since your breast reconstruction, how often do you generally feel:
|
|
None
of the time
|
A little of the time
|
Some of the time
|
Most of the time
|
All of
the time
|
Not Applicable
|
|
a.
Sexually attractive in
your clothes?
|
1
|
2
|
3
|
4
|
5
|
N/A
|
|
b.
Comfortable/at ease
during sexual activity?
|
1
|
2
|
3
|
4
|
5
|
N/A
|
|
c.
Confident sexually?
|
1
|
2
|
3
|
4
|
5
|
N/A
|
|
d.
Satisfied with your sex-life?
|
1
|
2
|
3
|
4
|
5
|
N/A
|
|
e.
Confident sexually about how your breast(s) look
when unclothed?
|
1
|
2
|
3
|
4
|
5
|
N/A
|
|
f.
Sexually attractive when
unclothed?
|
1
|
2
|
3
|
4
|
5
|
N/A
|
Please check that you have answered all the questions before going on to the next page
6. In the past 2 weeks, how often have you experienced:
|
|
None
of the time
|
A little of the time
|
Some of the time
|
Most of the time
|
All of
the time
|
|
a.
Neck pain?
|
1
|
2
|
3
|
4
|
5
|
|
b.
Upper back pain?
|
1
|
2
|
3
|
4
|
5
|
|
c.
Shoulder pain?
|
1
|
2
|
3
|
4
|
5
|
|
d.
Arm pain?
|
1
|
2
|
3
|
4
|
5
|
|
e.
Rib pain?
|
1
|
2
|
3
|
4
|
5
|
|
f.
Pain in the muscles of
your chest?
|
1
|
2
|
3
|
4
|
5
|
|
g.
Difficulty lifting or moving your arms?
|
1
|
2
|
3
|
4
|
5
|
|
h.
Difficulty sleeping
because of discomfort in your breast area?
|
1
|
2
|
3
|
4
|
5
|
|
i.
Tightness in your breast area?
|
1
|
2
|
3
|
4
|
5
|
|
j.
Pulling in your breast
area?
|
1
|
2
|
3
|
4
|
5
|
|
k.
A nagging feeling in your breast area?
|
1
|
2
|
3
|
4
|
5
|
|
l.
Tenderness in your
breast area?
|
1
|
2
|
3
|
4
|
5
|
|
m.
Sharp pains in your breast area?
|
1
|
2
|
3
|
4
|
5
|
|
n.
Shooting pains in your
breast area?
|
1
|
2
|
3
|
4
|
5
|
|
o.
An aching feeling in your breast area?
|
1
|
2
|
3
|
4
|
5
|
|
p.
A throbbing feeling in
your breast area?
|
1
|
2
|
3
|
4
|
5
|
|
q.
Swelling (lymphoedema) of the arm on the side that
you had your mastectomy surgery?
|
1
|
2
|
3
|
4
|
5
|
Please check that you have answered all the questions before going on to the next page
The following questions are about reconstruction using a TRAM or DIEP flap (i.e., reconstruction using skin and fat from you abdomen/tummy area). If you do not have a TRAM or DIEP flap, please skip to question 10. If you do have a TRAM or DIEP flap, please answer the following questions:
7. In the past 2 weeks, with your abdomen (tummy area) in mind, how often have you experienced:
|
|
None
of the time
|
A little of the time
|
Some of the time
|
Most of the time
|
All of
the time
|
|
a.
Difficulty sitting up
because of abdominal muscle weakness (e.g. getting out of bed)?
|
1
|
2
|
3
|
4
|
5
|
|
b.
Difficulty doing everyday activities because of
abdominal muscle weakness (e.g. making your bed)?
|
1
|
2
|
3
|
4
|
5
|
|
c.
Abdominal discomfort?
|
1
|
2
|
3
|
4
|
5
|
|
d.
Abdominal bloating?
|
1
|
2
|
3
|
4
|
5
|
|
e.
Abdominal bulging?
|
1
|
2
|
3
|
4
|
5
|
|
f.
Tightness in your
abdomen?
|
1
|
2
|
3
|
4
|
5
|
|
g.
Pulling in your abdomen?
|
1
|
2
|
3
|
4
|
5
|
|
h.
Lower back pain?
|
1
|
2
|
3
|
4
|
5
|
8. In the past 2 weeks, how satisfied or dissatisfied have you been with:
|
|
Very
Dissatisfied
|
Somewhat
Dissatisfied
|
Somewhat
Satisfied
|
Very
Satisfied
|
|
a.
How your abdomen looks?
|
1
|
2
|
3
|
4
|
|
b.
The position of your navel (belly button)?
|
1
|
2
|
3
|
4
|
|
c.
How your abdominal scars look?
|
1
|
2
|
3
|
4
|
9. In the past 2 weeks, how satisfied or dissatisfied have you been with:
|
|
Very Dissatisfied
|
Somewhat
Dissatisfied
|
Somewhat
Satisfied
|
Very
Satisfied
|
|
a.
How your abdomen feels now compared to before your surgery?
|
1
|
2
|
3
|
4
|
|
b.
How your abdomen looks now compared to before your surgery?
|
1
|
2
|
3
|
4
|
Please check that you have answered all the questions before going on to the next pageThis question is about NIPPLE reconstruction. If you did not have nipple reconstruction, please skip to question 11.If you did have nipple reconstruction, please answer question 10 below.
10. In the past 2 weeks, how satisfied or dissatisfied are you with:
|
|
Very
Dissatisfied
|
Somewhat
Dissatisfied
|
Somewhat
Satisfied
|
Very
Satisfied
|
|
a.
The shape of your reconstructed nipple(s)?
|
1
|
2
|
3
|
4
|
|
b.
How your reconstructed nipple(s) and
areola(s) look?
|
1
|
2
|
3
|
4
|
|
c.
How natural your
reconstructed nipple(s) look?
|
1
|
2
|
3
|
4
|
|
d.
The colour of
your reconstructed nipple/areolar complex?
|
1
|
2
|
3
|
4
|
|
e.
The height (projection) of your reconstructed nipple(s)?
|
1
|
2
|
3
|
4
|
Please check that you have answered all the questions before going on to the next page
11. How satisfied or dissatisfied were you with the information you received about:
|
|
Very
Dissatisfied
|
Somewhat Dissatisfied
|
Somewhat
Satisfied
|
Very
Satisfied
|
|
a.
How the breast
reconstruction surgery was to be done?
|
1
|
2
|
3
|
4
|
|
b.
Healing and recovery
time?
|
1
|
2
|
3
|
4
|
|
c.
Possible complications?
|
1
|
2
|
3
|
4
|
|
d.
The options you were given regarding types
of breast reconstruction?
|
1
|
2
|
3
|
4
|
|
e.
Having breast
reconstruction at the same time as your mastectomy (immediate
reconstruction) versus having it later (delayed reconstruction)?
|
1
|
2
|
3
|
4
|
|
f.
How long the process of
breast reconstruction would take from start to finish?
|
1
|
2
|
3
|
4
|
|
g.
What size you could expect your breasts to be
after reconstructive surgery?
|
1
|
2
|
3
|
4
|
|
h.
How much pain to expect
during recovery?
|
1
|
2
|
3
|
4
|
|
i.
What you could expect your breasts to look like
after surgery?
|
1
|
2
|
3
|
4
|
|
j.
How long after
reconstruction surgery it would take to feel like yourself/feel normal
again?
|
1
|
2
|
3
|
4
|
|
k.
How the surgery could affect future breast cancer
screening (e.g. mammograms)?
|
1
|
2
|
3
|
4
|
|
l.
Lack of sensation in
your reconstructed breast and nipple?
|
1
|
2
|
3
|
4
|
|
m.
What other women experience with their breast
reconstruction surgery?
|
1
|
2
|
3
|
4
|
|
n.
What the scars would
look like?
|
1
|
2
|
3
|
4
|
Please check that you have answered all the questions before going on to the next page
12. These questions ask about the Consultant Surgeon in charge of your breast reconstruction surgery.Did you feel that he/she:
|
|
Definitely Disagree
|
Somewhat Disagree
|
Somewhat Agree
|
Definitely
Agree
|
|
a.
Was competent?
|
1
|
2
|
3
|
4
|
|
b.
Gave you confidence?
|
1
|
2
|
3
|
4
|
|
c.
Involved you in the
decision-making process?
|
1
|
2
|
3
|
4
|
|
d.
Was reassuring?
|
1
|
2
|
3
|
4
|
|
e.
Answered all your
questions?
|
1
|
2
|
3
|
4
|
|
f.
Made you feel comfortable?
|
1
|
2
|
3
|
4
|
|
g.
Was thorough?
|
1
|
2
|
3
|
4
|
|
h.
Was easy to talk to?
|
1
|
2
|
3
|
4
|
|
i.
Understood what you
wanted?
|
1
|
2
|
3
|
4
|
|
j.
Was sensitive?
|
1
|
2
|
3
|
4
|
|
k.
Made time for your
concerns?
|
1
|
2
|
3
|
4
|
|
l.
Was available when you
had concerns?
|
1
|
2
|
3
|
4
|
Please check that you have answered all the questions before going on to the next page
13. These questions ask about members of the medical team other than the Consultant Surgeon in charge of your care (i.e. nurses and other doctors who looked after you).Did you feel that they
|
|
Definitely
Disagree
|
Somewhat Disagree
|
Somewhat Agree
|
Definitely
Agree
|
|
a.
Were professional?
|
1
|
2
|
3
|
4
|
|
b.
Treated you with
respect?
|
1
|
2
|
3
|
4
|
|
c.
Were knowledgeable?
|
1
|
2
|
3
|
4
|
|
d.
Were friendly and kind?
|
1
|
2
|
3
|
4
|
|
e.
Made you feel
comfortable?
|
1
|
2
|
3
|
4
|
|
f.
Were thorough?
|
1
|
2
|
3
|
4
|
|
g.
Made time for your
concerns?
|
1
|
2
|
3
|
4
|
Please check that you have answered all the questions
BREAST-Q © Memorial Sloan-Kettering Cancer Center and The University of British Columbia, 2006, All rights reserved


