Case Report

Advanced Sebaceous Gland Carcinoma of the Eyelid in a Pthisical Eyeball Managed by Exenteration with Skin Grafting
*, Surekha Bangal* Satish Sonawane*Dharmdip Patel *Akshay Bhandari * Waman Chavan
- * Ophthalmology, Pravara Institute of Medical Sciences, Loni, Maharashtra, Ahmednagar, India
- Published 10 October, 2014
This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/3.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited
Abstract
Sebaceous gland carcinoma is rare malignant neoplasm involving eyelids having aggressive local behaviour and metastasis to regional lymph nodes and distant organs.A 59 year old male presented with growth involving left upper and lower eyelid since two years. His vision in right eye was 20/40 and left eye was no PL. There were multiple nodular swellings involving whole upper lid, lateral canthus and lateral half of lower eye lid. Eye ball structures were not visible. MRI orbit was suggestive of heterogeneously enhancing lesion seen on anterolateral aspect of left globe involving orbicularis oculi, lacrimal gland, lateral, superior and inferior recti and inferior oblique along with orbital fat. The eyeball was pthisical. CT brain showed no intracranial extension. Biopsy was suggestive of sebaceous gland carcinoma. Left orbital exenteration was done with skin grafting. Exenteration is currently performed less often but it is still indicated for advanced and diffuse sebaceous gland carcinoma with orbital invasion.
Keywords
Eye lid, Sebaceous gland carcinoma, exenteration, skin grafting
Introduction
Sebaceous gland carcinoma (SGC) is found most frequently in the ocular region, more commonly in upper eye lid (75%). Thiersch reported the first case of periorbital SGC in 1865. SGC is a malignant neoplasm arising either from the meibomian glands in the tarsus or from zeis’s glands of eye lash follicles and also from caruncle and eyebrow [1]. It is a rare eyelid tumour with a mortality rate second only to malignant melanoma [2]. SGC is capable of aggressive local behavior and metastasis to regional lymph nodes and distant organs.
Case report
A 59 years old male presented with growth on left upper and lower eyelid since 2 years (Figure 1). There was history of surgery done for a swelling on the left upper lid 15 years back. He was not having history of systemic disease and systemic examination was within normal limits. Preauricular, post auricular and submandibular lymph nodes were not palpable.

Figure 1: Preoperative clinical photograph
On ophthalmic examination, vision in right eye was 20/40 and left eye was no PL. Right eye anterior segment and fundus examination was normal except for the presence of immature senile cataract. There were multiple nodular swellings with diffuse thickening of whole left upper eye lid, lateral canthus and lateral half of left lower lid. The skin over the swelling at the lateral canthus showed multiple areas of ulceration. Trichiasis and entropion was present in left lower eye lid. Left eye ball structures were not visible except for the opaque cornea. Extra ocular movements were restricted. Laboratory investigations, X-ray chest and lumbo-sacral spine, USG abdomen were normal. MRI orbit plain and contrast showed heterogeneously enhancing lesion on anterior and lateral aspect of pthisical left globe involving orbicularis oculi, lacrimal gland, lateral, superior, inferior recti and inferior oblique with involvement of orbital fat and slight deformation of globe (Figure 2). CT brain and orbit did not reveal bone involvement or intracranial extension. Histopatholoical examination of the incisional biopsy showed well differentiated lobules of tumour cells with sebaceous differentiation (Figure 3).
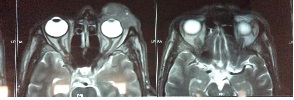
Figure 2: MRI brain and orbit
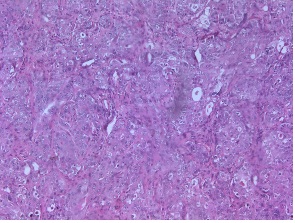
Figure 3: Nuclear and cellular pleomorphism
Considering the highly malignant nature of the neoplasm, involving the orbital contents and having poor prognosis decision of exenteration was taken. Written informed consent was obtained. Left orbital exenteration with skin grafting was done under general anaesthesia. (Figure 4). Postoperatively histopatholoical diagnosis of SGC was confirmed (Figure 5). There were no signs of recurrence during follow up examination for 4 months (Figure 6). Patient is advised regular follow up. Eye prosthesis was given after 8 months. (Figure 7).

Figure 4: Orbital exenteration with skin graft

Figure 5: Exenterated mass (6x5 cm)

Figure 6: Four month postoperative

Figure 7: After eye prosthesis
Discussion
Sebaceous gland carcinoma (SGC) is found most frequently in the ocular region. SGC is considered as the third most common eyelid malignancy after basal and squamous cell carcinoma. It is a rare highly malignant eyelid tumour with a mortality rate second only to malignant melanoma. It represents 0.2% to 0.7% of all eyelid tumours and 1% to 5.5% of all eyelid malignancies. SGC is more frequent in women (73%) than in men and usually seen in the 6th to 7th decade of life [3]. Myriads of inflammatory conditions such as blepharitis, blepharoconjunctivitis, meibomianitis, ocular cicatricial pemphigoid and recurrent chalazion can be one of the various clinical presentations of SGC [4]. Our patient presented in the advanced stage of the disease with involvement of the orbital structures. Highly malignant nature of this tumour warns prompt wide surgical excision for better outcome and higher survival rates. Histopatholoical examination showed well differentiated lobules of tumour cells with sebaceous differentiation. Individual lobule showed nuclear and cellular pleomorphism with foamy cytoplasm [5]. Cryotherapy and radiotherapy has limited role in inoperable cases or those who refuse surgery. Considering the above facts exenteration of the left orbit was indicated in our case.
Conclusion
Exenteration is currently performed less often but it is still indicated for advanced and diffuse SGC with orbital invasion for better prognosis.
Author contribution
SB and AB carried out the
literature search and prepared the draft manuscript, SS and
AB carried out the experiments and interpreted the results,
AB designed the study and performed the analysis, AB,
DP and WC conceived the study, participated in design
and edited the final manuscript. All authors read and approved the final
manuscript for submission.
Ethical Consideration
The written informed consent was obtained from the patient for publication of this case report.
Funding
None declared
Conflicts of Interests
The authors declare that there are no conflicts of interests.
Acknowledgement
None
References
[1].Boniuk M, Zimmerman LE. Sebaceous carcinoma of the eyelid, eyebrow, caruncle and orbit. Trans Am Acad Ophthalmol Otolaryngology 1968; 72:619–41
[Pubmed]
[2].Marlis Z, Hintschich CR, Garner A. Sebaceous carcinoma of the eyelid a clinic pathological study. Br J Ophthalmol 1998;82:1049-55.[Pubmed]
[3].Doxanas MT, Green WR. Sebaceous gland carcinoma: review of 40 cases. Arch Ophthalmol 1984;102:245-9
[Pubmed]
[4].Kenneth CS, Fong MA, Raman Malhotra. Common eyelid malignancies clinical features and management options. OT 2005:November 18; 30-34. http://www.optometry.co.uk/uploads/articles/aff9794de0a3c3caead621804b5ff111_Malhora181105.pdf [Last accessed October 14, 2014][Pubmed]
[5].Harsh Mohan. Text book of pathology. 3rd Edition, Jaypee Brothers Medical Publishers (p) Ltd, New Delhi, 1998:580.


