Original Article

Analysis of V5 Predicting Radiation Pneumonitis in Patients Received Thoracic Irradiation Treatment
1,Bu-Hai Wang, Xiao-Lei Wang, Jian-Qi Yang, Wei Hua
- Clinical College, Yangzhou University Medical Academy, Jiangsu Province, Yangzhou, China
- 1Northern Jiangsu People’s Hosptial, Jiangsu Province, Yangzhou, China
- Submitted:Monday, March 3, 2014
- Accepted:Saturday, April 19, 2014
- Published:Wednesday, April 30, 2014
This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/3.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited
Abstract
Background
To examine V5 as the dosimetric predictor of radiation pneumonitis in patients received thoracic radiation therapy beside V20, V30 and MLD.
Methods
One-hundred patients receiving thoracic irradiation from 2011 to 2012 at Subei People’s Hospital were retrospectively reviewed, from which esophageal and lung cancer patients were eighty-six and fourteen, respectively. Pneumonitis was graded by using the Common Terminology Criteria for Adverse Events version 4.0. Dosimetric parameters (V5, V10, V15, V20, V25, and V30) were entered as continuous variables. A cross tabulation, an independent t-test and a receiver observer curve (ROC) were used to analyze the data.
Results
In the final, 50(50%) of total 100 patients had grade 0-1 RP, 44(44%) had grade 2 RP, 4(4%) had grade 3 RP and 2(2%) had grade 4 RP. No significant discrepancy was found between grade 0-1 and grade 2-4 in the following clinical parameters, such as age, gender, ECOG performance status and history of chemotherapy. No significant difference of RP incidence was found between Non-CT and Concurrent-CT arms (χ2 = 0.026, P > 0.1). The ROC indicated the AUC value was 0.627 for V5 (P = 0.034).
Conclusions
Those patients whose DVH parameters such as MLD, V20 and V30 were constrainted still occur RP. V5 was a statistically significant parameter associated with grade 2-4. We recommend V5 should be kept as low as possible, in addition to the conventional dosimetric factors. 50% of V5 is considered to be a threshold, the incidence of grade≥2 RP in the group with V5< 50% and ≥ 50% were 59.36% and 33.3 %( P < 0.05).
Background
Radiation therapy (RT) is an integral component of thoracic tumor therapy and is employed with chemotherapy as a definitive option in advanced unresectable disease. Radiation-induced lung injury (RILI) may be seemed as the progression of damages including radiation pneumonitis (RP) and radiation fibrosis [1]. To counteract this fatal phenomenon, intensity-modulated radiation (IMRT) and 3D-CRT was used by limiting dose-volume parameters such as dose-volume V20, V30, mean lung dose (MLD), which validity and significance has been confirmed in most studies [2]. However, some patients still occured RP though those predictive facotors were controlled in rational range. The low dose volume of lung, primarily V5 was paid more and more attention and some retrospective analysis revealled its role preliminarily in predicting the incidence of RP [3]. We conducted a retrospective study to investigate the dosimetric parameters predicting acute and chronic lung injury in esophageal and lung cancer patients undergoing irradiation treatment with or without chemotherapy.
Materials and methods
Patient selection
One-hundred patients receiving thoracic irradiation with or without concurrent chemotherapy from 2011 to 2012 at Northern Jiangsu People’s Hospital were retrospectively reviewed, from which esophageal and lung cancer patients were eighty-six and fourteen, respectively.
Radiation therapy and dosimetric factors
All patients were treated with 3D-CRT or IMRT. Planning computer tomography (CT) images were taken on a CT simulator (GE) and then were transferred to treatment planning system (TPS, Varian Eclipse DX). Photon beam energy is to be individualized based on the anatomic location of the tumors and beam path from 6 to 15MV. Lung cancer plan: The gross tumor volume (GTV) was defined through the superimposition of each visible tumor on each series of CT scans. The margin of the clinical tumor volume (CTV) was 0.8cm(adenocarcinoma) or 0.6cm (squamous carcinoma) beyond the GTV. Bronchus margin was extended 1.5cm, including lymphatic positive region. The planning target volume (PTV) was generated from a 0.5cm isotropic expansion of the CTV. The IMRT plan was designed as 4 to 7 fields irradiating and a total dose of 60-70Gy was delivered at 1.8-2.0Gy per fraction. While achieving the target dose, each specific organ at risk (OAR) such as normal lung, heart, esophagus, and spinal cord were kept below a maximum. Esophageal cancer plan: The GTV was identified thickness of esophageal wall that was more than 5mm. The CTV was then expanded from the GTV with a margin 1.0cm laterally and a 3.0cm margin in the superior and inferior dimensions. An additional 0.5cm laterally expansion and 1.0cm in the superior and inferior dimensions around the CTV was included for the PTV. The IMRT plan was designed as 3 to 7 fields irradiating and a total dose of 58-70Gy was delivered at 1.8-2.2Gy per fraction.
The TPS was used to compute the dose-volume histogram (DVH), which was utilized to determine the dose received by 5 and 95% of GTV, CTV and PTV, the volume of lung receiving more than 5, 10, 15, 20, 25 and 30 Gy (V5, V10, V15, V20, V25, V30) and doses received by OAR. We tried to minimize the risk of pulmonary toxicity by limit the mean lung dose (MLD), V20, V30 as 20Gy, 30%, 15% or less, because their correlation with RP was demonstrated in most studies.
Chemotherapy
Cisplatin-based chemotherapy with paclitaxel or 5-FU was combined with RT for some patients, others received RT only. Concurrent or sequential chemoradiotherapy were both applied. More details could be are summarized in [Table 1]
Table-1
:
Patient characteristics(n=100)
|
|
Characteristic
|
Number of
patients (%)
|
|
Gender
|
|
|
|
Male
|
|
72(72)
|
|
Female
|
|
28(28)
|
|
Age(yr)
|
|
|
|
Range
|
41-84
|
|
|
Median
|
63.5
|
|
|
≤65
|
|
58(58)
|
|
>65
|
|
42(42)
|
|
ECOG performance status
|
|
|
≤1
|
|
88(88)
|
|
≥2
|
|
12(12)
|
|
Previous CT
|
|
7(7)
|
|
Previous and subsequent CT
|
4(4)
|
|
Concurrent CT
|
53(53)
|
|
Non-CT
|
36(36)
|
|
RP = radiation pneumonitis, CT = chemotherapy, ECOG =
Eastern Cooperative Oncology Group.
|
Statistical analysis
Statistical analysis was done using SPSS (version 17.0 SPSS
Inc., Chicago, IL, USA). Dosimetric parameters (V5, V10, V15, V20, V25, and V30)
were entered as continuous variables. A cross tabulation, an independent t-test
and a receiver observer curve (ROC) were used to analyze the data. Statistical
significance was set at P values ≤0.05. Written informed consent was taken to
any treatment in all patients and the study protocol including the use of the
database was approved by the Institutional Review Board of Northern Jiangsu
People’s Hospital and met the guidelines of the responsible governmental
agencies.
Results
RP was diagnosed by serial follow-up interviews and CT scans. The grade of pneumonitis was defined through the Common Terminology Criteria for Adverse Events, version 4.0 (CTCAE 4.0) (grade 1, asymptomatic, clinical, or diagnostic observations only, intervention not indicated; grade 2, symptomatic, medical intervention indicated, limiting instrumental activities of daily living; grade 3, severe symptoms, limiting self-care activities of daily living, oxygen indicated; grade 4, life-threatening respiratory compromise, urgent intervention indicated; grade 5, death).
The follow-up ranged from 1 to 30 months, with 14 months being the median value.[Table 1] shows the characteristics of the patients. In the final, 50 (50%) of total 100 patients had grade 0-1 RP, 44 (44%) had grade 2 RP, 4 (4%) had grade 3 RP and 2 (2%) had grade 4 RP. The male-female ratio in Grade 0-1 and Grade 2-4 RP was no significantly difference (χ2 = 1.786, P = 0.181) [Table 2] No significant discrepancy was found between two arms in the following clinical parameters, such as age, gender, ECOG performance status and history of chemotherapy. For history of chemotherapy, 36 patients received RT alone, 15 of which developed Grade 2-4 RP, 7 patients had pre-RT CT, 2 had CT pre-after-RT, 53 had concurrent chemoradiotherapy, the incidence of grade 2-4 RP was 41.67%, 42.86%, 100% and 43.40%, respectively. No significant difference of RP incidence was found between Non-CT and Concurrent-CT arms (χ2 = 0.026, P = 0.871).
|
Factor
|
Number of
patients (%)
|
χ2
|
P-value
|
|
|
|
Grade 0-1
|
Grade 2-4
|
|
|
|
Gender
|
|
|
|
|
|
|
Male
|
|
39(39)
|
33(33)
|
1.786
|
0.181
|
|
Female
|
|
11(11)
|
17(17)
|
|
|
|
Age(yr)
|
|
|
|
|
|
|
≤65
|
|
32
|
26
|
1.478
|
0.224
|
|
>65
|
|
18
|
24
|
|
|
|
ECOG performance status
|
|
|
|
|
|
≤1
|
|
73(73)
|
25(25)
|
3.168
|
0.075
|
|
≥2
|
|
6(6)
|
6(6)
|
|
|
|
Concurrent CT
|
30(30)
|
23(23)
|
0.026
|
0.871
|
|
Non-CT
|
21(21)
|
15(15)
|
|
|
For parameters of radiation, we could find in the [Table 3]The parameters such as mean dose, total dose, fractions and fractionated dose was no significantly different between the incidence of grade 0-1 and grade 2-4 RP. Their P value was all ≥ 0.05 (P = 0.091, 0.47, 0.23, 0.362, respectively).
|
|
|
MEAN
|
SD
|
P-value
|
|
Means dose
|
Grade 0-1
|
10.17
|
2.21
|
0.091
|
|
Grade 2-4
|
10.91
|
2.07
|
|
Total dose
|
Grade 0-1
|
59.1
|
4.96
|
0.47
|
|
Grade 2-4
|
58.36
|
5.3
|
|
Fractions
|
Grade 0-1
|
28.76
|
2.34
|
0.23
|
|
Grade 2-4
|
28.18
|
2.41
|
|
Fractionated dose
|
Grade 0-1
|
2.056
|
0.824
|
0.362
|
|
Grade 2-4
|
2.071
|
0.0852
|
|
SD = standard
deviation
|
The ROC (receiver observer curve) curve indicated the AUC (area under curve) value was 0.627 for V5 (P = 0.034). V5 was the only statistically significant parameter associated with grade 2-4; the concrete data were listed in[Table 4] ROC curve was showed in[Figure 1,Figure 2,] as part of official publication
|
|
|
MEAN
|
SD
|
ROC
|
P-value
|
|
|
|
AUC
|
P-value
|
|
V 5(%)
|
Grade 0-1
|
49.95
|
12.89
|
0.627
|
0.028
|
0.034
|
|
Grade 2-4
|
55.69
|
13.81
|
|
|
|
V10(%)
|
Grade 0-1
|
40.49
|
9.73
|
0.592
|
0.111
|
0.15
|
|
Grade 2-4
|
40.49
|
10.08
|
|
|
|
V15(%)
|
Grade 0-1
|
27.75
|
7.46
|
0.573
|
0.208
|
0.2
|
|
Grade 2-4
|
29.62
|
7.04
|
|
|
|
V20(%)
|
Grade 0-1
|
18.61
|
5.78
|
0.51
|
0.869
|
0.59
|
|
Grade 2-4
|
19.19
|
5.02
|
|
|
|
V25(%)
|
Grade 0-1
|
12.12
|
4.55
|
0.464
|
0.537
|
0.43
|
|
Grade 2-4
|
11.4
|
4.51
|
|
|
|
V30(%)
|
Grade 0-1
|
7.76
|
3.65
|
0.492
|
0.885
|
0.72
|
|
Grade 2-4
|
7.49
|
3.62
|
|
|
|
SD = standard deviation, ROC = receiver observer curve,
AUC = area under curve, V5-30 = volume percentage of tumor-free normal
lung receiving at least 5-30Gy.
|
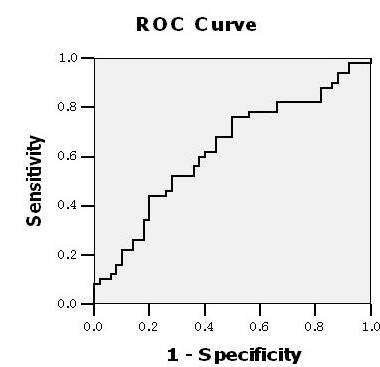
Fig 1. The ROC curve of V5 yielded 0.627 of the AUC, which was statistically significant (P = 0.034).
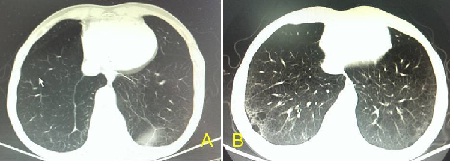
Figure 2 showed A 62-year-old man treated with concurrent chemoradiation for esophageal squamous carcinoma. The V5 was 51%, the V20 was 23% and V30 was 8.0%. The patient developed grade 3 pulmonary toxicity approximately 4 months after completion of two cycles of concurrent chemoradiotherapy. (A) Baseline pretreatment computed tomography (CT) of the Chest. (B) CT of the chest 4 months after treatment revealed bronchiectasis, ground-glass opacities, and infiltrates within the treatment field.
Discussion
The DVH parameters are crucial and useful for predicting the occurrence of RP. For the moment, MLD, V20 and V30 have been shown to be significantly associated with the incidence of RP. Different studies give different “threshold’’ constraints. The volume acknowledged widely but not absolutely was MLD≤20Gy, V20 ≤35 %, V30 ≤15% [4]. We found when we control these conventional parameters; the incidence of RP seems lower in clinical practice. How to explain some patients still occur RP? We consider a large area of low-dose radiation related. To achieve good conformal dose distribution around the target, MLD, V20 and V30 was restricted as low as possible by using IMRT, Rapid-Arc or dynamic conformal multiple-arc technique so that the low-dose exposure area of normal tissue is inevitably increased [5]. V5 as a typical parameter attracts more attention. Yorke’s study found that occurrence of RP was related to low-dose radiation area, especially V5-V13 [6]. A research of MD. Anderson showed V5 was a significant factor with grade ≥ 3 RP in patients with NSCLC treated with concurrent chemotherapy and 3D-CRT, the threshold value was 42% [7]. Similarly, Jo et al. analyzed pulmonary dosimetric parameters and confirmed V5 was associated with Grade ≥ 2 RP in patients received helical-tomotherapy-based hypofractionated radiotherapy for pulmonary metastases with statistical significance, the threshold value of V5 was 65% [8]. Song reported a study of 37 patients with NSCLC treated with helical tomotherapy and identified V5 > 60% as the only independent risk factor for the development of grade 3 RP [9]. The concrete threshold values vary but not fluctuate too much. In our study, 50% of V5 is considered to be a threshold, the incidence of grade ≥ 2 RP in the group with V5 < 50% and ≥ 50% were 59.36% and 33.3% (P < 0.05). 7 patients developed grade ≥ 3 RP with V5 > 58% and V10 > 42%. The ROC curve of V5 yielded 0.627 of the AUC with low sensitivity but still significant. Maybe the bias concerned with less sample size.
Intensity-modulate radiotherapy (IMRT) is applied in more and more radiation oncology Dept. in China because of its better conformity, accuracy and controllability than 3D-CRT. RP is a common and fatal complication in the past. With the revolution of technique, such as IMRT, and SBRT (stereotactic body radiotherapy), radiation comes into a new area.
TTrivial and complicated factor influence the incidence of RP, especially grade 2-4 that would threaten life. We just discuss elements that result in grade 2-4 RP. Lung disease patients especially those who have poor pulmonary function or with a smoking history take greater risk [10]. We did not collect these data because in most departments of China, patients do not examine pulmonary function in general before radiation. Those patients have notable symptom abandon therapy directly. But now we start to assess each possible person to receive therapy.
Elderly patients have increased pulmonary toxicity after thoracic irradiation in several prospective trials [11,14]. Jordan’s study showed that age ≥ 70 years was the most significant predictor for symptomatic pneumonitis. The reason maybe the decreased tolerance to thoracic radiation(dilatation of alveoli, enlargement of airspaces, and loss of supporting tissue for peripheral airways), cardiac and or pulmonary comorbidities, not well-defined dosimetric parameters in radiation treatment [8]. For elders, we should make assurance doubly sure.
GGender was found to be a risk factor for RP and females are danger than males in most studies, especially women with smaller lung volume. But our data revealled the RP incidence was no different. This seemed credible according to Zhang’s meta-analysis of large sample [15].
Chemotherapy seems correlating with RP. Earlier meta-analysis of 461 patients with NSCLC revealled that concurrent chemoradiotherapy was easier to develop RP than radiotherapy alone [16]. Recently Parashar’s[17] study also showed risk of RP was significantly increased in concurrent chemotherapy of advanced lung cancer if the field size is ≥ 200 cm. In addition to this, few studies confirmed this conclusion. We understand RT combined with chemotherapy increase the cytotoxicity of blood and normal tissue. And there are a variety of chemotherapy regimens, we still lack of irrefutable evidence. Whether concurrent or sequential chemotherapy is safer is uncertain, either. We could use amifostine as protective agent to reduce the risk of RP [18].
Conclusions
In our study, after thoracic irradiation by using conventional technique IMRT, grade 0-1 RP developed in 50%, grade 2 in 44%, grade 3 in 4% and grade 4 in 2% of all patients. When MLD, V20,V30 and other potential related parameters were controlled in safe range, V5 was proved to be significantly associated with RP, and the ROC curve indicated the AUC value was 0.627 (P = 0.034). By further data analyzing, we recommend V5 should be kept as low as possible, in addition to the conventional dosimetric factors, when V5 < 50% vs. V5≥ 50%, the incidence of grade ≥ 2 RP was 59.36% and 33.3% (P <0.05)..
List of abbreviations used
RP, Radiation pneumonitis; CT, Chemotherapy; DVH, Dose-volume histogram; MLD, mean lung dose; IMRT, Intensity modulated radiation therapy
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
All the authors have made substantial contributions to
conception and design, acquisition of data, or analysis and interpretation of
data.
BHW organized the study and was primarily responsible for drafting the
manuscript.
JQY and XLW gathered primary data, follow up results and guided
statistical analysis and also participated in drafting the manuscript.
WH
helped to investigate data of dose, parameter and CT images of radiotherapy.
BHW coordinated the research and provided close guidance throughout the process.
All authors read and approved the final manuscript.
The authors have
been involved in drafting the manuscript or revising it critically and have all
given final approval of the version to be published.
Xiao-Lei Wang is joint
first author.
Acknowledgments
This work was supported by the Jiangsu Ministry of Health grant (grants YZ201027).
References
[1]Abid SH, Malhotra V, Perry MC: Radiation-induced and chemotherapy-induced pulmonary injury. Curr Opin Oncol 2001, 13(4):242-248.[Pubmed].
[2]. Kobayashi H, Uno T, Isobe K, Ueno N, Watanabe M, Harada R, Takiguchi Y, Tatsumi K, Ito H: Radiation pneumonitis following twice-daily radiotherapy with concurrent carboplatin and paclitaxel in patients with stage III non-small-cell lung cancer. Jpn J Clin Oncol 2010, 40(5):464-469 [Pubmed].
[3]Gridelli C, Langer C, Maione P, Rossi A, Schild SE: Lung cancer in the elderly. J Clin Oncol 2007, 25:1898-1907 [Pubmed].
[4]. Kharofa J, Gore E: Symptomatic Radiation Pneumonitis in Elderly Patients Receiving Thoracic Irradiation. Clinical Lung Cancer 2013, 14(3):283-287 [Pubmed].
[5]. Takeda A, Kunieda E, Sanuki N, Ohashi T, Oku Y, Sudo Y, Iwashita H, Ooka Y, Aoki Y, Shigematsu N, Kubo A: Dose d istribution analysis in stereotactic body radiotherapy using dynam icconformal multiple-arc therapy. Int J Radiat Oncol Biol Phys 2009, 74:363-369[Pubmed].
[6]Yorke ED, Jackson A, Rosenzweig KE, Braban L, Leibel SA, Ling CC: Correlation of dosimetric factors and radiation pneumonitis for non-small cell lung cancer patients in a recently completed dose escalation study. Int J Radiat Oneol Biol Phys 2005, 63:672-682.
[Pubmed].
[7]Wang SL, Liao ZX, Wei X, Liu HH, Tucker SL, Hu CS, Mohan R, Cox JD, Komaki R: Analysis of clinical and dosimetric factors associated with treatment-related pneumonitis (TRP) in patients with non-small-cell lung cancer (NSCLC) treated with concurrent chemotherapy and three-dimensional conformal radiotherapy (3D-CRT). Int J Radiat Oncol Bid Phys 2006, 66:1399-1407.
[8]. Jo IY, Kay CS, Kim JY, Son SH, Kang YN, Jung JY, Kim KJ: Significance of low-dose radiation distribution in development of radiation pneumonitis after helical-tomotherapy-based hypofractionated radiotherapy for pulmonary metastases. Journal of Radiation Research 2013[Epub ahead of print]
[9]Song CH, Pyo H, Moon SH, Kim TH, Kim
DW, Cho KH: Treatment-related pneumonitis and acute esophagitis in
non-small-cell lung cancer patients treated with chemotherapy and helical
tomotherapy. Int J Radiat Oncol Biol Phys 2010, 78:651-658 [Pubmed].
[10]Li Y, Zhu SC, Chi ZF: Analysis on the risk factors of radiation pneumonitis after three-dimensional radiotherapy in lung cance patients. Cancer Res Prev Treat 2007, 34(8):586-589.
[11]Schild SE, Mandrekar SJ, Jatoi A, McGinnis WL, Stella PJ, Deming RL, Jett JR, Garces YI, Allen KL, Adjei AA: The value of combined-modality therapy in elderly patients with stage III nonsmall cell lung cancer. Cancer 2007, 110(2):363-368. [Pubmed]
[12]Kean HM, Stella PJ, Hillman SL, Rowland KM, Cannon MW, Behrens RJ, Gross GG, Sborov MD, and Friedman EL, Jatoi A: Exploring therapeutic decisions in elderly patients with non-small cell lung cancer: results and conclusions from North Cen-tral Cancer Treatment Group Study N0222. Cancer Invest 2011, 29:266-271.
[13]. Schild SE, Stella PJ, Brooks BJ, Mandrekar S, Bonner JA, McGinnis WL, Mailliard JA, Krook JE, Deming RL, Adjei AA, Jatoi A, Jett JR: Results of combined-modality therapy for limited-stage small cell lung carcinoma in the elderly. Cancer 2005, 103:2349-2354. [Pubmed].
[14]Claude L, Pérol D, Ginestet C, Falchero L, Arpin D, Vincent M, Martel I, Hominal S, Cordier JF, Carrie C: A prospective on radiation pneumonitis following conformal radiation therapy in non--small--celllung cancer: clinical and dosimetric factors analysis. Radiother Oncol 2004, 71:175-181 [Pubmed].
[15]. Zhang XJ, Sun JG, Sun J, Ming H, Wang XX, Wu L, Chen ZT: Prediction of radiation pneumonitis in lung cancer patients: a systematic review. J Cancer Res Clin Oncol 2012, 138:2103-2116 [Pubmed].
[16]ByharDT RW, Scott C, Sause WT, Ming H, Wang XX, Wu L, Chen ZT: Response, toxicity, failure patterns, and smvival in five radiation therapy oncology group (RTOG) trials of sequential and/or concurrent chemotherapy and radiotherapy for locally advanced non-small cell carcinoma of the lung. Int J Radiat Oncol Biol Phys 1998, 42:469-478.
[17]. Parashar B, Edwards A, Mehta R, Pasmantier M, Wernicke AG, Sabbas A, Kerestez RS, Nori D, Chao KS: Chemotherapy significantly increases the risk of radiation pneumonitis in radiation therapy of advanced lung cancer. Am J Clin Oncol 2011, 34(2):160–164. [Pubmed].
[18]Mehta V: Open label multicenter trial of subcutaneous amifostine (Ethyol) in the prevention of radiation induced esophagitis and pneumonitis in patients with measurable, unresectable non-small cell lung cancer. Semin Oncol 2004, 31:42-46 [Pubmed].


