Case Report

How Common are Benign Retroperitoneal Tumors? A Case Series with Review of Literature.
*Yamini Chitra V *Paramesh K N *Rithin Punjala Sai
- *Surgical Gastroenterology and Bariatric centre, Vydehi Institute of Medical Sciences
and Research Centre, Karnataka, Bangalore, India
- Submitted: Saturday, December 06, 2014
- Accepted: Sunday, January 18, 2015
- Published: Saturday, January 24, 2015
This is an Open Access article distributed under the terms of the Creative Commons Attribution License ((http://creativecommons.org/licenses/by/3.0)which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited
Abstract
Introduction
Benign retroperitoneal tumors are usually rare and form 4%-25% of all retroperitoneal tumors in the past. Due to advanced imaging modalities the number of incidental tumors has increased and now forms up to 60% of all retroperitoneal tumors. Based on imaging techniques, various diagnostic criteria have been developed to ascertain origin and to determine the benign or malignant nature of these tumors. Large sizes, symptoms, heterogenous lesions on imaging, are considered as signs of malignancy. But surprises do occur.
Case Presentation
We present two cases of benign retroperitoneal tumors, first a case of massive retroperitoneal tumor in a 30 year old male with vague abdominal pain. Preoperative computed tomography revealed heterogeneously enhancing mass 20×15×12 cm with cystic areas and calcifications, suspected to be malignant and of pancreatic origin. Peroperatively it was of retroperitoneal origin and pancreas was compressed &pushed superiorly. Patient underwent total excision of tumor. Second case, a 24 year male with incidentally diagnosed presacral lesion, 7×7cm size, with extension into S1 sacral foramina. Heterointensity on T2 W magnetic resonance imaging gave a suspicion of malignant nerve sheath tumor and the tumor was excised in toto. Both the patients postoperative histopathology showed a benign schwannoma and immunohistochemistry was positive for S 100. Both patients are tumor free 12 months and 7 months respectively after surgery.
Conclusion
Benign retroperitoneal tumors can grow to a large size before they become symptomatic. Massive size is often misleading regarding both site of origin of tumor and the benign or malignant nature of it. Preoperative imaging will not always give a clue to the nature of it making preoperative diagnosis of benign tumors very difficult. But complete excision of tumor gives excellent results.
Key words
Schwannoma, Retroperitoneum, Computed tomography, Magnetic resonance imaging, Immunohistochemistry
Introduction
Benign retroperitoneal tumors are usually rare and formed 4%-25% of all retroperitoneal tumors in the past. Due to advanced imaging modalities the number of incidental tumors has increased and now forms up to 60% of all retroperitoneal tumors [1]. Based on imaging techniques, various diagnostic criteria have been developed to ascertain origin and to determine the benign or malignant nature of these tumors. Large size, symptoms are considered as signs of malignancy. But surprises do occur.
We would like to present two of these tumors. One, a very massive tumor with areas of necrosis on imaging, mimicking malignancy and another, small but in a critical area, preoperative imaging suggested a neural origin with scalloping of the adjacent bone, both were histologically benign schwannomas. The clinical presentation, diagnostic modalities and treatment options of retroperitoneal tumors, especially schwannomas are discussed.
Case Presentation
Case 1
A 30 year old male patient presented with dull aching abdominal pain of 6 months duration in right upper quadrant of abdomen and no weight loss or vomiting or bowel or bladder disturbance. There was no significant past history. Clinical examination revealed a firm to hard mass involving entire upper half of abdomen. A contrast enhanced CT abdomen revealed a well defined, heterogeneously enhancing mass 20×15×12 cm, with smooth margins in the retrogastric region (Figure 1).
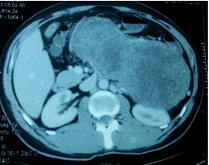
Figure 1- Contrast CT showing heterodense tumor, areas of cystic degeneration
It had few cystic areas suggestive of necrosis and multiple calcifications and it was displacing all major vessels (Figure 2). An upper GI endoscopy was normal. A preoperative diagnosis of retroperitoneal tumor of probable pancreatic origin was made.
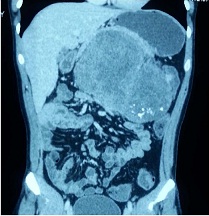
Figure 2- CT-Coronal section showing tumor calcifications
Peroperatively tumor was of retroperitoneal origin, 22×15 cm size, of variable consistency. Pancreas was compressed & pushed superiorly. All major blood vessels were separated from the tumor. Entire tumor was excised
in toto (Figure 3).

Figure 3- Excised specimen of patient 1
Postoperative period was uneventful. HPE showed a well circumscribed tumor composed of cellular Antoni A areas and Antoni B areas with areas of hyaline & cystic degeneration & ischaemic necrosis (Figure 4).
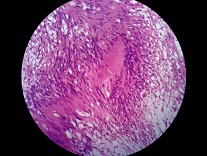
Figure 4- HPE of schwannoma: showing tumor composed of cellular Antoni A areas and Antoni B.
Immunohistochemistry (IHC) showed S-100 positive (3+) in >90% of cells suggestive of schwannoma (Figure 5). Postoperative period was uneventful and patient is doing well 1 year after surgery with no recurrence.
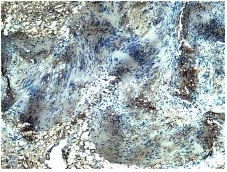
Figure 5- IHC showing S 100 positive
Case 2
24 year old male presented with an incidental mass in the retrorectal area which was detected by ultrasound following a trivial trauma to his abdomen. Abdominal findings were not contributory. Per rectal examination revealed a firm mass in the retrorectal area, lower border felt 5cm from anal verge, overlying mucosa was normal.MRI showed a heterointense lesion in the presacral region on the left side measuring 66 × 60 × 70 mm in T2 W images extending through the left S1 foramina causing widening of the foramen with anterolateral scalloping of S1 vertebra, lesion displacing the rectum right laterally (Figure 6).
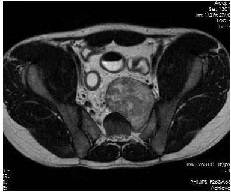
Figure 6-T2W axial MRI image - tumor heterointense. Extending into sacral foramen. Scalloping of vertebra seen
T1 W images showed a hypointense lesion (compared to muscle) (Figure 7) intensely enhancing Post-Gadolinium contrast (Figure 8). Peroperatively, there was a well encapsulated tumor of size 7×7 cm with no involvement of rectum or presacral fascia. It was posterior to presacral fascia which was incised and tumor was excised in toto. Postoperative period was uneventful with no neurologic deficit.Postoperative histology was suggestive of schwannoma and IHC showed S 100 to be positive. Patient is totally asymptomatic and tumor free 7 months after surgery.
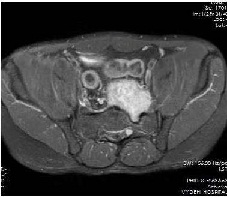
Figure 7-T1W axial MRI image -Post-Gadolinium-Intensely enhancing lesionextending into ipsilateral sacral foramen

Figure 8-T1W sagittal MRI image -Post-Gadolinium - intensely enhancing tumor
Discussion
Retroperitoneal tumors can be benign or malignant. The benign tumors may be of neurogenic origin like schwannoma, paraganglioma, ganglioneuroma or sacral meningioma, ependymoma, chordoma, chondrosarcoma, giant cell tumor, aneurysmal bony cyst, osteoblastoma, sacrococcygeal teratoma, desmoid tumors, leiomyoma or lymphomas [2]. Though they have different cells of origin, their biological behavior is almost the same.
Studies in the past in 1950’s and 1970’s have described a very low incidence of benigntumors (4-25%).Storm et al,reported that nearly half of the retroperitoneal tumors were sarcomas [3]. But with advanced diagnostic modalities, number of incidentally detected benign tumors have increased &incidence is reported as high as 60% in some series.1
Retroperitoneal space is expansive. So, tumors grow to a very large size,displacing adjacent structures before producing symptoms. Symptoms range from vague abdominal pain to atypical symptoms like flank pain, hematuria, recurrent renal colic pain, headache, secondary hypertension [4].
Schwannomas are nerve sheath tumors, common in 4th to 6th decade of life withmale:female ratio of 2:3 [4]. Majority are solitary [5] 0.5-5% of schwannomas occur in the retroperitoneum, accounting for 0.5-12% of all retroperitoneal tumors [4].
Malignant transformation occurs only in 0.7 to 2.6% of retroperitoneal schwannomas [6]. But in Von Recklinghausen’s disease malignant schwannomas aremore common and occurs in 5% to 18 % of cases [2].
Histopathology of schwannomas consists of compact cellular areas (Antoni A) along with loose hypocellular myxoid stroma with microcystic spaces (Antoni B). Malignant schwannomas are characterized by high mitotic index, cellular pleomorphism and vascular and adjacent tissue infiltration. They behave like high grade sarcomas with local recurrence and distal metastasis. Immunohistochemistry is important for confirmation of diagnosis and also for ruling out malignancy. In Schwannomas there is a diffuse positivity for S 100 protein in cytoplasm of these cells.Vimentin is used as a sarcoma tumor marker to identify mesenchymal tissue.
Schwannomas of long duration undergo fatty degenerative changes and with diffuse areas of hypocellularity are termed ancient schwannomas [7].
Investigations like ultrasound abdomen help detect these masses, which show their homogenous or heterogenous echotexture. But investigatory modalities like CT and MRI help not only in detection, but also show tumor characteristics which help in diagnosis, determine operability and planning treatment. On CT scan, well delineated tumors with areas of calcification, no involvement of adjacent organs, absence of lymph nodes and metastasis suggest a benign nature. Most incidental tumors are benign. Retroperitoneal schwannomas appear as well-delineated round or oval masses with punctate or mottled calcification and cystic degeneration on CT scan [4].
J.Nakashima et al, [1] have shown that large tumors (>5.5 cm), presence of symptoms, no calcification and cystic degeneration are indicators of malignancy. Calcifications were reported in 7 of 15 benign cases and in none of the malignant ones. But Stephen
et al, [8] have reported calcifications in malignant fibrous histiocytoma and recurrent liposarcoma.
But in our patient with schwannoma, tumor was of larger size, symptomatic with cystic degeneration, still benign. Retroperitoneal shcwannomas have high chances of cystic degeneration [9]. Cystic degeneration occurs when tumor outgrows its blood supply and will not always indicate malignancy. Though CT is useful, MRI is the diagnostic modality of choice for evaluating retroperitoneal tumors. In schwannomas, masses appear as low signal intensities on T 1 weighted images and high signal on T 2 weighted images. But this is not specific as it is found in other neurogenic tumors like ganglioneuromas also. Depending on the cell density, the signal intensity on T2-weighted images may vary. Tumors with microscopic findings of hypercellular Antoni type A tissue have intermediate signals, while tumors with Antoni type B tissue have a bright signal on T2-weighted images.
But site of origin may not be accurately determined by imaging.In our patient as pancreas was not separately visualized, a preoperative diagnosis of pancreatic neoplasm was made. But peroperatively pancreas was free and pushed up.Schwannomas can also mimic an adrenal tumor [9] or as hepatic tumors or psoas abscess [4]. A schwannoma in a similar location as our second patient was reported to be of mesorectal origin [10].
CT guided biopsy or FNAC is not recommended as representative viable tissue may not be available and degenerative areas may be misdiagnosed as malignancy. Tumor seedling, risk of hemorrhageand infection is also feasible [4]. So, histological diagnosis should be made only after total excision of tumor.
Angiography used to be done in the past but degree of vascularity does not correlate with malignancy [1]. Haemangiopericytomas are very vascular tumors.
Ideal treatment of choice is complete excision of the tumor with negative margins.If intra operatively it is adherent to adjacent organs, role of enmassexcision is controversial.Some [9] believe that as malignancy is rare in retroperitoneal schwannomas, it is not necessary. But as malignant degeneration is possible, and incidence is more in Von Recklinghausen’s disease (5% to 18 % of cases) [2] and as a possibility of malignancy cannot be ruled out based on either preoperative imaging or by frozen section we feel that a radical excision is needed if adherent to adjacent organs. The possibility of recurrence also necessitates this. Incomplete excision always leads to recurrence and should be completely avoided.
Laparascopic excision has been tried in small tumors with good results [2 6]. It is useful if total excision of tumor is feasible with no tumor spillage and has less morbidity and helps early recovery. Partial excision or intralesional enucleation and tumor spillage leads to local recurrence in about 16-54 % of patients and should be completely avoided [4 6].
Conclusions
Massive size of retroperitoneal tumors is often misleading regarding both site of origin of tumor and the benign or malignant nature of it. Preoperative imaging will not always give a clue to the nature or cell of origin and so preoperative diagnosis is not always possible. CT guided biopsy should never be done. Histology and immunohistochemistry are required for definite diagnosis postoperatively. But complete excision of tumor without spillage gives excellent results and should always be attempted.
Learning points
-
Retroperitoneal tumors can grow to a large size before they become symptomatic.
-
Incidental tumors are increasing due to improving imaging modalities.
-
Different histological types occur but symptoms produced depend on the site, size of tumor and infiltration of adjacent tissue in malignancy.
-
Benign schwannomas are smaller with areas of calcification.
-
MRI is the imaging modality of choice for these tumors. It shows the site, size, adjacent organ involvement (T1 W) and muscles infiltration (T2 W).
-
CT guided biopsy is contraindicated due to fear of hemorrhage, infection, tumor dissemination and inadequate sampling.
-
Postoperative histology and immunohistochemistry are final markers of diagnosis.
-
Total excision of tumor with negative margin is the treatment of choice in benign retroperitoneal tumors and results are excellent.
Ethical considerations
An informed written consent has been obtained from both the patients.
Conflicts of Interest
The Authors declare no competing interests or conflict of interests
Authors' contributions
VYC conceived the study, participated in design, carried out literature search, performed the analysis and edited the final manuscript.
KNP carried out literature search, helped prepare draft manuscript
PSR carried out literature search, helped prepare draft manuscript
All authors read and approved the final manuscript for submission.
Acknowledgements
Dr.Rohini A,Assistant Professor in Dept. of Radiology and Dr.Sumana, Professor in Dept. of Pathology, for their valuable contribution for reviewing CT and MR images and reviewing histology slides respectively.
References
[1].Nakashima J, Ueno M, Nakarnura K, Tachibana M, Baba S, Deguchi N et al. Differential Diagnosis of Primary Benign and Malignant Retroperitoneal Tumors. Int J Urol 1997; 4:441-446 [Pubmed]
[2].Retroperitoneal Schwannoma: A Case Report and Review of The Literature. Journal of Neurological Sciences (Turkish). 2010; 27(3):353-358. [Pubmed]
[3].Storm FK, Mahvi DM. Diagnosis and management of retroperitoneal soft-tissue sarcoma. Ann Surg. Jul 1991; 214(1): 2–10. PMC1358407 [Pubmed]
[4].Cury J, Coelho R F, Srougi M. Retroperitoneal schwannoma: case series and literature review. CLINICS 2007; 62(3):359-62. PubMed PMID: 17589680.[Pubmed]
[5].Hughes MJ, Thomasb JM, Fisher C, Moskovic EC. Imaging features of retroperitoneal and pelvic schwannomas. Clinical Radiology. 2005; 60:886–893 [Pubmed]
[6].Okuyama T, Tagaya N, Saito K, Takahashi S, Shibusawa H, Oya M. Laparoscopic resection of a retroperitoneal pelvic schwannoma. Journal of surgical case reports. 2014(1). DOI: 10.1093/jscr/rjt122 [Pubmed]
[7].Yoshino T, Yoneda K. Laparoscopic resection of a retroperitoneal ancient schwannoma: a case report and review of the literature. Anticancer Res. 2008 Sep-Oct; 28(5B):2889-91. PubMed PMID: 19031930 [Pubmed]
[8].Stephens DH, Sheedy PF, Hattery RR, Williamson B. Diagnosis and Evaluation of Retroperitoneal Tumors by Computed Tomography. Am J Roentgenol. September 1977; 129:395-402.[Pubmed]
[9].Brian KP, Yu-Meng Tan, Yaw-Fui A. Chung, Pierce KH, London L.P.J. Ooi, Wai-Keong Wong et al. Retroperitoneal schwannoma. The American Journal of Surgery 192 (2006) 14–18.
[10].Jayprakash G, Yong C, Yanqing W. A case report of a Giant Schwannoma of the Mesorectum. British Journal of Medical Practitioners. 2009;2(3): 51-53.


