Case Report

Nasopharyngeal Carcinoma with Atypical Ophthalmic Presentation- A Rare Case Report
1 Shaqul Qamar Wani, 2 Talib Khan, 3 Saiful Yamin Wani, 1 Arshid Manzoor Najmi, 1 Tariq Rasool Malik, 1 Mohamad Maqbool Lone, 1 Fir Afroz.
- 1 Department of Radiation Oncology, Sher - I - Kashmir Institute of Medical Sciences, Srinagar, Jammu and Kashmir, India- 190011.
- 2 Department of Anaesthesiology, Pain and Critical Care, Sher - I - Kashmir Institute of Medical Sciences, Srinagar, Jammu and Kashmir, India- 190011
- 3 Directorate of Health Services Kashmir, Srinagar, Jammu and Kashmir, India- 190001.
- Submitted: January 29, 2015
- Accepted: March 15, 2015
- Published: May 17, 2015
This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/3.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited
Abstract
Introduction
Nasopharyngeal carcinoma (NPC), a rare malignancy with unique and complex etiology, is most confused and commonly misdiagnosed disease and can present as painless enlargement of upper neck nodes, followed by nasal, aural, ophthalmic, neurological manifestations.
Case presentation
We present a case of NPC in a 24 year old unmarried female, who initially presented with painless bilateral loss of vision, initially treated empirically for optic neuritis and Tuberculosis for four years.
Conclusion
Isolated painless and bilateral loss of vision though unusual and rare manifestation of NPC should be considered as a possible differential.
Key words
nasopharyngeal carcinoma, bilateral loss of vision, optic neuritis, paraneoplastic effect, ophthalmic presentation.
Introduction
Nasopharyngeal carcinoma (NPC) is a rare malignancy with unique and complex etiology. NPC is one of the most confusing, commonly misdiagnosed, and poorly understood diseases. NPC has a remarkable racial and geographical distribution [1, 2]. NPC has attracted world-wide attention because of complex interactions of genetic, viral, smoking, environmental, dietary factors, occupational etc., which have been implicated in causation of NPC [1- 9].
The clinical presentations of NPC may sometimes be insidious and nonspecific. They are usually related to the local, regional and distant spread or metastasis of the lesion. They may include cervical lymphadenopathy, nasal blockage, epistaxis, hyponasal speech and otologic and neuro-ophthalmic manifestations [2, 10]. The clinical morphology may be infiltrative, ulcerative or exophytic [10]. The neuro-ophthalmic manifestations present usually late with the advancement of disease. Ophthalmic manifestations of NPC include ocular motility problems (cranial nerve involvement), blurred vision, proptosis, orbital pain, and optic disc edema [11]. Loss of vision as initial presentation is very rare and can be optic neuritis or/ as paraneoplastic manifestation of NPC [12, 13].Here we present a case of NPC with atypical neuro-ophthalmic presentation misdiagnosed for four years.
Case Presentation
We present a 24 year old Asian female student presented with acute diminution of vision in both eyes 4 years back followed by complete loss of vision one year later in both eyes. There was no history of pain, redness in eyes, headache, blurring of vision, double vision, and inability to move eyeballs. Magnetic resonance imaging (MRI) of brain revealed normal study (Figure 1) and patient was started on intravenous methylprednisolone 1gram for three days followed by tapered dose of prednisolone but with no improvement in vision.
Repeat MRI another six month later again revealed normal study (Figure 2) and patient continued on steroids and multivitamins without any benefit. Another MRI four months later showed localized enhancement of left optic nerve and cavernous sinus (Figure 3), followed by another MRI two months later which gave the impression of bilateral cavernous sinus infiltration and orbital apex syndrome (OAS) with left optic neuritis (Figure 4). The patient was continued on steroids. Another six months later MRI revealed peri-optic enhancing soft tissue involving optic nerve up to the optic chiasm, likely possibility of granulomatous etiology (likely Sarcoidosis, Wegener’s Granulamatosis or Tuberculosis). Cerebrospinal fluid (CSF) analysis and chest roentgenogram (CXR) were normal. Rheumatoid factor (RF), anti-nuclear antibody (ANA), C - reactive protein (CRP) profile was negative. Ultrasonography (USG) evaluation of abdomen and pelvis was normal. She was put on anti-tubercular treatment for six months in view of MRI showing granulomatous lesion (likely tubercular) in bilateral optic canal. Nasopharyngeal biopsy revealed nasopharyngeal granular lesion.
Figure 1- MRI Brain and Orbit showing normal study
Figure 2- MRI Brain and Orbit showing Normal Study
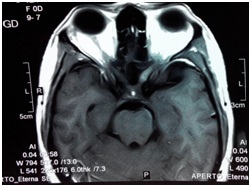
Figure 3 MRI showing localised enhancement of left optic nerve (ON) and cavernous sinus (CS)
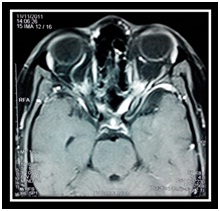
Figure 4- MRI showing Bilateral cavernous sinus (CS) infiltration and orbital apex syndrome (OAS) with left optic neuritis (ON)
Contrast enhanced (CE) MRI another six month later gave the impression of bilateral bulky cavernous sinus with diffuse enhancing cavernalduralpachymeningeal thickening seen extending upto orbital apex, features suggestive of infective etiology likely tubercular pachymeningitis. Repeat biopsy nasopharynx was suggestive of sarcoma possibly rhabdomyosarcoma and was started on adriamycin and ifosfamide based chemotherapy. Positron emission tomography – computed tomography (PET-CT) using fluorodeoxyglucose (FDG) radiotracer, revealed FDG avid thickening in nasopharynx, with mild FDG avid sclerotic metastasis involving clivus, cervical vertebrae and upper thoracic vertebrae. Non-FDG avid meningeal enhancement in cavernous sinus extending into bilateral orbital apices. Repeat nasopharyngeal biopsy revealed tumor composed of malignant epithelial cells. Immune histochemistry (IHC) was cyto keratin positive and leukocyte common antigen (LCA) and CD profile for lymphoma was negative confirming the diagnosis of NPC. Patient was advised but refused to undergo EBV DNA levels in view of terminal illness. She is presently on palliating treatment.
Discussion
The NPC is a rare malignancy worldwide, the most confusing, commonly misdiagnosed, and poorly understood disease [2]. The ophthalmic manifestation as only or the first symptom is very rare in NPC at presentation [14]. Similarly the isolated optic nerve involvement is rare [14] but usually indicates cavernous sinus invasion [8, 9, and 14]. The ophthalmic involvement though not uncommon in patients with nasopharyngeal carcinoma in the late stages of disease [13] but isolated optic nerve involvement is rarely reported as an initial manifestation [13, 15]. The patients with the orbital or ocular manifestations also have lesser survival and poor prognosis [11]. The sudden onset of painless monocular blindness can be the initial manifestation of a NPC [16], but in our case, patient had acute and painless bilateral loss of vision.
The optic neuritis with sectorial field loss as a remote effect of NPC likely paraneoplastic effect as there was neither any tumor mass around the optic nerve nor any histological evidence of tumor infiltration [12].
The most common pathway of NPC spread as orbital invasion are through pterygopalatine fossa and inferior orbital fissure, followed ethmoid and/or sphenoid sinuses as can be seen best by Coronal sections on CT or MRI [5, 9, 7, 11, 17]. NPC can invade orbital apex and can present as OAS and the causes can be inflammatory, infectious, neoplastic, iatrogenic/ traumatic, or vascular processes [18, 19].
Conclusions
The present case description emphasizes that acute painless bilateral loss of vision can be a rare and unusual initial manifestation of NPC. The present report suggests that NPC can present as retrobulbar/optic neuritis with initial negative radiological findings most likely due to its paraneoplastic effect. In order to reduce the delay in diagnosis, the patients presenting with acute painless loss of vision should be ruled out for NPC.
Ethical Considerations
Written informed consent was obtained from the patient for the publication of this case report and accompanying images.
Conflict of Interest
The authors declare no conflict of interest.
Author’s contributions
SQW prepared and approved the manuscript, TK approved final manuscript, SYW also helped in writing manuscript, AH, and TRM, MML, and FA did the literature search and prepared the draft manuscript.
All authors read and approved the final manuscript.
Funding
None
Acknowledgement
None
References
[1].Chang ET, Adami HO. The enigmatic epidemiology of nasopharyngeal carcinoma. Cancer EpidemiolBiomarkers Prev2006; 15:1765-77 [Pubmed]
[2].Kumar S. Epidemiological and etiological factors associated with nasopharyngeal carcinoma. ICMR Bulletin 2003;33.http://icmr.nic.in/busept03.pdf [Last accessed on May 17, 2015]
[3].Wani SQ, Khan T, Lone MM, Afroz F, Khan NA.Nasopharyngeal carcinoma: An 11 year study with respect to patient characteristics, clinical aspects and staging at presentation. J Cancer SciTher 2014, 6:9 http://omicsonline.org/1948-5956/1948-5956.S1.037_005.pdf Abstract presented at Global Cancer Conference &Medicare Summit, Hyderabad, September 15-17, 2014.
[4].Brennan B. Nasopharyngeal carcinoma. OrphanetJRare Dis 2006;1:23.http://www.ojrd.com/content/pdf/1750-1172-1-23.pdf [Pubmed]
[5[.Hu KS, Chan ATC, Costantino P, Harrison LB. Cancer of the nasopharynx. In: Harrison LB, Sessions RB, Hong WK, editors. Head and neck cancer: a multidisciplinary approach. 3rd ed. Philadelphia: Wolters Kluwer/ Lippincott Williams &Wilkins 2009 p. 502-43.
[6].Rubin P, Hansen JT. Nasopharynx. In: Rubin P, Hansen JT, editors. TNM staging atlas with oncoanatomy. 2nd ed. Philadelphia: Wolters Kluwer/ Lippincott Williams &Wilkins 2012 p. 42-51.
[7].Chan SH.Etiology of nasopharyngeal carcinoma. Ann Acad Med Singapore. 1990 Mar; 19(2):201-7.[Pubmed]
[8].Lee AWM, Perez CA, Law SCK, Chua DTT, Wei WI, Chong V. Nasopharynx. In: Halperin EC, Perez CA, Brady LW, Editors. Perez and Brady's Principles and Practice of Radiation Oncology. 5th Ed. Chapter 38; Philadelphia: Wolters Kluwer/ Lippincott Williams &Wilkins. 2008
[9].Mendenhall WM, Werning JW, Pfister DG. Cancer of the Head and Neck. In: DeVita VT, Lawrence TS, Rosenberg SA, Editors. DeVita, Hellman &Rosenberg's Cancer: Principles &Practice of Oncology, 8th Ed. Vol 1, Chapter 36; Philadelphia: Wolters Kluwer/ Lippincott Williams &Wilkins. 2008
[10].Daniel A, Fasunla AJ. Nasopharyngeal cancer mimicking otitic barotrauma in a resource - challenged center: a case report. J Med Case Rep. 2011 Oct 31; 5:532. doi: 10.1186/1752-1947-5-532.[Pubmed]
[11].Hsu WM, Wang AG. Nasopharyngeal carcinoma with orbital invasion. Eye 2004; 18:833–8 [Pubmed]
[12].Hoh ST, Teh M, Chew SJ. Paraneoplastic optic neuropathy in nasopharyngeal carcinoma--report of a case.Singapore Med J 1991; 32:170-3[Pubmed]
[13].Tsai CC, Ho HC, Kau HC, Kao SC, Hsu WM. Optic neuritis: a rare manifestation of nasopharyngeal carcinoma. Eye 2002; 16:501-3 [Pubmed]
[14].Lee AWM, Foo W, Law SCK, Poon YF, Sze WM, O SK, Tung Y, Lau WH. Nasopharyngeal carcinoma: Presenting symptoms and duration before diagnosis. Hong Kong Med J 1997; 3:355-61.[Pubmed]
[15].Park KA, Oh SY. Nasopharyngeal carcinoma presenting with rapidly progressive severe binocular optic neuropathy and periocular pain in a young man. Journal of Neuro-Ophthalmology 2010; 30:150-2 [Pubmed]
[16].Carlin L, Biller J, Laster DW, Toole JF. Monocular blindness in nasopharyngeal cancer. Arch Neurol 1981; 38:600 [Pubmed]
[17].Luo CB, Teng MM, Chen SS, Lirng JF, Guo WY, Chang T. Orbital invasion in nasopharyngeal carcinoma: evaluation with computed tomography and magnetic resonance imaging. Zhonghua Yi XueZaZhi (Taipei) 1998; 61:382-8.[Pubmed]
[18].Aryasit O, Preechawai P, Aui-Aree N. Clinical presentation, etiology and prognosis of orbital apex syndrome. Orbit 2013; 32:91-4. [Pubmed]
[19].Yeh S, Foroozan R. Orbital apex syndrome.CurrOpinOphthalmol 2004; 15:490–8.[Pubmed]


