Original Article

Cerebral Candiasis
*Vivek Sharma(M.Ch.), *Divye Prakash Tiwari(M.Ch.) *Janak Raj(M.S.)
- *Department of Neurosurgery, Institute of Medical Sciences, Varanasi, India
- Sunday, October 13, 2013
- Thursday, October 31, 2013
- Saturday, November 02, 2013
This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/3.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Introduction
Cerebral candiasis is not commonly seen in live patients but it is observed in autopsy. It has more preponderance in immunocompromised patients either suffering from AIDS or on steroid therapy.It is very rare in healthy individual.There is strong suspicion of brain lesion as fungal if adjoining paranasal sinus is involved. Treatment includes decompressive surgery followed by Amphotericin.
Methods
All cases with proven diagnosis in last 20 years were taken into consideration. They were analysed in respect of age, sex, clinical feature, radiological feature, surgery and final outcome.
Results
There were 10 histologically proven cases of Cerebral Candiasis with male predominance. The most commonly affected age group is 40 to 50 years. AIDS was present in 3 cases while three patients were immunocompromised.
The Frontal lobe was involved in 90% as it was near to ethmoid sinus, which was initial site of affection. The seizure was manifesting symptom. Decompression was done 6 cases while diagnostic biopsy in 4 cases. Long term outcome was unsatisfactory because of underlying cause.
Key Words
Candiasis, cebebral candiasis, Fungal granuloma, AIDS
Introduction
Candida albicans is atrue yeast and a normal constituent of the human flora. Most of the patients with cerebral Candiasis are not recognized until post mortem examination [1]. This fungus is present normally in gastrointestinal tract and can invade tissues when overwhelming numbers are present. Deep Candiasis affects the kidney (80%), brain (50%) and heart (40%) but no tissue is exempted [2]. In most of the cases infection is opportunistic and is found in association with surgery, immunosuppression, prolonged antibioticusage, drug abuse or AIDS [3]. It is also common in preterm neonates or neonates with congenital or acquired AIDS [4].It is emphasized that cerebral mycosis should always be considered when neurological symptoms were clinically observed in patients who had severe underlying diseases with severe lymphocytopenia [5]. Infection in previously healthy individual is very rare.
Patients and Methods
All cases with histologically proven in last 20 years were taken into study. Their age, sex, clinical picture, associated disease, immunological status and radiological finding were collected and analysed. Their outcome were assessed in view of surgical & medical management.
Results
Ten patients ranging from 30-50 years who had histologically proven, were managed. Male and female ratio was 3:2. The most common age group was 40-50 years of age table 1.
| Age |
Sex |
Incidence |
| 20-30 |
Male Female |
0
0
|
| 30-40 |
Male Female |
2 (20%)
2 (20%)
|
| 40-503 |
Male Female |
4 (40%)2 (20%) |
Clinical Feature
The most common presentation was generalized tonic-clonic seizure which was found in all cases. The hemiparesis was noted in 2 cases. There was revised intracranial pressure with papilloedma in 2 cases. The history of nasal discharge was present in 2 cases table 2..
| Symtoms/SignsN |
Number of patients |
| Seizure1 |
10 |
| Raised Intracranial Tension |
4 |
| Hemiparesis |
2 |
| Papilloedema |
4 |
| Nasal Discharge |
6 |
| Behaviour Disorder |
2 |
Radiology
Either Computed Tomography or Magnetic Resonance Imaging with Contrast was done in all cases. Ethmoidal sinus was affected in four patients. Lesion was hypo to iso intense with with irregular enhancement. Most patients had no significant mass effect table 3.
| Location |
Number of patient |
| Frontal |
| Unilateral |
7 |
| Bilateral |
2 |
| Temporal |
1 |
The six out of ten patients had compromised immunological status. Three patients HIV positive and three were on chronic steroid therapy. There were two patients who were not associated with other co-morbid condition table 4.
| Feature |
Number of Patients |
| AIDS |
3 |
| Chronic Corticosteriod therapy |
3 |
Treatment
All patients underwent either diagnostic or therapeutic surgery. Lesion was diffuse and relatively avascular adhered to dura and sinus at base. All patients received medical treatment by Amphotericin B with careful watch on renal and bone marrow function
Outcome
Mortality was high (60%) in immunocompromised patients within one year while rest two developed significant recurrence four years later and expired 4 years later.
Illustrative Case 1
History: A 38 years right handed male, carpet weaver from India presented with complaints of headache, vomiting and convulsion since 10 months. Headache was of gradual onset, progressive in nature initially diffuse and global but later localized to forehead, severe in intensity and intermittent. Vomiting was spontaneous and projectile, 1-2 hour after beginning of headache. Convulsions were of generalized type with preictal aura or post ictal palsies. There has been no other associated history except mild watering of right eye due to involvement of paranasal sinus. He was not drug addict. There was no history of symptoms which would suggest diabetes, hypertension, leukemia, lymphoma or immunocompromised status. There was no history of extra marital contact.
Examination: General examination was normal with no sign of meningeal irritation. Chest, cardiovascular, abdomen, scalp and spinal examination was inconclusive. Patient was conscious with normal higher mental function, intelligence, speech and reasoning. Patient had right anosmia and bilateral papilloedema. Motor and sensory systems including bladder and bowel control were normal. Abnormal glabellar & palmomental reflexes were present all superficial and deep tenden jerks were normal without gait abnormality.
Management: The X-ray chest and ELISA for HIV was negative. Computed Tomography scan was negative. CT scan head (plain and contrast) showed a large hypodense poorly enhancing lesion in right frontal region compressing the right lateral ventricle with midline shift with obliteration of sulci. Posterior group of right ethmoidal air sinus was opacified with erosion of bony ethmoidal roof Figure 1
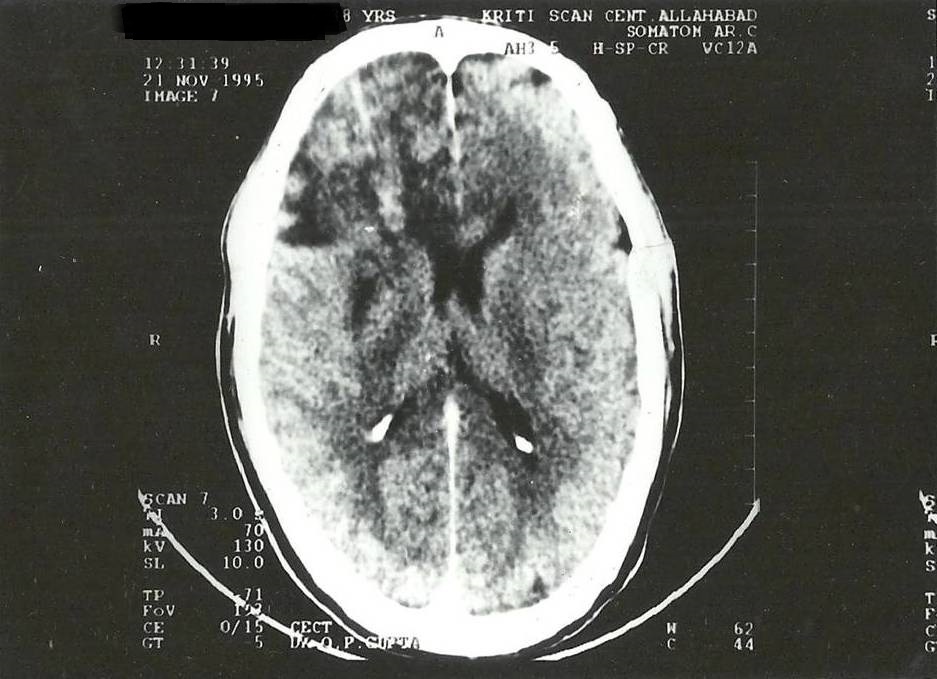
Figure 1: CT Axial Section showing frontal lesion
Histopathological examination of ethmoidal biopsy of right posterior ethmoid sinus proved ill defined epitheloid granulomas with multinucleate/histocytic gaint cell with mixed inflammatory cell infilterate along with multiple fragments of fungal hyphal elements suggestive of fungal granuloma.Patient was subjected to classical right frontal lobectomy. The lesion was avascular ill defined diffuse infilterating growth of variable consistency (jelly-like to hard).Right olfactory nerve was involved in process but continuation between ethmoid sinus and frontal lobe could not be confirmed, and ventricle was free of pathology. Histopathogical examination was of a granulomatous process containing
well marked cellular collection madeup of lymphocytes, plasma cells and multinucleate giant cells with presence of organism in the form of yeast and hyphal structure suggestive of candida. More over marked vasculitis with resultant thrombosis and whit matter infarct where also seen Figure 2. Culture grown from biopsy specimen showed candida species. Post operative period was uneventful with normal mentation without neurological deficit. Patient was put on Amphotericin-B.
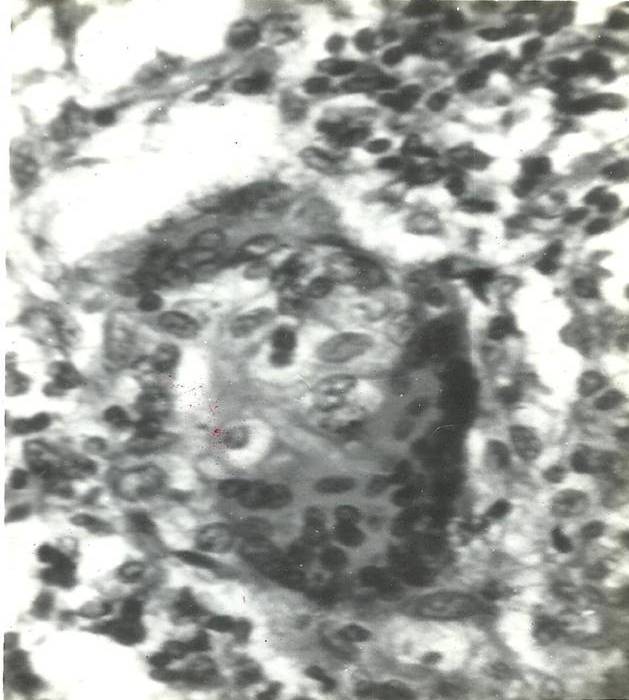
Figure 2: Microhistolopathology of excised lesion
Illustrative case 2
History: A 46 year old male patient, labourer by occupation admitted with complaints of recurrent fit and recovered on antiepileptic treatment. He was known case of AIDS.
Examination: Neurological examination was normal.
Investigation: MRI showed multiple enhancing ring like lesions in frontal lobe with reactive oedema extending to opposite cerebral hemisphere and involving ethmoid sinus Figure 3.

Fig.3: Coronal view of Contrast MRI exhibiting lesion in frontal lobe involving ethmoid sinus
Treatment: Frontal craniectomy followed by decompressive surgery was done. Lesion was avascular with variable consistency. Histopathological examination was suggestive of Candiasis Figure 4.

Figure 4: Micro-histopathological photograph of excised lesion
Discussion
Candida has emerged as one of the common pathogen in patients with serious underlying disorders. This has been notable in patient with narcotic addiction, immunosuppressive therapy, prolonged antibiotic treatment and intravenous catheter [5,6]. Bayer reported that Candiasis of central nervous system may present as meningitis granuloma or as an abscess [7]. Gould PR noted that Candida granulomas are multiple and commonly located at the junction of gray and white mater [8]. Extra cranial focus of infection was present in 70% [3]. Present study showed ethmoidal fungal granuloma in 60%. Although the candida meningitis can be diagnosed by lumbar puncture and by analysis of CSF but the mass lesion needs CT Scan or MRI for the diagnosis. Marcinkowski M et al suggested that in neonates with systemic fungal infection the brain imaging with sonography should be considered as bed side investigation [4].Treatment is removal ofsource of infection at the earliest with control or stabilization of the underlying debilitating disease if present. The treatment should be given with Amphotericin –B [9]. Ferrari P et al also reported the successful treatment of low birth weight babyu with cerebral fungal granuloma liposomal amphotericin B without recurrence upto 7 years followup [10].
Authors' Contributions
VS: Concept of study and final approval
DPT: Concept and analysis of study, literature search and preparation of manuscript
JR: Concept and design of study
Conflict of Interest
The authors declare that there are no conflicts of interests
Ethical Considerations
Written informed consent was taken from the patients for
publication of this case report
Funding
None
References
[1].Carey ME. Infections of the spine and spinal cord. In: neurological Surgery, Youmans JR, WB Saunders Company,1990: 3769
[2].Joseph C Parker, Michrel l Dyer. Neurological Infections due to Bacteria, Fungi and Parasites.In: Text book of Neuropathology, Richard L David David M.Robertson Williams and Williams Company. Baltimore,USA.1988: 662-703
[3].Manoj K Bhattacharya, Bhattacharya A, Sridhar K. Fungal Infections. In: Text Book of Neurosurgery, B Rammamurthi, PN Tandon. B.I.Churchill Livingstone. New Delhi India 1996: 553-565
[4].Marcinkowski M, Bauers K, Stoltenburg-Didinger G, Versmold H.Fungal brain abscesses in neonates: Sonographic appearance and correshistopathologic findings.J Clin Ultrasound.2001;29(7):417-21.[pubmed].
[5].Abe F,Nakamura N, Ommura Y. A pathological study on cerebral mycosis. No To Shinkei.1982;34(12):1169-74.[pubmed].
[6].L.Tveten. Candidiosis .In: Handbook of Clinical Neurology Vol.35 (ed) PJ Vinken and Gin Bruyn North Holland Publishing Company, Amsterdam Netherland 1978:413-442.
[7].Parker JC Jr, McCloskey JJ, Lee RS.Human cerebral candidosis --a postmortem evaluation of 19 patients. Hum Pathol. 1981;12:23-8.[pubmed].
[8].Gould PR, Gould IM. Cryptococcosis in Zimbabwe. Trans R Soc Trop Med Hyg. 1985;79:67.[pubmed].
[9].Sanchez Portocarrero J, Perez-Cecilia E, Corral O,Romero-Vivas J,Picazo JJ. The central nervous system and infarction by Candida species. Diagmn Microbiol Infect Dis.200;37(3):169-79. [pubmed].
[10].Ferrari P, Chiarolanza J, Capriotti t, Garetti E, Venuta A. Favorable course of cerebral candidiasis in a low-birth newborn treat liposomal amphotericin B. Pediatr Med Chir. 2001;23(2-3):197-9[pubmed]

