Research

Primary Intracranial Hydatid Cysts: Review of Ten Cases
Ravi Shankar Prasad, Kulwant Singh, Vivek Sharma
- Department of Neurosurgery, Institute of Medical Sciences Varanasi-221005, India
- Submitted: December 23, 2012;
- Accepted: January 11, 2013
- Published: January 17, 2013
This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/3.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Introduction
Intracranial hydatid cyst is a rare disease, with reported incidence of 1-2% of all cases with hydatid disease. Hydatid disease is caused by infestation of larvae of Taenia echinococcus. Cerebral hydatid disease is more common in pediatric population but all patients in the present series were adults. The features of this disease are retrospectively analyzed in this presentation and the literature is reviewed.
Material and Method
The present study is a retrospective analysis of ten cases of intracranial hydatid cysts managed at SS Hospital BHU, Varanasi during 2009-2012. A detailed recording was made of the presenting features, neurological signs, investigations, type of surgery and outcome.
Results
All patients presented with focal neurological deficit, seizure, and features of raised intracranial pressure, or brain stem compression. The mean age of presentation was 27 years. Radiological investigation was CT scan in nine cases and MRI was done in one case only. Four patients had multiple intracranial cysts while six had solitary cysts. In four cases cyst was located in parietal lobe out of which two were multiple, one was in suprasellar region, two in frontal region, one in the third ventricle, one in interhemispheric region which was multiple and one had multiple cysts occupying frontal, deep parietal and in posterior fossa of brain. Total excision of cyst was done in all the cases.
Conclusion
Intracranial Hydatid Cysts though rare but seen even in adults. A high index of suspicion and proper management can prevent life threatening consequences.
Key words
Hydatid, Intracranial, Cyst.
Introduction
Hydatid disease is caused by infestation of larvae of Taenia echinococcus. The definitive hosts of echinococcus are various carnivores, the common being the dog. All mammals (more often being sheep and cattle) are intermittent hosts. Humans get infected through the faeco-oral route by ingestion of food or milk contaminated by dog faeces containing ova of the parasite or by direct contact with dogs. The eggs loose their enveloping layer in the stomach, releasing the embryos. The embryos pass through the wall of the gut into the portal system and carried to the liver where most larvae get entrapped and encysted. Some may reach the lungs and occasionally, some may pass through capillary filters of liver and lungs and get entry into systemic circulation. These may even reach the brain. Various cases of intracranial hydatid cyst have been reported but this study includes cases at different uncommon sites of which mode of presentation, radiological features, treatment and outcome have been discussed and relevant literature is reviewed.
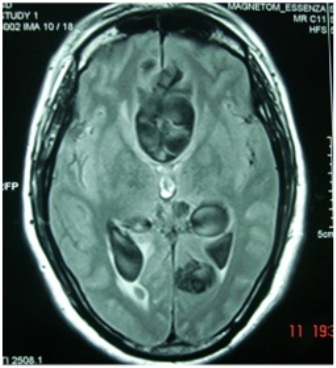
Figure-1: Multiple interhemispheric cysts.
Material and methods
We retrospectively analyzed ten cases of intracranial hydatid cysts managed at SS Hospital BHU, Varanasi during 2009-2012. A detailed recording was made of the presenting features, neurological signs, investigations, type of surgery and outcome.
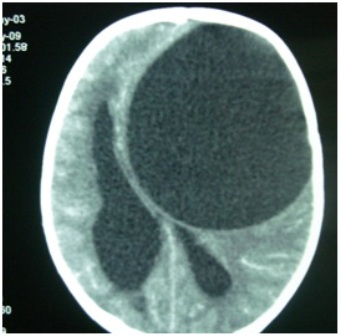
Figure-2: Large single cyst.
Results
Ten cases of intracranial hydatid cysts treated during the period of 2009-2012 at SS Hospital BHU represent an incidence of 2% of all space occupying lesions operated during this period (Table 1). The mean age of presentation was 28 years. The male to female ratio was 7:3. In three cases only, history of pet dogs was found. Eight were from rural background and two were from urban areas. The duration of symptoms varied from one month to one year. The clinical features are described in the table 1. These varied according to the location of cyst in the brain and its size. Headache was the commonest presentation; seizure was present in four cases. Papilloedema was seen in five cases. Two patients were blind. One patient with multiple cysts presented in emergency in unconscious state due to a cyst in posterior fossa which was compressing brain stem. CT scan was done in nine cases and MRI was done in one case. Four had cyst in parietal lobe out of which two were multiple, one in interhemispheric region which was multiple (Figure 1), two cases of huge cyst in frontal (Figure 2) one small cyst in third ventricle which was producing hydrocephalus and one in the suprasellar region (Figure 3). One patient had multiple cysts including in frontal, deep parietal and in posterior fossa (Figure 4). USG abdomen and X-ray chest was done in all the cases but failed to reveal any associated hydatid cyst in lung and abdomen. In all the cases total excision were done including the four with multiple cysts. Only in one case of multiple parietal cysts, rupture occurred while delivering the cyst (Figure 5) and in the rest six cases cysts were excised in toto (Figures 6). The large cysts in frontal region were excised by hydrodissection i.e., by gentle saline irrigation around the wall. The other seven were excised by gentle traction and dissection (Figure 7 and 8). The intraventricular small cyst was excised through endoscope. None of our patient has recurrence of intracranial hydatid disease till now as we do CT scan at six months intervals. All patients received albendazole in postoperative period.

Figure-3: Suprasellar cyst with deep sylvian extension.
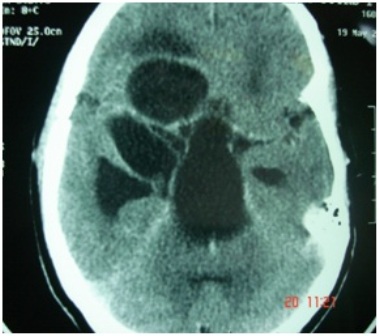
Figure-4: Multiple cysts .
Discussion
Intracranial hydatid cyst is a rare disease, with reported incidence of 1-2% of all cases with hydatid disease [1]. Hydatid disease is endemic in the middle east, Mediterranean countries, South America, North Africa and Australia [2]. Cerebral hydatid disease is more common in pediatric population [3, 4]. but all patients in the present series were adults. History of direct contact with dogs is available in only three cases, as infection can also be acquired by eating contaminated food and milk. In the present series, our patients belonged to eastern UP and Bihar who are very fond of chutney and salad which are uncooked food.

Figure-5: Multiple hydatid cysts.
Intracranial hydatid cysts are more frequently located in the supratentorial compartment. The parietal lobe is the commonest site and was seen in four cases in the present series. All four cases reported by Dharker et al., [5] and three out of five cases of intracerebral hydatid cysts reported by Balasubramaniam et al., [6] had parietal lobe involvement. The other less common sites reported are skull [6], cavernous sinus [7], eye ball [8], pons [9], skull [6], extradural [10], cerebellum and ventricles [4]. Solitary hydatid cyst in the third ventricle, as seen in one case in this study is a rare site for intracranial hydatid cyst. Also suprasellar and interhemispheric hydatid cyst are not reported till now. Hydatid cysts of posterior fossa are also rarely reported. The cerebral hydatid cysts are slow growing and present late when they increase in size and become large. In the present series also all the cysts were quite huge except the cyst in suprasellar region and the intraventricular one There is no consensus on the growth rate of the hydatid cysts of the brain and has been variably reported between 1.5-10 cm/year [3, 11].

Figure-6: Large hydatid cyst of brain.
Intracranial hydatid cysts are commonly solitary. Multiple intracranial cysts are rare. Onal et al., [2] found only three cases of multiple cysts in their series of 33 cases and Lunardi et al., [12] found 2 cases in their series of 12 cases. We also observed fairly high incidence of 40% (four out of ten cases) of multiple cysts in the present series.
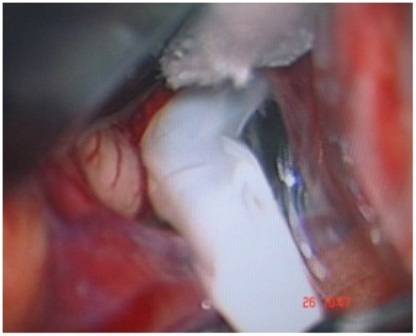
Figure-7: Delivery of a hydatid cyst.
Intracranial hydatid cyst may also be classified as primary or secondary. The primary cysts are formed as a result of direct infestation of the larvae in the brain without demonstrable involvement of other organs. In primary multiple cysts, each cyst has a separate pericyst with brood capsule scolices and these originate from multiple larvae affecting brain after crossing the gastrointestinal tract, liver, lungs and right side of heart without affecting them. The primary cysts are fertile as they contain scolices and brood capsules, hence rupture of primary cyst can result in recurrence. The secondary multiple cysts results from spontaneous, traumatic or surgical rupture of the primary intracranial hydatid cyst and they lack brood capsule and scolices. The secondary intracranial hydatid cysts are therefore, infertile and the resultant risk of recurrence after their rupture is negligible. Primary multiple cysts are uncommon and isolated case reports of primary multiple hydatid cysts have appeared in the literature [13, 14]. Nurchi et al., [13] while reviewing the literature found only eleven reported cases of primary multiple hydatid cysts. In the present series, we had four cases of primary multiple hydatid cysts two in parietal and one in interhemispheric region and one in multiple regions of brain including frontal, parietal and posterior fossa.
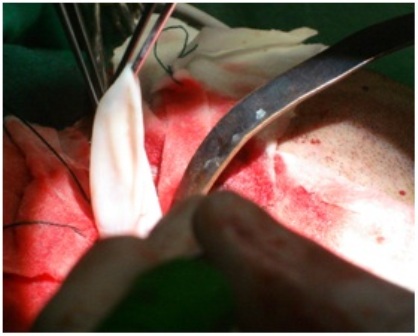
Figure-8: Excision of a hydatid cyst.
The patients with intracranial hydatid cysts usually present with focal neurological deficit and features of raised intracranial pressure; the latter may be due to the large size or due to interference with pathway of CSF flow. Erashin et al., [1] observed that 18 out of 19 cases presented with raised intracranial pressure. Four cases had convulsions. Four patients (one frontal one suprasellar and two parietal) in the present series had focal neurological deficits and features of raised intracranial pressure was present in eight cases. Four patients had seizures. One patient of suprasellar cyst had headache and signs of chiasmal compression in form of blindness. Another patient of third ventricle cyst had hydrocephalus leading to papilloedema and diminution of vision. One patient with cyst in posterior fossa presented in emergency with history of unconsciousness for one day only. MR and CT scans characteristically show hydatid cyst as a spherical, well defined, non enhancing cystic lesion without peripheral edema [15, 16]. The fluid density is generally equal to that of CSF in both CT and MR scan. A fine rim of peripheral enhancement with perilesional edema may be seen in the presence of active inflammation [16]. MR scan may show a low density cyst wall [15] and relations with surrounding structures are better delineated than on CT scan. We could not identify scolices on CT or MR scan. In our series nine patients had CT scan and only one had MRI as our patients mostly belong to low socioeconomic group and in our setup, MRI costs much more than CT scan. Other reports on MR findings [13, 15] showed similar findings. Kohli et al., [17] performed in vivo and in vitro MR spectroscopy (MRS) studies in a patient of intracranial hydatid cyst. Besides lactate, alanine and acetate, a large resonance for pyruvate was observed. MRS pattern appeared different from the other cystic lesions of brain and they suggested MRS as an adjunct to imaging in the differential diagnosis of intracranial hydatid. Role of MRS in monitoring drug therapy was also highlighted. In none of our patients MRS was done as they belong to low income group.
Table 1: Details of patients and management
| Sl. No |
Age/sex |
Chief complaints |
Duration |
CT/MRI scan |
Treatment |
| 1 |
25/M |
Headache, convulsion,
Right hemiparesis
|
3 months |
Left frontal large
Single cyst
|
Excision by
hydrodissection
|
| 2 |
29/M |
Headache, convulsion,
Right hemiparesis
|
1 months |
Left parietal
Single cyst
|
Excision by
Traction and dissection
|
| 3 |
26/M |
Headache, convulsion,
Right hemiparesis |
1 year |
Right parietal
multiple cyst
|
Excision by
Traction and dissection
|
| 4 |
14/F |
focal convulsion
|
6 months |
Left parietal
Single cyst
|
Excision by
Traction and dissection
|
| 5 |
20/M |
Headache, diminution of vision |
1 months |
Third ventricle
Single cyst with
hydrocephalus
|
Endoscopic excision |
| 6 |
30/F |
Headache, diminution of vision |
1 months |
Suprasellar
Single cyst
|
Excision by
Traction and dissection
|
| 7 |
50/M |
Headache
|
8 months |
multiple
interhemispheric
cyst |
Excision by
Traction and dissection
|
| 8 |
6/M |
Headache, altered sensorium |
6 months |
Left frontal large
single cyst |
Excision by hydrodissection |
| 9 |
40/M |
Sudden unconsciousness |
1 day |
Multiple cysts
in frontal,
parietal and
posterior fossa |
Excision by
Traction and dissection
|
| 10 |
30/M |
Headache, vomiting, right hemiparesis |
2 months |
Multiple cysts in
parietal region |
Excision by
Traction and dissection
|
The treatment of hydatid cyst is surgical and the aim of surgery is to excise the cyst in toto without rupture to prevent recurrence and anaphylactic reaction. Various surgical options as summarized by Arana-Iniquez [18] include, puncture and aspiration of the cyst fluid through a small hole in the cyst wall, cortical incision over cyst and expulsion of hydatid cyst by insuffalation of air in the contra lateral ventricle and the most commonly done procedure designed to give birth to the intact cyst by irrigating saline between cyst wall-brain interface. This is possible because of minimal adhesions around the cyst wall. Our two patients of large frontal cyst were also operated by this technique. In seven cases excision of cyst were done by gentle dissection and traction. In our patient of intraventricular cyst excision was done endoscopically.
Conclusions
Intracranial Hydatid Cysts though rare but seen even in adults. This article is an attempt to create awareness of this condition for the early diagnosis of Hydatid cyst even in adult patients. A high index of suspicion and proper management can prevent life threatening consequences.
Conflict of interest
The authors declare that they have no competing interests.
Author’s Contribution
RSV: Concept and Analysis of cases study, Literature search and preparation of manuscript.
KS, VS: Concept and design of study.
References
[1]. Erşahin Y, Mutluer S, Güzelbağ E. Intracranial hydatid cysts in children. Neurosurgery 1993; 3: 219-224. [Pubmed]
[2]. Onal C, Barlas O, Orakdögen M, Hepgül K, Izgi N, Unal F. Three unusual cases of intracranial hydatid cysts in paediatric age group. Pediatr Neurosurg 1997; 26: 208-213. [Pubmed]
[3]. Dharker SR: Hydatid disease. In: Text Book of Neurosurgery,. Ramamurthi B, Tandon PN (Eds.). Second edition, Churchill Livingstone, New Delhi 1996; 535-544.
[4]. Jiménez-Mejías ME, Castillo-Ojeda E, Cuello Contreras JA, García Gutiérrez D, Romero Arce J, Pachón Díaz J. [Cerebral hydatidosis. Analysis of a series of 23 cases]. Med Clin (barc) 1991; 97: 125-132. [Pubmed]
[5]. Dharker SR, Dharker RS, Vaishya ND, Sharma ML, Chaurasia BD. Cerebral hydatid cysts in central India. Surg Neurol 1977; 8: 31-34. [Pubmed]
[6]. Balasubramanium V, Ramanujam PB, Ramamurthi B et al : Hydatid disease of the nervous system. Neurol India 1970; 18 : 92-95. [Pubmed]
[7]. Rivierez M, el-Azhari A, el Tantaoui M, Alaoui M. [Hydatid cyst of cavernous sinus: a case.] Neurochirurgie 1992; 38(1) : 46-49. [Pubmed]
[8]. Sinav S, Demirci A, Sinav B, Oge F, Sullu Y, Kandemir B. A primary intraocular hydatid cyst. Acta Ophthalmol 1991; 69: 802-804. [Pubmed]
[9]. Abbassioun K, Amirjamshidi A, Moinipoor MT: Hydatid cyst of the pons. Surg Neurol. 1986; 26(3):297-300. [Pubmed]
[10]. Mathuriya SN, Khosla VK, Kak VK et al: Multiple intracranial hydatid cysts - a case report. Neurol India 1987; 35: 163-168.
[11]. Sierra J, Oviedo J, Berthier M, Leiguarda R. Growth rate of secondary hydatid cysts of the brain. J Neurosurg 1985; 62: 781-782. [Pubmed]
[12]. Lunardi P, Missori P, Di Lorenzo N, Fortuna A. Cerebral hydatidosis in childhood: a retrospective survey with emphasis on long-term follow-up. Neurosurgery 1991; 29: 515-517. [Pubmed]
[13]. Nurchi G, Floris F, Montaldo C, Mastio F, Peltz T, Coraddu M. Multiple cerebral hydatid disease: case report with magnetic resonance imaging study. Neurosurgery 1992; 30: 436-438. [Pubmed]
[14]. Sharma A, Abraham J: Multiple giant hydatid cysts of the brain-case report. J Neurosurgery 1982; 57: 413-415. [Pubmed]
[15]. Coates R, Von Sinner W, Rahm B: MR imaging of an intracranial hydatid cyst. AJNR Am J Neuroradiol. 1990; 11: 1249-1250. [Pubmed]
[16]. Karak PK, Mittal M, Bhatia S, Mukhopadhyay S, Berry M. Isolated cerebral hydatid cyst with pathognomonic CT sign. Neuroradiology 1992; 34: 9-10. [Pubmed]
[17]. Kohli A, Gupta RK, Poptani H, Roy R. In vivo proton magnetic resonance spectroscopy in a case of intracranial hydatid cyst. Neurology 1995; 45: 562-564. [Pubmed]
[18]. Arana Iniquez R: Echinococcus. Infection of the Nervous System. In: Hand Book of Clinical Neurology, Part III, Vinken PJ, Bruyn GW, (Eds.) Elsevier/North Holland Biomedical Press, Amsterdam 1978; 175-208.

