Case Report

A Rare Presentation of Insulinoma as Postpartum Hypoglycaemia
1Kalyan Chakradhar, 2Randy Rajesh Sisodiya, 3 Mukhyaprana Prabhu, ,4, Raunak Maru
- 1Senior Resident, Department of general surgery Kasturba Medical College, Manipal
- 2Assistant Professor, Department of General Surgery Kasturba Medical College, Manipal
- 3Professor, Department of General Medicine Kasturba Medical College, Manipal
- 4Junior Resident, Department of General SurgeryKasturba Medical College, Manipal.
- Sunday, December 08, 2013
- Friday, January 24, 2014
- Saturday, February 08, 2014
This is an Open Access article distributed under the terms of
the Creative Commons Attribution License
(http://creativecommons.org/licenses/by/3.0)which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited
Abstract
Insulinomas are rare neuroendocrine tumors, being even rarer during pregnancy. Postpartum hypoglycemia is an uncommon presentation due to insulinoma. We present a case of 25 year old female who presented with complaints of sweating and drowsiness relieved by taking oral glucose. Patient had history of loss of consciousness five days after delivery. She was evaluated with necessary investigations but the cause could not be identified and hence treated symptomatically. She is suffering from similar complaints since 10 months whenever she skips a meal which were relieved by taking glucose. Patient was evaluated with supervised 72 hour fast during the present admission during which she developed neuroglycopenic symptoms after four hours of fasting, with low plasma glucose of 27mg/dl and inappropriately elevated levels of serum insulin 13.5 µU /ml. Failure of endogenous insulin secretion to be suppressed by hypoglycemia is the hallmark of an insulinoma .Magnetic resonance imaging of abdomen revealed a 1.5*1.9 cm mass in body of pancreas which was treated by enucleation with histopathology confirming insulinoma. Our case illustrates the importance of considering insulinoma as a cause of postpartum hypoglycemia.
Introduction
Pancreatic neuroendocrine tumors are rare tumors with an incidence of 1- 4 cases per million populations per year [1] but incidence of insulinoma in pregnancy is not known. Insulinoma are most common neuroendocrine tumors. Insulinomausually occur as sporadic tumors (80%) or as a part of a familial syndrome multiple endocrine neoplasia (MEN-1) (4-7%). In the sporadic form, the tumors are solitary and small (<2 cm in diameter). This makes localization often difficult. Approximately 10%
of insulinomas are malignant and multiple [2]. Patients with insulinoma have symptoms of hypoglycemia resulting from neuroglycopenia and increased catecholamine release The finding of inappropriately elevated levels of insulin in the face of hypoglycemia is the key to diagnosis. Diagnosis of insulinoma relies on clinical features along with laboratory tests and imaging investigations to aid in localization of tumor. Hypoglycemia in postpartum period can occur due to varied causes. We present a case of insulinoma in a 25 year old female who presented with neuroglycopenic symptoms in postpartum period. Our case shows usefulness of intraoperative ultrasound for localization of insulinomas and screening of rest of pancreas. Review of literature showed evidence of five cases of insulinomas manifesting as postpartum hypoglycaemia [3].
Case Report
A 25 years old female presented with an episode of loss of consciousness associated with diaphoresis, palpitation, tremulousness, relieved by taking glucose water orally. Patient had history of similar complaints since 10 months, when she had an episode of sweating, tremors, palpitation, associated with loss of consciousness five days after the delivery of her first child. She was treated with intravenous dextrose after which she regained consciousness. She was evaluated with necessary biochemical and contrast enhanced computed tomography of abdomen and no abnormality could be found. In the past 10 months patient had recurrent episodes of loss of consciousness associated with sweating, tremors whenever she skips a meal. No history of seizures, dyspnea, chest pain. Systemic inquiry revealed no other co morbid illness. She denied history of any prolonged drug intake or abuse. For further evaluation she was advised for hospitalization. On general examination she had 136 cm height, 46kg weight and BMI 24.6. With a working diagnosis of insulinoma, patient was evaluated.
Her hemogram, liver and renal and thyroid functional tests were normal. Patient was subjected to supervised 72 hour fast. She developed neuroglycopenic symptoms within 7 hours of fasting which was relieved by administration of intravenous dextrose. Her blood glucose was 27 mg/dl with insulin level of 13.5uU/ml with an insulin glucose ratio of 0.5. Fasting c peptide level was 2.4ng/ml with negative urinary sulfonyl urea.Patient was evaluated for the presence of the MEN-1 and no evidence for the same was seen.Patient’s serum calcium, parathyroid hormone and prolactin levels were normal.Magnetic resonance imaging (MRI) abdomen revealed 1.5x1.9 cm isodense small contour bulging lesion in proximal body of pancreas with rest of pancreas being normal [Figure I]. Finding was confirmed on EUS (endoultrasound).
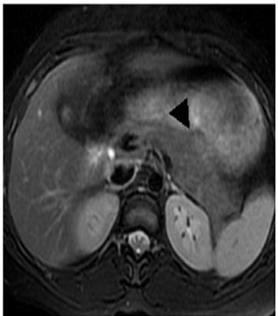
Figure 1: MRI Abdomen Showing 1.5x1.9 cm Isodense Small Contour Bulging Lesion
in Proximal Body of Pancreas
Patient underwent laparotomy.Intra- operative ultrasound showed a well-defined hyper-echoic rounded lesion in the head of the pancreas. Enucleation of 2x1.5 cm lesion found along the superior border of pancreas [Figure 2]

Figure 2: Intraoperative Photograph Showing 2*2 cm Insulinoma Arising from Superior Border
of Body of Pancreas
was done; rest of pancreas was screened by intraoperative ultrasound and was found to be normal. Postoperative period was uneventful and the patient did not suffer from any hypoglycemic episodes. Histopathology of the excised specimen was consistent with insulinoma with a mitotic figure of 2/10 [Figure 3] .
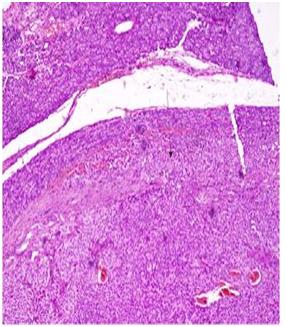
Figure 3: Histopathological Image Showing Insulinoma with Mitotic Figure of 2/10
Patient is on regular follow up and did not have any hypoglycemic episode in last 3 months.
Discussion
Insulinoma is characterized by Hyperinsulinaemichypoglycemia which presents as 1) neuroglycopenic symptoms; dizziness,diplopia, blurring of vision, amnesia, obtundation, irrationalbehaviour, seizures and coma and 2) adrenergic symptoms due to sympathetic-adrenal stimulation; anxiety, tremors, sweating, palpitation and hunger. The symptoms are classically precipitated by fasting; exertion missed meal and ameliorated by intake of sugars, sweets, fruits, and juices [4]. Whipple and Franz described a triad of clinical findings that were unique to patients with insulinoma: symptoms of hypoglycemia, a plasma glucose level of 45mg/dl (2.5 millimole /liter) or less when symptoms ofhypoglycemia occurred, and relief of symptoms with the administration of glucose [5]. Failure of endogenous insulin secretion suppression by hypoglycemia is the hallmark of an insulinoma. Thus, the finding of inappropriately elevated levels of insulin in the face of hypoglycemia is the key to diagnosis. Diagnosis depends on the exclusion of the more common causes of hypoglycemia (e.g. factitious insulin or sulphonylurea administration) and on the demonstration of raised plasma insulin and C-peptide levels in the presence of hypoglycemia [6].The biochemical diagnosis is established in 95% of patients during prolonged fasting (up to 72 hour) when the following parameters are found:
•Serum insulin levels of 10 µU/mL or more (normal < 6 µU/mL)</p>
•Glucose levels of less than 40 milligram/dL
•C-peptide levels exceeding 2.5 ng/mL (normal < 2 ng/mL)</p>
•Proinsulin levels greater than 25% (or up to 90%) that of immunoreactive insulin.
•Screening for sulfonylurea negative
•Most cases of insulinoma manifest during first trimester of pregnancy. Only five cases of post-partum insulinoma have been reported previously. Second and third trimesters of pregnancy are known to be an insulin resistance state due to placental counter-regulatory hormones like human placental lactogen, estrogen, progesterone, and increase in free cortisol levels3. These factors may have contributed to masking disease progression in later stages of pregnancy and patient presenting post-partum.
Dual-phase contrast spiral CT scan of abdomen is non-invasive study of choice. On CECT insulinomas are hyper vascular compared to the surrounding pancreas [7].Somatostatin receptor scintigraphy (SRS) or Octreoscan images tumors based on the density of type 2 somatostatin receptors. It is excellent and correctly identifies 90% of pancreatic neuroendocrine tumors. However, insulinomas are the exception, and they usually do not image on SRS [8].EUS is preoperative imaging study of choice and can identify tumors as small as 2 to 3 cm with sensitivity of 70% to 90%, and 100% specificity [9].Intra-arterial calcium stimulation with pancreatic venous sampling has recently emerged as a very sensitive and specific localization procedure [10].
Surgical excision is the treatment of choice and is curative in most cases.Enucleation is done for solitary insulinoma, especially if not abutting a main pancreatic ductor a major blood vessel while distal pancreatectomy with or without splenectomy is preferred for multiple insulinoma in the body and tail of the pancreas. Pancreatoduodenectomy (Whipple's procedure) for a non-enucleable insulinoma in the head and neck regions of the pancreas. Intraoperative palpation and intraoperative ultrasound are used to localize insulinomas which were not diagnosed preoperatively and to rule out multiple insulinomas.
Authors' Contribution
KC and RM are associated with conception and design, acquisition of data, analysis and interpretation of data. KC and MP are associated with drafting the article and revising it critically for important intellectual content.
RS has contributed to the final approval of version published
Conflict of Interests
The authors declare that there are no conflicts of interests
Ethical Considerations
Written informed consent was obtained from the patient for publication of this case report
Acknowledgement
None
Funding
None declared
References
[1]Dennis Vardakas, John Karoubalis, Theodora Pappa, George Piaditis and George N Zografos. Pancreatic insulinoma: current issues and trends.Hepatobiliary Pancreat Dis Int 2010; 9: 234-241.[Pubmed]
[2]Doherty GM, Toppan, Shawker TH, Miller DL, Eastman RC, Gorden P, Norton JA.Results of a prospective strategy to diagnose, localize, and resect insulinomas. Surgery. 1991; 110(6):989-96.[Pubmed]
[3]Rodrigues Queiróz AJ, Nazareno LS, Miranda JE, de Azevedo AE, Teixeira da Cruz CA, Pirani Carneiro F, Florêncio da Costa AC etal. Insulinoma diagnosed in the postpartum: clinical and immune histochemical features. Gynecol Endocrinol. 2012 Aug; 28(8):633-6[Pubmed]
[4]Paul TV, Jacob JJ, Vasan SK, Thomas N, Rajarathnam S, Selvan B, Paul MJ etal. Management of insulinomas: analysis from a tertiary care referral center in India. World J Surg. 2008; 32(4): 576-82.[Pubmed]
[5]. Whipple AO, FranzVK .Adenoma of islet cells with hyperinsulinism. AmSurg 101:1299–1335.[Pubmed]
[6]Svartberg J, Stridsberg M, Wilander E, Andersson DEH, Eriksson B. Tumor-induced hypoglycemia in a patient with insulin-dependent diabetes mellitus. J Intern Med. 1996; 239: 181–5[Pubmed]
[7]Fraker DL, Norton JA.Localization and resection of insulinomas and gastrinomas. JAMA.1988; 259(24):3601-05.[Pubmed]
[8]Lamberts SW, Hofland LJ, van Koetsveld PM, Reubi JC, Bruining HA, Bakker WH, Krenning EP. Parallel in vivo and in vitro detection of functional somatostatin receptors in human endocrine pancreatic tumors: consequences with regard to diagnosis, localization, and therapy.J Clin Endocrinol Metab. 1990; 71(3):566-74.[Pubmed]
[9]Rösch T, Lightdale CJ, Botet JF, Boyce GA, Sivak MV, Jr, Yasuda K, Heyder N et al. Localization of pancreatic endocrine tumors by endoscopic ultrasonography. N Engl J Med. 1992 Jun 25; 326(26):1721–1726.[Pubmed]
[10]Yao MM, Reynertson RH. Insulinoma: a case report and review of the clinical features and Diagnosis. Gundersen Lutheran Medical Journal 2005; 3: 73-6.

