Case Report

Symptomatic Colonic Mucocele in an Adult Patient with Imperforate Anus
1Nathalie Mantilla,3Jennifer Blumetti,2Marc Singer,3Herand Abcarian.,
- 1Department of Surgery, University of Illinois at Chicago Medical Center, 840 S Wood St. Suite 376-CSN. Chicago, IL 60612.
- 2 Departments of Colon & Rectal Surgery, Highland Park Hospital. 777 Park Avenue West. Highland Park, IL 60035.
- 3Departments of Colon &Rectal Surgery, Stroger Hospital of Cook County. 1900 W Polk St. Room 406. Chicago, IL. 60612.
- Submitted: Tuesday, June 24, 2014
- Accepted: Friday, July 25, 2014
- Published: Sunday, November 16, 2014
This is an Open Access article distributed under the terms of the Creative Commons Attribution License ((http://creativecommons.org/licenses/by/3.0)which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited
Abstract
Background
Mucocele is a rarely encountered complication in the lower gastrointestinal tract. It has been most commonly described in the appendix however, it is also known to occur in the colon. The case of woman with a symptomatic mucocele 20 years after an ileostomy for imperforate anus is detailed.
Case Presentation
A 20 year old woman presented with one week history of crampy abdominal pain and progressive abdominal distention. The patient has significant medical and surgical history having been born a conjoined twin with multiple congenital anomalies including imperforate anus for which she had an ileostomy and mucus fistula. The output from the mucus fistula had gradually decreased over time. On physical examination her abdomen was much distended but non tender to palpation. She had a functioning ileostomy with a mucus fistula. No perineal opening was present. A CT scan identified large fluid filled bowel loops in the pelvis. A small bowel follow-through and fistulogram were performed, revealing a markedly stenotic area of either colon or small bowel approximately 15 cm in length, with an area of post stenotic dilatation, and ending in a blind pouch. Malrotation of small bowel was also identified. At exploratory laparotomy, an extremely dilated colon was found with stenotic terminal ileum. The colon was filled with copious amounts of yellow mucus. The terminal ileum and cecum were resected, and the ascending colon was brought to the abdominal wall as a new mucus fistula.
Conclusions
Colonic mucocele is a rare entity with few case reports in the literature. The majority of these cases are due to sequestration of mucosal islands after resection.
Keywords
Mucocele, Obstruction, Colon, Congenital Malformation.
Introduction
Mucocele of the lower gastrointestinal tract is a rare complication which has most commonly been described in the appendix [1 2 3]. In the colon and rectum mucocele occurs even less commonly, and has been described after repair of imperforate anus [4], pull-through for Hirschsprungs disease [5] proctectomy and ileal pouch anal anastomosis [1], and colon resection. [6]. In these cases, the mucocele formation was felt to be due to retained islands of mucosa; rarely does a colonic mucocele develop as a stoma complication resulting in closed loop obstruction [7 8]. In this case, we report a symptomatic mucocele which occurred 20 years after stoma formation in a patient with imperforate anus.
Case Presentation
The patient is a 20 year old female who presented with one week history of progressive abdominal distention and cramping abdominal pain. She denied nausea, vomiting or changes in bowel habits. Her past medical history was significant for being a former conjoined twin with multiple congenital anomalies, including pelvic bony malformation, single kidney, bladder malformation, malrotation and imperforate anus. She had renal failure and was undergoing dialysis. Her surgical history included separation from her twin, ileostomy and mucus fistula formation, and bladder reconstruction. The imperforate anus was never repaired, although her colon was left in place for the possibility of future repair. According to the patient, she had irrigated the mucus fistula as a child, but had stopped several years ago. She noted that the output from the mucus fistula had decreased over time, especially during the week prior to presentation, and she noted that her cramping abdominal pain improved with output from the mucus fistula.
On physical examination she was a thin woman in mild distress. She had marked scoliosis of her thoracic spine. Her abdomen was very distended, but non tender to palpation. She had extensive scarring from her previous surgeries, and had a functioning right sided ileostomy with an inferomedially placed mucus fistula. She also had evidence of imperforate anus with no perineal fistula visualized (Figure 1).

Figure 1: Perineum with imperforate anus.
Abdominal X ray demonstrated deformities of the pelvic bones and opacity in the pelvis. CT scan showed large fluid filled bowel loops in the pelvis (Figure 2). Small bowel follow-through and fistulogram were performed. Malrotation and normal caliber small bowel were identified on the follow-through (Figure 3A) On the fistulogram, a markedly stenotic area of either colon or small bowel was identified, approximately 15 cm in length, with an area of post stenotic dilatation, and ending in a blind pouch(Figure 3B).

Figure 2: Pelvic CT showing the dialatation
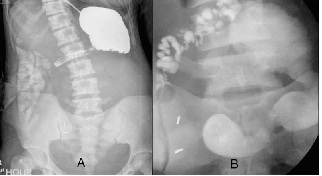
Figure 3: Small bowel follow through (A) and fistulogram through mucus fistula (B).
Exploratory laparotomy revealed extremely dilated colon, with stenotic terminal ileum(Figure 4).The colon was filled with copious amounts of yellow mucus. Resection was performed of the terminal ileum and cecum, and an ascending colon mucus fistula was created. Pathology revealed focal luminal stricture with colitis and congestion, with fibrosis of the lamina propria.

Figure 4: Pathology specimen. Note strictured ileum with dilated cecum
The postoperative course was uneventful. She was instructed to irrigate the mucus fistula weekly, and will plan for definitive repair of her imperforate anus vs. total proctocolectomy in the future.
Discussion
Mucocele of the lower gastrointestinal tract is a rare entity, most commonly described in the appendix, where it occurs in 0.2 to 0.3% of all appendectomy specimens [3]. It occurs due to longstanding obstruction of the lumen, with resultant slow accumulation of mucus [1 8], and in the case of the appendix, can be associated with neoplastic changes in the appendix or elsewhere [1 3]. In the colon and rectum, this entity occurs even less commonly, with rare case reports describing mucocele formation after colon resection [5] after repair of imperforate anus [4] after pull through foHirschsprungs disease [5] and after ileal pouch anal anastomosis for Ulcerative colitis [1] These all occurred due to retained islands of mucosa. Mucocele can also occur, as it did in this case presentation, as a result of a closed loop obstruction of defunctionalized colon secondary to a stoma complication
In 1974, Nicosia and Abcarian described a patient who developed a colonic mucocele after perineal trauma [7]. The patient had undergone end colostomy with mucus fistula 30 years prior to development of the mucocele. The mucocele developed when the patients mucus fistula stenosed, creating a closed loop obstruction. Witte [8] described a similar case in 1989 in a patient with longstanding ulcerative colitis and loop transverse colostomy. A distal rectal stricture combined with stenosis of the distal limb of the colostomy resulted in a closed loop obstruction. A significant finding in both these and our case was a decrease in drainage from the defunctionalized limb, which occurred for some time prior to diagnosis.
Although mucocele of the colon as a stoma complication is extremely unusual, the type of stoma created influences its formation, especially in children with anorectal malformations. The majority of these children, as in our patient, require a stoma prior to definitive repair. The type and site of colostomy is extremely important to prevent complications, which can occur in 28-74% of children [9]. Loop stomas will typically not completely divert the fecal stream, and can lead to distal fecal impaction and urinary contamination if a urinary tract malformation or fistula is also present. A colostomy and mucus fistula positioned too close together can result in the same scenario if required to be covered by one stoma appliance. For many surgeons, a descending colostomy with mucus fistula is the procedure of choice [10 12]. It is proximal enough to allow adequate length of colon distally to perform the repair, and has a decreased tendency to prolapse compared to sigmoid or transverse colostomies [10 12].
Transverse colostomies have a higher morbidity and an increased tendency to form mucoceles in children, especially in patients in whom there is a long time interval to definitive surgery. Pena [10] described a characteristic finding of microcolon at the level of the mucus fistula with dilation distally in patients with right transverse colostomy; this resulted in worse clinical outcomes after definitive repair. Despite the importance of proper stoma placement in these children, some surgeons are still creating stomas other than left sided colostomies. Pena found that 29.5% of 1470 stomas created were located in sites other than the sigmoid or descending colon, including 35 ileostomies. He determined that 46% (282 of 616) of stomas created at other institutions were misplaced. In addition there were 62 children who underwent Hartmans procedure, which can result in mucocele if the patient has a narrow or absent perineal fistula, creating a closed loop obstruction [10].
The diagnosis of colorectal mucocele requires a high index of suspicion. In a patient with a longstanding stoma, decrease in drainage of a defunctionalized limb may be the only sign. Similar to appendiceal mucoceles, abdominal pain and increase in abdominal girth may be described [12 3,4 5 7 8]. Treatment of the mucocele must be individualized for each patient. In the case reports by Nicosia and Witte, resection of the colon and rectum with permanent stoma was performed. In this case given the patient’s young age and the possibility of future repair of her imperforate anus, segmental resection and creation of a new mucus fistula was performed.
Conclusion
Colonic mucocele is a rare entity with few case reports in the literature. The majority of these cases are due to sequestration of mucosal islands after resection. However, it can occur as the result of a closed loop obstruction resulting from stoma complication.
Authors Contribution
NM, BJ, SM, and AH: Substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data, Drafting the article or revising it critically for important intellectual content.
All authors read and approved the final manuscript.
Conflict of Interests
The authors declare that there are no conflicts of interest.
Ethical Considerations
Written informed consent was obtained from patient for publication of this case report.
Funding
None declared
Acknowledgement
None
References
[1].Heise CP, Gopal D, Harms BA. Novel Presentation of ileal pouch mucocele. Surgery 2005; 138:100-102
[Pubmed]
[2].Stocchi L, Wolff BG, Larson DR, Harrington JR. Surgical Treatment of Appendiceal Mucocele. Archives of Surgery 2003; 138:585-590
[Pubmed]
[3].Pitiakoudis M, Tsaroucha AK, Mimidis K, Polychronidis A, Minopoulos G, Simopoulos C. Mucocele of the Appendix: a report of five cases. Tech Coloproctol 2004; 8:109-112
[Pubmed]
[4].Panicek DM, Leeson SH, Hitch DC, Farrar FM. Perirectal Mucocele after imperforate anus repair. Pediatr Radiol 1987; 17: 73-74
[Pubmed]
[5].Hitch DC, Patil UB, Panicek DM. Mucocele after endorectal pull-through for Imperforate Anus. Journal of Pediatric Surgery 1987; 22: 1023-1024
[Pubmed]
[6].Haber MM, Leon ME, BAkker JE, Nagle D. Carcinoembryonic antigen elevation due to bowel sequestration with mucocele formation following colonic resection. Arch Pathol Lab Med 2003;127:1376-1379[Pubmed]
[7].Nicosia JF, Abcarian H. Mucocele of the distal colonic segment, a late sequela of trauma to the perineum: report of a case. Diseases of the Colon and Rectum 1974;17:536-539
[Pubmed]
[8].Witte JT, Harms BA. Giant colonic mucocele after diversion colostomy for ulcerative colitis. Surgery 1989;106:571-574[Pubmed]
[9].Chandaramouli B, Srinivasan K, Jagdish S, Ananthakrishnan N. Morbidity and Mortality of Colostomy and its closure in Children. Journal of Pediatric Surgery 2004;39:596-599
[Pubmed]
[10].Pena A, Migotto-Krieger M, Levitt MA. Colostomy in anorectal malformations: a procedure with serious but preventable complications. Journal of Pediatric Surgery 2006;41:748-756
[Pubmed]
[11].Levitt MA, Pena A. Outcomes from the correction of anorectal malformations. Curr Opin Pediatr 2005;17:394-401
[12].Patwardhan N, Kiely EM, Drake DP, Spitz L, Pierro A. Colostomy for anorectal anomalies: High incidence of complications. Journal of Pediatric Surgery 2001;36:795-798[Pubmed]

