Original Article

Prevalence of Postcholecystectomy Symptoms: Long Term Outcome after Open versus Laparoscopic Cholecystectomy
*Somendra Bansal, *Sanchit Jain, *Ram Naresh Daga,*Kailash Chand Vyas
- Submitted: Friday, January 03, 2014
- Accepted: ;Saturday, February 08, 2014
- Published:Monday, March 17, 2014
This is an Open Access article distributed under the terms of the Creative Commons Attribution License ((http://creativecommons.org/licenses/by/3.0)which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited
Abstract
Objectives
After cholecystectomy, a certain number of patients continue to suffer from abdominal symptoms or develop such symptoms postoperatively. The aim of this study was to compare the prevalence of postcholecystectomy symptoms (PCSs) between open and laparoscopic cholecystectomy and to find out and investigate the cause of PCSs.
Material and Methods
This study was conducted in MB Government Hospital, Udaipur on 100 patients undergoing open or laparoscopic cholecystectomy for symptomatic cholelithiasis. Preoperative and postoperative symptoms of 50 Patients (37 females), aged 20 to 79 years, who underwent open cholecystectomy, were prospectively compared questionnaire with those of 50 patients (39 females) aged 16 to 75 years, who underwent laparoscopic cholecystectomy. Patients were followed up for an average of 11 to 12 months.
Results
There was no statistically significant difference in prevalence of postcholecystectomy symptoms after open cholecystectomy compared with laparoscopic cholecystectomy (26% v/s 14%, P = 0.134).
Conclusions
There is no significant difference in prevalence of post-cholecystectomy symptoms after open cholecystectomy compared with laparoscopic cholecystectomy.
Introduction
Cholecystectomy is the gold standard for treatment of cholelithiasis and for biliary pain and other gall bladder diseases. Many patients, however, are dissatisfied with the procedure because of lack of improvement or relapse of symptoms initially attributed to the presence of gallstones or because of the emergence of new gastrointestinal complaints presumably related to the operation. These so called postcholecystectomy syndromes [1] range from mild ill defined digestive symptoms to severe attacks of abdominal pain and jaundice.
Causes of symptoms after cholecystectomy may be divided into four categories: first, common bile duct stones may have been overlooked [2]. Second, other gastrointestinal conditions such as gastroesophageal reflux, peptic ulcer disease and functional dysmotility disorders may have coexisted and their symptoms erroneously attributed to gallstones. Third, loss of reservoir function of the gall bladder has been shown to result in a number of adverse changes: impairment of the antropyloric motor unit [3], increased duodenogastric reflux [4], increased gastroesophageal reflux [5] and a reduced bile salt pool which may result in subclinical fat malabsorption and diarrhea [6]. Finally, the abdominal wound may result in pain from nerve damage or the development of an incisional hernia.
Persistent symptoms after cholecystectomy occur in upto 40% of patients [1]. Although most of these complain of mild and transient symptoms, severe pain persists as a long-term complaint in upto 10%. With the introduction of laparoscopic cholecystectomy one could expect a decrease of the prevalence of PCSs owing to advantages of minimally invasive techniques causing fewer adhesions and scar related problems. However, one could look for an increase of PCSs due to the more liberal indication for cholecystectomy performed for functional disorders or for symptoms caused by undiagnosed stenosis of the papilla formerly detected intraoperatively by combined pressure and flow measurements [7]. Few studies have compared the late results of laparoscopic cholecystectomy with those of open cholecystectomy [7,9,12].
The goal of present study was to compare the data from a single institution regarding prevalence of PCSs in prospective study after open and laparoscopic cholecystectomy.
Patients and Methods
This study was conducted between 1st January 2008 to 31st December 2009. We compared two groups of patients which were comparable in terms of demographic data, in terms of preoperative symptomatology [Table 1,2].
| Parameter |
Open group
(Open cholecystectomy
|
Lap group
(Laparoscopic cholecystectomy)
|
| (i) No. of patients |
50 |
50 |
| (ii) Follow up times (Months) |
12 (3 - 5) |
11 (3 - 15) |
| (iii) Female/Male |
2.8 (37 : 13) |
3.5 (39 : 11) |
| (iv) Age (years) |
46 (20 - 79) |
45 (16 - 75) |
The first (“open”) group consisted of 50 patients who underwent open cholecystectomy which was done through a right subcostal incision. Patients with common bile duct exploration or other additional procedures were excluded. The second (“lap”) group consisted of 50 patients who underwent laparoscopic cholecystectomy. Conversion to open cholecystectomies were excluded from this study.
Patients with choledocholithiasis, acute cholecystitis and Gall bladder mass were excluded in both groups. In both groups only those patients were included who could be followed up. All those patients, who were lost/could not be followed up, excluded from this study.
Patients in both groups were interviewed preoperatively about their history and asked to give a detailed description of their symptoms using a standard questionnaire. The various diagnostic investigations were done. The follow up of both groups were done by personal interview using a standard symptom questionnaire. Pain and symptoms were quantified using the visick classification [10]. Visick-I: no symptoms, Visick-II: minor symptoms without interference with daily activities, Visick-III: symptoms not relieved by care, influencing daily activities and ability to work and Visick-IV: symptoms not improved, relapse.
All symptoms that occurred during follow up were taken into account regardless of whether they occurred intercurrently or had been successfully treated. Patients having PCSs were investigated to find out cause. For statistical analysis we used the Chi-square test and t-test.
Result
Preoperative symptoms and diagnosis
Most common symptom was pain in right upper quadrant / epigastric area in both groups. Other symptoms such as nausea and vomiting, flatulent dyspepsia, fever and jaundice were almost equally distributed in both groups (Table 2). Diagnostic procedures performed including liver function, ultrasound, Magnetic Resonance Cholangiopancreatography (MRCP).
|
Symptoms
|
Open
cholecystectomy (OC) group (n=50)
|
Laparoscopic
cholecystectomy (LC)
group
(n=50)
|
|
|
|
No. of cases
|
%
|
No. of cases
|
%
|
|
(1)
|
Pain
|
|
|
|
|
|
|
- No pain
|
4
|
8.0
|
2
|
4.0
|
|
|
- Pain in right upper
|
46
|
92.0
|
48
|
96.0
|
|
|
quadrant / epigastric area
|
|
|
|
|
|
(2)
|
Character of pain
|
|
|
|
|
|
|
- Colicky
|
36
|
72.0
|
40
|
80.0
|
|
|
- Constant
|
10
|
20.0
|
8
|
16.0
|
|
(3)
|
Other symptoms
|
|
|
|
|
|
|
- Nausea and vomiting
|
22
|
44.0
|
26
|
52.0
|
|
|
- Flatulent dyspepsia
|
20
|
40.0
|
18
|
36.0
|
|
|
- Fever
|
7
|
14.0
|
3
|
6.0
|
|
|
- Jaundice
|
2
|
4.0
|
3
|
6.0
|
|
(4)
|
Multiple symptoms
|
32
|
64.0
|
33
|
66.0
|
Long term results
In both group all patients were followed up for an average of 11 to 12 months.(Table 3). The difference in prevalence of postcholecystectomy symptoms for the two groups was not significant (P = 0.134). Prevalence of PCSs in “open” group was 26% as compared to 14% in “lap” group. 74% of patients in “open” group could be classified as having visick score of I compared to 86% in “lap” group. Visick score II applied to 20% of the “open” group and 10% of the “lap” group. Visick score III was found in 4% in “open” group and 2% in “lap” group. Visick score IV was found in 2% of the patients in both groups. (Figure 1).
|
Follow up signs and
symptoms after chollecystectomy
|
Open
cholecystectomy(OC) group (n=50)
|
Laparoscopic
cholecystectomy(Lc) group (n=50)
|
P value
|
|
No. of
cases
|
%
|
No. of
cases
|
%
|
|
Pain (right upper
quadrant epigastric area)
|
8
|
16.0
|
2
|
4.0
|
0.038
|
|
Flatulent dyspepsia
|
8
|
16.0
|
6
|
12.0
|
0.193
|
|
Nausea & vomiting
|
1
|
2.0
|
1
|
2.0
|
1.000
|
|
Jaundice
|
1
|
2.0
|
-
|
-
|
0.315
|
|
Scar pain
|
6
|
12.0
|
1
|
2.0
|
0.050
|
|
Incisional hernia
|
1
|
2.0
|
-
|
-
|
0.315
|
|
Retained CBD stone
|
-
|
-
|
1
|
2.0
|
0.315
|
|
Cholangitis
|
-
|
-
|
-
|
-
|
-
|
|
Pancreatitis
|
1
|
2.0
|
-
|
-
|
0.315
|
|
Gastritis
|
2
|
4.0
|
1
|
2.0
|
0.558
|
|
CBD stricture
|
1
|
2.0
|
-
|
-
|
0.315
|
|
Port site parietal
abscess
|
-
|
-
|
1
|
2.0
|
0.315
|
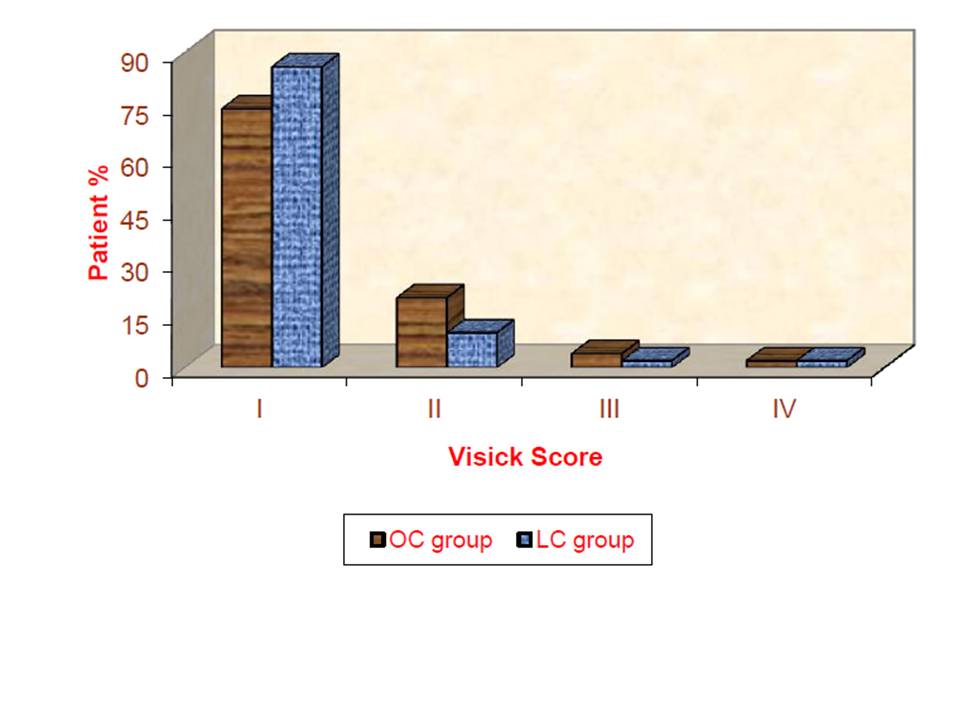
Fig.1: Symptomatic outcome after cholecystectomy. Visick classification for long term outcome after open or laparoscopic cholecystectomy. Visick-I: no symptoms, Visick-II: minor symptoms without interference with daily activities, Visick-III: symptoms not relieved by care, influencing daily activities and ability to work, Visick-IV: symptoms not improved, relapse
Flatulent dyspepsia was most common symptom in both groups (16% in “open” group and 12% in “lap” group, P = 0.193). Pain in right upper quadrant was present in 16% in “open” group and 4% in “lap” group with statistically significant difference (P = 0.038). Patients mentioned scar related pain more often in the “open” group than in the “lap” group (12% vs. 2%; P = .050).
All symptomatic patients, regardless of whether they were treated successfully during the follow up period, remained classified by their primary Visick score.
Incisional hernia occurred in one patient who had open cholecystectomy but there was no port site hernia in the laparoscopy group. Retained common bile duct (CBD) stones occur in 2% cases after laparoscopic cholecystectomy. For retained CBD stones, Endoscopic Retrograde Cholangiopancreatography (ERCP) was done but it was unsuccessful and later on choledochoduodenostomy was done. 2% cases developed each CBD stricture and pancreatitis in open group and 2% cases developed port site parietal abscess in lap group. ERCP was done for CBD stricture but stricture could not be negotiated, so hepaticojejunostomy was done. Port site parietal abscess was diagnosed by Computed Tomography (CT) scan. Incidence of PCSs was more common in younger age females in both group. Incidence of PCSs increased with increase in duration of preoperative symptoms in both groups.
We did not observe a significant difference in prevalence of PCSs between open and laparoscopic cholecystectomy. One year post-operatively, 94% of patients after open and 96% after laparoscopic cholecystectomy had no or only minor symptoms. In most retrospective series that compared the symptomatic outcome after open and laparoscopic cholecystectomy, there has been no difference [7,8,9,12,13]. Thus the prevalence of PCSs did not change with introduction of minimally invasive technique. This is explained by the fact that gall stones are the cause of patient‟s symptoms, which are eliminated regardless of difference in access [7].
After open cholecystectomy, patients with typical gall stone related symptoms pre-operatively (i.e. colicky pain in the right upper quadrant or epigastric area for a duration of hours) had a better long-term outcome than patients with other abdominal symptoms preoperatively [14], whereas the outcome after laparoscopic cholecystectomy was not influenced by any single symptom or combination of preoperative symptoms [15].
Coliky pain was better relieved than constant pain [8], and more intense symptoms better than mild preoperative ones [13], and there does not seem to be a difference between open and laparoscopic cholecystectomy. Functional disorders can also be „cured‟ by cholecystectomy. Therefore the expectation of some patients that cholecystectomy will relieve dyspeptic symptoms appear to be realistic, but the relief is unpredictable [16]. Symptomatic patients mostly had functioning gall bladders preoperatively and longer duration of symptoms prior to cholecystectomy [17].
Reduction in right upper quadrant pain after laparoscopic cholecystectomy together with lack of any difference in prevalence of mild gastrointestinal symptoms (such as indigestion and heartburn) between two groups suggest that factors associated with operative procedures may be responsible at least in part for the difference in symptoms in the both groups [18]. Stiff et al. reported that significantly fewer patients complained of right upper quadrant pain after laparoscopic cholecystectomy than after conventional surgery (3% v/s 10% P<0.05) and postulated that intercostal nerve. might be damaged by subcostal wound which may lead to neuroma formation. Other potential explanations include a reduction in intra-operational adhesions or the placebo effect of surgery [18]. According to Peterli et al. [15] the aetiologies of the postcholecystectomy syndrome after laparoscopic cholecystectomy were: residual stones (1%), subhepatic fluid formation (0.8%), incisional hernia (0.4%), peptic disease (4%), wound pain (2.4%) and functional disorders (26%). Schoenemann et al. [19] found that functional disorders were the most common cause of PCSs. In this study, flatulent dyspepsia persisted in 23.7% cases who had a complained of flatulent dyspepsia before operation and 8.0% cases who had no complaint of flatulence before operation. Flatulent dyspepsia was most common symptom after cholecystectomy in both groups. Bates et al. [20] found that commonest persisting symptoms, 12 months after cholecystectomy was excessive flatulence (47%), indigestion (46%). Scar related problems are more common in open group as compared to lap group [7,21]. In Stiff et al. [18] study found 1.3% incidence of incisional hernia after open cholecystectomy as compared to 0% after laparoscopic cholecystectomy. Port site abscess formation due to a dropped non-opaque gallstone is an unusual complication of laparoscopic cholecystectomy in which diagnosis was suggested with combination of ultrasound and computed tomography findings and confirmed by surgery [22]. One case of port site parietal abscess was present after lap cholecystectomy in this study which was diagnosed by CT scan but no calculus or foreign body was found in abscess cavity.
All symptoms were more common in women than in men and after operation flatulence was the most severe symptoms [23]. Bodvall and Overgaard [11] reported that younger women had more PCSs and patients with longer preoperative history had also more frequency of PCSs and this was confirmed in the present study.
In conclusion, there was no significant difference in prevalence of post-cholecystectomy symptoms after open cholecystectomy compared with laparoscopic cholecystectomy.
Authors’ Contributions
SB and SJ carried out the literature search and prepared the draft manuscript, SB carried out the experiments and interpreted the results, RND and KCV designed the study and performed the analysis, SB and SJ conceived the study, participated in design and edited the final manuscript. All authors have read and approve the final manuscript for submission.
Conflict of Interests
The authors declare that there are no conflicts of interests.
Ethical Considerations
The study was approved by the Institute Ethics Committee.
Funding
None Declared
Acknowledgements
None
References
[1].Bodvall B. The postcholecystectomy syndromes. Clin. Gastroenterol 1973; 2: 103-06[pubmed]
[2].Ruddell WS, Lintott DJ, Ashton MG, Axon AT. Endoscopic retrograde cholangiography and pancreatography in investigation of postcholescystectomy patients. Lancet 1980; i:444-7[[pubmed]
[3].Johnson AG. Pyrolic function and gallstone dyspepsia. Br J Surg 1972; 59:449-54.[[pubmed]
[4].[Brown TH, Walton G, Cheadle WG, Larson GM. The alkaline shift in gastric pH after cholecystectomy. Am J Surg 1989; 157:58-65[[pubmed]
[5].Jazrawi S, Walsh TN, Byrne PJ, et al. Cholecystectomy and oesophageal reflux: a postoperative evaluation. Br J Surg 1993; 80:50-3.[[pubmed]
[6][Thaysen EH, Pedersen L. Idiopathic bile acid catharsis. Gut 1976; 17: 965-70[[pubmed]
[7].Peterli R, Schuppisser JP, Herzog U, Ackermann C, Tondelli PE. Prevalence of postcholecystectomy symptoms: Long-term outcome after open versus laparoscopic cholecystectomy. World J Surg 2000; 24:232-1235[pubmed]
[8].Vander Velpen GC, Shimi SM, Cuschieri A. Outcome after cholecystectomy for symptomatic gall stone disease and effect of surgical access: laparoscopic versus open approach. Gut 1993; 34(10): 1448-51.[pubmed]
[9].Kane RL, Lurie N, Borbas C, Morris N, Flood S, McLaughling B, Nemanich G, SchultzThe outcomes of elective laparoscopic and open cholecystectomies. J Am Coll Surg 1995; 180:136.[pubmed]
[10].Visick AH, A study of the failures after gastrectomy. Ann R Coll Surg Engl 1948; 3: 266.[pubmed]
[11][Bodvall B, Overgaard B. Computer analysis of postcholecystectomy biliary tract symptoms. Surg Gynecol Obstet 1967; 124: 723-32[pubmed]
[12].Wilson RG, Macintyre IM. Symptomatic outcome after laparoscopic cholecystectomy. Br J Surg 1993; 80, 439-41[pubmed]
[13].McMahon AJ, Ross S, Baxter JN, Russell IT, Anderson JR, Morran CG, Sunderland GT, Galloway DJ, O‟Dwyer PJ. Symptomatic outcome one year after laparoscopic and minilaprotomy cholecystectomy: a randomized trial. Br J Surg 1995; 82:1378-82[pubmed]
[14].Konsten J, Gouma DJ, von Meyenfeldt MF, Menheere P. Long-term follow up after open cholecystectomy. Br J Surg 1993; 80, 100-102[pubmed]
[15][.Peterli R, Merki L, Schuppisser JP, Ackermann C, Herzog U, Tondelli P. Postcholecystectomy complaints one year after laparoscopic cholecystectomy. Results of a prospective study of 253 patients. Chirurg 1998 Jan; 69 (1): 55-60[pubmed]
[16].Bates T, Ebbs SR, Harrison M, A‟Hern RP. Influence of cholecystectomy on symptoms.Br J Surg 1991; 78, 964-967[pubmed]
[17].Anand AC, Sharma R, Kapur BM, Tandon RK, Analysis of symptomatic patients after cholecystectomy: is the term postcholecystectomy syndrome an anachronism? Trop Gastroenterol 1995 Apr-Jun; 16 (2): 126-31[pubmed]
[18].Stiff G, Rhodes M, Kelly A, Telford K, Armstrong CP, Rees BI. Long-term pain: less common after laparoscopic than open cholecystectomy. Br J Surg 1994; 81:1368-1370[pubmed]
[19].Schoenemann J, Zeidler J. Sequelae of cholecystectomy. Z Gastroenterol Feb 1997; 35(2):139-45[pubmed]
[20].Bates T, Mercer JC, Harrison M. Symptomatic gallstone disease before and after cholecystectomy. Gut 1984; 25:579-80.
[21].Muhe E. Long term follow up after laparoscopic cholecystectomy. Endoscopy 1992; 24:754-8[pubmed]
[22][.Akyar G, Aytac S, Yagci C. Abscess formation due to dropped gallstone after laparoscopic cholecystectomy. Eur J Radiol Nov 1997; 25(3):242-5.[pubmed]
[23].Ure BM, Troidl H, Spangenberger W, Lefering R, Dietrich A, Eypasch EP, Neugebauer E. Long-term results after laparoscopic cholecystectomy. Br J Surg 1995; 82, 267-270[pubmed]

