Research

Post traumatic Diaphragmatic hernia in children: Diagnostic Dilemmas and lessons learned.
1 Vaibhav Pandey, 1 Pranay Panigrahi, 1Rakesh Kumar, 2Vivek Srivastav
- 1 1Department of Paediatric Surgery, Institute of Medical Sciences, Banaras Hindu University, Varanasi, U.P., India
- 2 2Department of General Surgery, RML, Lucknow, India
- Submitted:Saturday, September 2, 2017
- Accepted: Thursday, November 23, 2017
- Published: Sunday, December 3, 2017
This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited
Abstract
Introduction:
Acquired diaphragmatic hernias are rare, life-threatening clinical conditions occurring after an abrupt increase of intra-abdominal pressure. We present our experience with post traumatic diaphragmatic hernia in children following blunt abdominal trauma.
Material and methods :
This retrospective study was conducted in the Department of Paediatric surgery and Level I pediatric trauma centre of northern India. All the patients with suspected diaphragmatic hernia following blunt abdominal trauma admitted in the department of paediatric surgery and trauma centre between April 2011 and March 2017 were included in the study. The case records were used to collect the data.
Results :
Total seven cases of were suspected to have post traumatic diaphragmatic hernia out of 142 patients managed during the study period. Out of these, three were cases of congenital asymptomatic eventration of diaphragm. Four cases were of post traumatic diaphragmatic hernia, three on left side and one on right side. Mode of injury was fall from height in all cases with a mean age of 4.54±1.44 years. All cases hemodynamically stable had abdominal distension and respiratory distress at time of presentation. Contrast enhanced computed tomography showed, diaphragmatic defect in all the patients. All four patients were operated after initial resuscitation.
Conclusion:
Acquired diaphragmatic hernia is a rare entity in children following blunt abdominal trauma and a very high index of suspicion should be there to rule out congenital asymptomatic eventration of diaphragm in order to avoid unnecessary laparotomies.
Key words:
abdominal trauma, liver atrophy, Post traumatic diaphragmatic hernia, right diaphragmatic hernia
Introduction:
Blunt trauma is a leading cause of death during childhood [1]. Solid organ injury and gastrointestinal perforations are the main complications of blunt abdominal trauma (BAT). Acquired diaphragmatic hernias are rare, life-threatening clinical conditions occurring after an abrupt increase in intra-abdominal pressure [1-3]. Blunt trauma abdomen accounts 2-7 % of these cases and 10–15% cases are a result of penetrating trauma [4-5]. Left sided hernia is more common as on the right side liver acts both as protector to the diaphragm and as a barrier to herniation. The right to left ratio has been reported to be about 1:15 in different reports [3]. We present our experience with post traumatic diaphragmatic hernia in children following blunt abdominal trauma.
Material and methods:
This retrospective study was conducted in the Department of Paediatric surgery and Level I pediatric trauma centre of northern India. After ethical approval, all the patients with suspected diaphragmatic hernia following blunt abdominal trauma admitted to the Department of paediatric surgery and Trauma centre between April 2011 and March 2017 were included in the study. The case records were used to collect the data about the demographics, mechanism of injury, hemodynamic status, physical examination findings, Glasgow Coma Score, laboratory values, radiologic imaging, number of associated injuries, management, and the outcome.
Results:
Total 142 patients with blunt abdominal trauma were admitted during the study period. Out of these, seven patients were suspected to have post traumatic diaphragmatic hernia at the time of admission on the basis of abdominal and chest radiographs. Later on, three were found to have associated incidental left sided eventration of the diaphragm which was asymptomatic previously (2 diagnosed with the help of previous radiographs and one intra-operatively) (Figure 1). Rest four cases were of post traumatic diaphragmatic hernia, three on left side and one on right side. Mode of injury was fall from height in all cases with a median age of 4 years (3-15 years). All four cases were hemodynamically stable at the time of presentation. Three children were males and two were females. One child presented with respiratory distress, 13 years after blunt abdominal trauma (sustained at age of 2 years) managed at our department. The chest radiograph showed right sided diaphragmatic hernia. The previous radiograph of the patient was normal. CT thorax confirmed the diagnosis with a right hemi-diaphragm defect Figure 2). So, a diagnosis of post traumatic diaphragmatic hernia was made. Rest three children presented after a mean time of 3.23±2.24 (range 2-6 days) following trauma (Table 1). All the patients had abdominal distension and respiratory distress at the time of presentation. Contrast enhanced computed tomography showed, a diaphragmatic defect in all the patients.
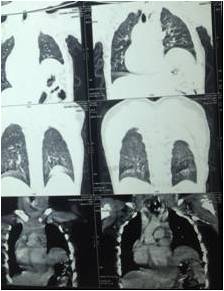

Fig 1: CT thorax showing left sided incidental eventration

Fig 2: CT thorax right sided hemithorax showing diaphragmatic hernia
Table 1: Demography of cases with post traumatic diaphragmatic hernia.
| Variable |
Value |
| Median age |
4 years (3-15 years). |
| Male: Female |
3:1 |
| Associated injury |
75% (Spleenic laceration and liver laceration) |
| Mean time of presentation after injury |
3.23±2.24 (Range 2-6 days) |
| Right : Left diaphragmatic defect |
1:3 |
All four patients were operated after initial resuscitation. The child with delayed presentation had atrophy of right lobe of liver and hypertrophy of left lobe with a defect of size 5x3 cm in right hemidiaphragm through which all the abdominal contents were herniating into right hemithorax (Figure 3&4). Repair was performed using non-absorbable interrupted sutures. Post operative period was uneventful in all. Out of three patients with eventration, one was operated (diagnosed intraoperatively). A placation of diaphragm was performed. Rest two cases with eventration were successfully followed without any intervention.

Fig 3: Intra-operative picture showing right sideddiaphragmatic defect

Fig 4: Repaired defect of diaphragm with atrophied right lobe of liver.
Discussion:
Sennertus in 1541 described Diaphragmatic rupture complicated by intra-thoracic herniation of an abdominal organ following an autopsy. He found a defect in diaphragm from which colon has herniated and got strangulated [4-5]. Isolated blunt traumatic diaphragmatic rupture is rare with an incidence of 0.8 – 5% [6]. Right sided diaphragmatic hernias are less common compared to the left side and it presents with nonspecific clinical and radiological findings making prompt diagnosis challenging [4]. The silent presentation and high morbidity and mortality rates associated with delayed diagnosis of cases make this clinical entity more important [7]. Usually, they are often not detected early leading to severe complications associated with high mortality rates [4-6]. In our series, all the cases were diagnosed early (except one case) and we had no mortality. We hypothesize that child with delayed presentation may have sustained damage to right hepatic vessels which caused gradual atrophy of right lobe. Further, there was either an immediate or delayed rupture of right diaphragm. This resulted in a gradual herniation of bowel and atrophied right lobe of liver into the thoracic cavity. Delayed rupture of the diaphragm may occur due to gradual devitalization of muscles of the diaphragm due to injury. This process may take hours to days [2-4]. Clinical presentation varies. Left sided herniation is more common and usually presents early than their right sided counterparts. The liver on right side acts as barrier and results in delayed herniation and late presentation [3-4]. Usually, at the time of injury there are no symptoms related to diaphragmatic rupture, patients have complaints are related to associated abdominal trauma. The duration of presentation may vary depending upon the time of herniation of viscus into thorax leading to further symptoms. Delayed presentation occurs as a recurrent cough and respiratory tract infection [8]. The early recognition of blunt traumatic diaphragmatic rupture usually depends on a high index of suspicion and Chest radiography represents the basic investigation for the diagnosis [8-9]. Computed tomography thorax and abdomen is most sensitive and specific for detection of hernia and associated complications.
In children, associated eventration may be misdiagnosed as a diaphragmatic hernia. Such cases until previously symptomatic due to diaphragmatic eventration (recurrent pneumonitis and respiratory distress), should be managed expectantly. A high index of suspicion is required to diagnose these patients to avoid unnecessary laparotomies. As one of the largest tertiary pediatric trauma care facility in northern India, we have been managing these cases in a volume much larger than most of the centers in our country. As incidental congenital eventration does not require any treatment, and we in spite of our large experience have missed this and operated such patients, the high index of suspicion of asymptomatic eventration in children cannot be overlooked. Surgical repair of the diaphragmatic defect can be performed through a trans-thoracic or trans-abdominal approach [4]. The use of interrupted or continuous non-absorbable suturing along with the intra-thoracic placement of chest tubes represents the classical strategy [4-5].
Conclusion:
An acquired diaphragmatic hernia is a rare entity in children following blunt abdominal trauma. Right sided defect are still rarer and past history o trauma may give a clue for the diagnosis.
A very high index of suspicion should be there to rule out congenital asymptomatic eventration of the diaphragm in order to avoid unnecessary laparotomies.
Acknowledgement:
We acknowledge Prof AN Gangopadhyay for conceptualization of this manuscript.
Conflict of Interest:
No conflicts of interest.
Authors Contribution
All authors contributed equally in preparation of manuscript
Ethical considerations
The study was approved by the Institute Ethics Committee
References
[1].Grosfeld JL, Rescorla FJ, West KW, Vane DW. Gastrointestinal injuries in childhood: analysis of 53 patients. J Pediatr Surg. 1989; 24:580–583. PMID: 2738826 [PubMed]
[2].Baek SJ, Kim J, Lee SH. Hepatothorax due to a right diaphragmatic rup- ture related to duodenal ulcer perforation. World Journal of Gastroenterology 2012;18:5649–52. PMID: 23112562 PMCID: PMC3482656 [PubMed] [PMC]
[3.Meyers BF, McCabe CJ. Traumatic diaphragmatic hernia. Occult marker of serious injury. Annals of Surgery 1993;218:783–90. PMID: 8257229 PMCID: PMC1243075 [PubMed][PMC]
[4].Rashid F, Chakrabarty MM, Singh R, Iftikhar SY. A review on delayed presentation of diaphragmatic rupture. World Journal of Emergency Surgery 2009;4:32. PMID: 19698091 PMCID: PMC2739847 [PubMed][PMC]
[5].Goh BK, Wong AS, Tay KH, Hoe MN. Delayed presentation of a patient with a ruptured diaphragm complicated by gastric incarceration and perforation after apparently minor blunt trauma. CJEM 2004; 6: 277–80. PMID: 17382006 [PubMed]
[6].Schumpelick V, Steinau G, Schluper I, Prescher A. Surgical embryology and anatomy of the diaphragm with surgical applications. Surg Clin North Am 2000;80:213-39. PMID: 10685150 [PubMed]
[7].Disler DG, Deluca SA. Traumatic rupture of the diaphragm and herniation of the liver. Am Fam Physician 1992;46:453–6. PMID: 1636561 [PubMed]
[8].Shetty P, Selvaraju K. A rare case of isolated blunt traumatic diaphragmatic rupture. Webmedcentral Gastrointestinal 2010;1:Wmc001183. http://www.webmedcentral.com/wmcpdf/Article_WMC001183.pdf
[9].McCann B, O’Gara A. Tension viscerothorax: an important differential for tension pneumothorax. Emerg Med J 2005;22:220-21. PMID: 15735278 PMCID: PMC1726701 [PubMed] [PMC]

