Case Report

Tumorlets, an Incidental Finding in a Dual Pulmonary Lesion; a Pathologist’s Curiosity
*Cicy Joseph, *Lekshmi Padmanabhanan,*V Letha, Renu Thambi,*,Sansho Ulahannan* Usha Poothiode ,
- *Pathology, Govt. Medical College Kottayam, Kerala, Kottayam, India
- Submitted:Thursday, November 06, 2014
- Accepted: Sunday, November 30, 2014
- Published: Monday, December 08, 2014
This is an Open Access article distributed under the terms of the Creative Commons Attribution License ((http://creativecommons.org/licenses/by/3.0)which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited
Abstract
Tumorlets are collections of neuroendocrine cells seen in the lungs.They may be incidentally detected and are usually seen associated with chronic lung diseases like bronchiectasis, bronchial asthma and sequestration.It is important to identify tumorlets especially in patients with prior history of carcinoma breast,since theymimic metastatic disease.
Our patient was a 49 year lady who presented with cough and dyspnea of 6 months duration. Radiology revealed a large cavitatary lesion occupying the entire lower lobe of right lung. A lobectomy was done and gross examination revealed a large cavity with thickened wall, bronchioles were also thickened and reached up to the pleural surface. Histology confirmed the diagnosis of bronchiectasis with cavity formation. Adjacent lung showed granulomatous reaction but there was no caseation necrosis. One of the sections had a minute (1mm) focus showing
a group of cells with neuroendocrine features. Further bits were taken and sections studied revealed a tumorlet of 4mm size. So a final diagnosis of bronchiectactic cavity with granulomatous reaction and tumorlet formation was made. We report this case because of its rarity.
Key words
bronchiectasis, granulomatous reaction, tumorlets
Introduction
Proliferation of neuroendocrine cells (PNC) may be seen as nodules or diffusely, in the lung. PNCs which are less than 5mms are called tumorlets and when larger they are called carcinoids [1, 2]. When seen closely associated with bronchial or bronchiolar epithelium,they are called Diffuse Idiopathic Pulmonary Neuroendocrine Cell Hyperplasia (DIPNECH) [2]. The main difference between DIPNECH and tumorlets is that the latter is always seen extraluminally, i.e., in the lung parenchyma.Tumorlets may be seen in many chronic fibrosing lung diseases and whether they cause fibrosis and inflammation or occur as a response to it is a matter of debate.However more weightage is given to the former concept [3, 4].
Case report
49 year old lady presented with complaints of cough and dyspnea of 6 months duration.There was no significant past history.On examination tachypnea and cyanosis were present.Systemic examination revealed decreased breath sounds on the right side of chest and occasional crepts were present.Routine blood investigations showed an ESR of 60mm/1st hr.Chest X-ray showed hypertranslucency in the right lower lobe.Computerized tomography revealed a large bulla occupying almost the entire lower lobe of right lung (Figure1a). Right lobectomy was done and the postoperative period was uneventful.
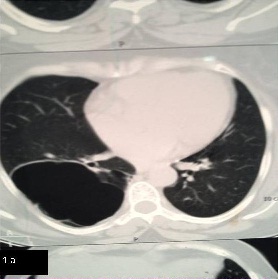
Figure 1 A): Computerized tomography scan showing a large bulla
occupying almost the entire lower lobe of right lung.
Gross examination showed a large irregular cavity measuring 7cm in diameter in the right lower lobe (Figure 1b).Wall was thickened, trabeculated, irregular and shaggy without any granular or necrotic material in the lumen.Adjacent areas of fibrosis were seen and the bronchioles were thickened and could be tracedup to the pleural surface.

Figure 1 B) Gross examination showed a large irregular cavity measuring 7cm
in diameter in the right lower lobe
Microscopic examination revealedchronic inflammation with formation of lymphoid follicles and granulomatous reaction with necrosis(Figure 1c & Figure 1d).
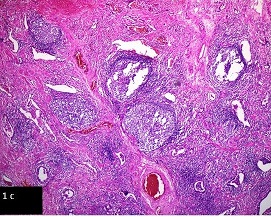
Figure 1 C) photomicrograph showing chronic inflammation and formation of
lymphoid follicles in lung parenchyma, H & E x 100.
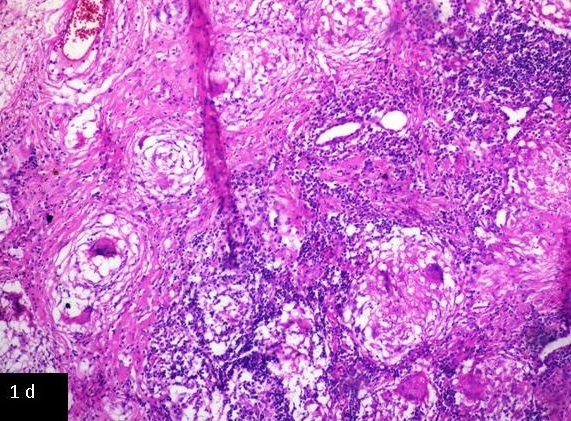
Figure 1 D) photomicrograph showing granulomatous reaction with necrosis, H & E x 200
The bronchioles were dilated and showed thickened walls.Initial sections showed a minute focus of neuroendocrine cells.Further sections revealed a 4mm sized collection of neuroendocrine cells(Figure 2a & Figure 2b).
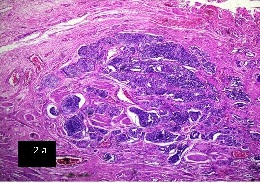
Figure 2A: Photomicrographs showing microscopy showing a collection of
neuroendocrine cells, H & E x 100
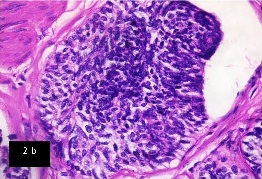
Figure 2B: Photomicrographs showing higher magnification of the same, H & E
x 400
These cells were seen extraluminally and showed a positive reaction with chromograninand synaptophysin on immunohistochemistry (Figure 2c & Figure 2d).Thus we gave a diagnosis of bronchiectactic cavity with granulomatous reaction and tumorlet formation.GMS and AFB stains were negative. Our patient is healthy and on follow up since 18 months.
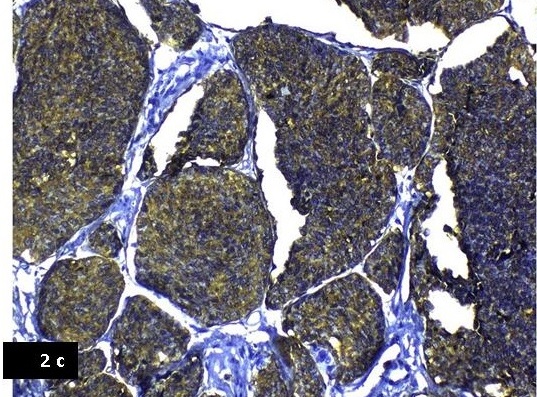
Figure 2C: Photomicrographs showing immunohistochemistry showing positive reaction for chromogranin,
200X.
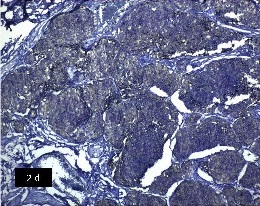
Figure 2D: Photomicrographs showing immunohistochemistryshowing positive reaction for synaptophysin, 100X
Discussion
Tumorlet is a nodular proliferation of neuroendocrine cells which arises from focal areas of bronchial and bronchiolar kultschitsky cells, usually associated with diffuse bronchiectasis and intralobar sequestration [5, 9]. They may also be found in otherwise normal lungs,though they are usually detected incidentally in lungs scarred by chronic pulmonary diseases [3, 4]. They are less than 5 mm in size, often peripheral in location,multiple and characterized by small nests of cells with neurosecretory granules[1]. Typically,they have a hyalinized, fibroelasticstroma [9]. They lack cellular atypia and mitosis and are thought to be benign [3]. But D’Agati and Perzin found that pulmonary tumor-lets had tumor characteristics since they could metastasize to the lymph nodes [9, 10].
Some authors consider tumorlets to represent tiny peripheral pulmonary carcinoids that differ mainly in size from the larger carcinoid tumors with which they share histological, ultra-structural, and immunohistochemical features [4]. Chromogranin A, CD56 and synaptophysin are the most useful neuroendocrine immunohistochemical markers and low levels of Ki-67 can help to distinguish them from small-cell carcinoma [5, 11].
Ultrastructurally the cells of tumorlets closely resemble those forming neuroepithelial bodies and typical carcinoid tumors [7, 9and 12].
Tumorlets are different from DIPNECHs.Sonological findings in DIPNECH are mosaic attenuation due to air trapping, whereas tumorlets are seen as subcentimetricnodules [1, 13]. Significant airflow obstruction is usually not attributed to tumorlets unlikeDIPNECHS whichare thought to be associated with airflow limitation [14]. Histopathologic findings of tumorlets are as nests located extraluminaly in the lung parenchyma,while presence of an intact basement membrane,intraluminal location and diffuse distribution favors DIPNECH[1, 13,14]. Regarding the behavior, tumorlets are thought to be benign and most do not evolve to carcinoids[3]. But DIPNECHs are thought to be pre neoplastic [11, 14]..
The significance of recognizing these neuroendocrine cell proliferations in the lung are because they closely mimic metastatic disease especially in patients with a prior history of breast cancer, when seen as multiple nodules [3, 14].Another microscopic differential is Minute Meningothelial-Like Nodule (Chemodectoma) which is seen as a localized proliferation of round to oval cells with eosinophilic cytoplasm. However they are devoid of endocrine granules and are similar to meningothelial cells.But they also show an association with chronic lung disease.
Tumorlets may be associated with many chronic lung diseases and are known to show a female preponderance [3, 14]. High altitude and smoking are also thought to be associated with the occurrence of tumorlets.Patients may have persistent disease but long term survival is thought to be excellent [ 14]
Conclusions
This case highlights the importance of careful observation of gross specimens and liberal sectioning from areas of suspicion. A proper diagnosis can avoid unnecessary therapy especially in cases where it mimics metastatic disease. Due to the varied categorizationsby different authors, a definite idea regarding the exact nature of such neuroendocrine cell proliferations still remains somewhat elusive.
Authors' Contribution
CJ: did pathological reporting, prepared and drafted the
article
LP: design, preparation and drafting of manuscript
VL: design,
preparation and drafting of manuscript
RT: review and editing of manuscript
SU: did literature search, design and editing of final manuscript.
UP: review
and editing of manuscript
All authors read and approved the final version.
Conflict of Interests
The authors declare that there are no conflicts of interests.
Ethical Considerations
Written informed consent for publication of this case report was obtained from the patient.
Funding
None declared
Acknowledgement
None
References
[1].Koo CW, Baliff JP, Torigian DA, Litzky LA, Gefter WB, and Akers SR: Spectrum of pulmonary neuroendocrine cell proliferation: diffuse idiopathic pulmonary neuroendocrine cell hyperplasia, tumorlet, and carcinoids. Am J Roentgenol.2010; 195(3):661–8[Pubmed]
[2].Gosney JR. Diffuse idiopathic pulmonary neuroendocrine cell hyperplasia as a precursor to pulmonary neuroendocrine tumors. Chest. 2004; 125(5 suppl): 108S.
[Pubmed]
[3]Ginsberg MS, Akin O, Berger DM, Zakowski MF, Panicek DM. Pulmonary Tumorlets: CT Findings Am J Roentgenol. 2004; 183(2):293-6
[Pubmed]
[4].He P, Gu X, Wu Q, Lin Y, Gu Y, He J.Pulmonary carcinoid tumorlet without underlying lung disease: analysis of its relationship to fibrosis. J Thorac Dis. 2012;4(6):655–8
[Pubmed]
[5].Ye Y, Mu Z, Wu D, Xie Y. Carcinoid tumorlet in pulmonary sequestration with bronchiectasis after breast cancer: A case report.Oncol lett. 2013:5:1546-48
[Pubmed]
[6].Dewan M, Malatani TS, Osinowo O, al-Nour M, Zahrani ME: Carcinoid tumourlets associated with diffuse bronchiectasis and intralobar sequestration. J R Soc Promot Health.2000;120(3):192–5.[Pubmed]
[7].Churg A, Warnock ML. Pulmonary tumorlet. A form of peripheral carcinoid. Cancer.1976; 37:1469–77
[Pubmed]
[8].Ranchod M: The histogenesis and development of pulmonary tumorlets. Cancer 1977; 39:1135–45.
[Pubmed]
[9].GosneyJ, Green AR, Taylor W. Appropriate and inappropriate neuroendocrine products in pulmonary tumourlets. Thorax 1990; 45:679-83
[Pubmed]
[10].D’Agati VD, Perzin KH. Carcinoid tumorlets of the lung with metastasis to a peribronchial lymph node. Report of a case and review of the literature. Cancer.1985; 55:2472–6.[Pubmed]
[11].Travis WD: Advances in neuroendocrine lung tumors. Ann Oncol.2010; 21(Suppl 7): vii65–71
[Pubmed]
[12].Bonikos DS, Archibald R, Bensch KG. On the origin of the so-called tumorlets of the lung. Hum Pathol 1976; 7:461-9.
[Pubmed]
[13].Gorshtein A, Gross DJ, Barak D, Strenov Y, Refaeli Y, Shimon I et al.Diffuse idiopathic pulmonary neuroendocrine cell hyperplasia and the associated lung neuroendocrine tumors.Clinical experience with a rare entity .Cancer 2012; 118(3):612–19
[Pubmed]
[14].Aubry MC, Thomas CF Jr, Jett JR,
Swensen SJ, Myers JL. Significance of multiple carcinoid tumors and tumorlets in
surgical lung specimens: analysis of 28 patients. Chest 2007; 131:1635-43. [Pubmed]

